Freely Available British and Irish Public Legal Information
[Home] [Databases] [World Law] [Multidatabase Search] [Help] [Feedback]
England and Wales High Court (Queen's Bench Division) Decisions
You are here: BAILII >> Databases >> England and Wales High Court (Queen's Bench Division) Decisions >> Taylor v Chesterfield Royal Hospital Nhs Foundation Trust [2019] EWHC 1043 (QB) (02 May 2019)
URL: http://www.bailii.org/ew/cases/EWHC/QB/2019/1048.html
Cite as: [2019] EWHC 1043 (QB)
[New search] [Printable PDF version] [Help]
Neutral Citation Number: [2019] EWHC 1048 (QB)
Case No: HQ16C03583
IN THE HIGH COURT OF JUSTICE
QUEEN'S BENCH DIVISION
Royal Courts of Justice
Strand, London, WC2A 2LL
Date: 30/04/2019
Before :
John Kimbell QC
(sitting as a Deputy High Court Judge)
- - - - - - - - - - - - - - - - - - - - -
Between :
|
|
REBECCAH TAYLOR |
Claimant |
|
|
- and - |
|
|
|
CHESTERFIELD ROYAL HOSPITAL NHS FOUNDATION TRUST |
Defendant |
- - - - - - - - - - - - - - - - - - - - -
- - - - - - - - - - - - - - - - - - - - -
Christopher Kemp (instructed by Tozers LLP ) for the Claimant
Farrah D. Mauladad (instructed by Weightmans LLP ) for the Defendant
Hearing dates: 4, 5, 6 and 7 February 2019
- - - - - - - - - - - - - - - - - - - - -
APPROVED JUDGMENT
John Kimbell QC sitting as Deputy High Court Judge:
INTRODUCTION
1. The Claimant is 26 years old. She was born at Royal Chesterfield Hospital (‘ the Hospital ’) on 13 November 1992. On that day she suffered a brachial plexus injury which she alleges was the result of negligence on the part of the two midwives and/or the registrar who attended her birth.
2. The brachial plexus is a network of nerves which emerge from the neck region of the spine. It conducts signals from the brain to the muscles of the shoulder and forearm. If these nerves are stretched beyond a certain point, they can rupture. If the damage is significant, it can lead to a permanent paralysis of the arm usually referred to as Erb’s (or Erb-Duchenne) palsy.
3. The Claimant is the second of four children. Her older brother, Oliver, was born in December 1990. Her younger brother, Harry, followed in October 1995 and younger sister, Holly, in 1999. Her parents are Deborah Taylor and Christopher Taylor. They are clearly a close, supportive and loving family.
4. Rebeccah was delivered at 20:35 by Dr Dobbs, a registrar. He had been summoned by the two midwives who had been in attendance up that point, Mrs Julie Rawson and Student Midwife Godfrey. They summoned Dr Dobbs because the delivery of Rebeccah’s body had not followed the delivery of her head in the usual way, i.e. with the next contraction. The reason for the interruption in delivery was that Rebeccah’s anterior (left) shoulder had become lodged underneath her mother’s pubic bone in a condition referred to as shoulder dystocia.
5. The entry in the agreed delivery notes signed by Dr Dobbs states:
“ Shoulder dystocia – [head] delivered
episiotomy cut + ant. shoulder del.
[with] suprapubic pressure + traction”.
6. It was noted immediately after her birth that Rebeccah’s left arm was floppy. It was thought that she might have suffered a fractured clavicle. An x-ray revealed that there was in fact no fracture but Rebeccah was subsequently diagnosed as having a Group 2 obstetric brachial plexus injury (‘ OPBI ’). The categorisation referred to is that developed by Gilbert and Tassin and described by Narakas in the table below: [1]
|
Group |
Roots injured |
Site of weakness / paralysis |
Likely Outcome |
|
1 |
C5, C6 |
Shoulder abduction/external rotation, elbow flexion |
Good spontaneous recovery in over 80% of cases |
|
2 |
C5, C6, C7 |
As above but with drop wrist |
Good spontaneous recovery in about 60% of cases |
|
3 |
C5, C6, C7, C8, T1 |
The whole plexus has been damaged. Complete flaccid paralysis |
Recovery in 30%-50% of cases |
|
4 |
C5, C6, C7, C8, T1 |
Complete flaccid paralysis with Horner Syndrome |
Without surgery severe defects throughout the limb. Full spontaneous recovery never occurs |
7. In Rebeccah’s case a spontaneous recovery has not occurred. She has not undergone any surgery and the loss of range of movement in her left arm is significant. This affects her daily life in a number of ways. She suffers back and shoulder pain. Notwithstanding all the challenges presented by her birth injury, she has thrived. She achieved bronze, silver and gold swimming medals at school and participated fully in dance and PE lessons as well as skiing trips. She took A-levels and obtained a graphic design degree from Manchester University. She has travelled and worked abroad.
8. Rebeccah’s parents did not bring a claim against the Hospital on her behalf while she was a child. However, whilst at university, Rebeccah began to research her birth injury and in 2013 she obtained a legal aid certificate to pay for legal advice. A letter of claim followed in July 2014 and a claim form was issued on 17 October 2016.
9. No limitation defence was pleaded by the Defendant.
THE PLEADED CASE
10. In summary, the Claimant alleges that her brachial plexus injury was caused by the negligent application of excessive traction to her head by the attending midwives and/or the registrar after shoulder dystocia had been correctly diagnosed by the midwives. The Defendant denies liability on the basis that the procedures in place and the steps taken in response to Rebeccah’s shoulder dystocia were in accordance with practices accepted as proper by a responsible body of medical people in 1992.
11. There were originally six pleaded breaches of duty, namely:
(a) Attempting to apply suprapubic pressure while Mrs Taylor remained in the left lateral position.
(b) Failing to move Mrs Taylor into the dorsal position before applying suprapubic pressure.
(c) Failing to alter the maternal position after the attempt to deliver in the left lateral position as a manoeuvre to overcome the shoulder dystocia.
(d) Either by the midwives or Dr Dobbs applying excessive traction to the Claimant’s head in an attempt to deliver her shoulders.
(e) Either by the midwives or Dr Dobbs applying more than diagnostic traction to the Claimant’s head in an attempt to deliver her shoulders.
(f) Either by the midwives or Dr Dobbs applying traction to the Claimant’s head such as to damage permanently her (left) brachial plexus.
12. However, in the course of the trial, the first three allegations set out above were abandoned. The case thus becomes a case about traction.
QUANTUM
13. Quantum was agreed in the sum of £1,150,000.
MEDICAL FACTUAL BACKGROUND
14. Mrs Taylor’s due date was 2 November 1992. On 8 November 1992, Mrs Taylor was admitted to the Hospital’s Labour Suite with a suspected spontaneous rupture of membranes and occasional uterine tightening. Following a medical review, Mrs Taylor was allowed to go home with an antenatal clinic appointment.
15. On 12 November 1992, Mrs Taylor attended her final antenatal assessment. By now, she was 10 days past her due date. It was noted that Rebeccah was a “big baby”. A vaginal examination was performed and Mrs Taylor’s cervix was found to be 2cm dilated. It was noted that Mrs Taylor was “anxious” and had requested induction of labour. Mrs Taylor was admitted at 18.40. The admitting midwife noted that Mrs Taylor had “anxiety re size of baby & method of induction”.
16. Mrs Taylor was assessed at 06.00 on 13 November. She had slept very little overnight because of discomfort. On vaginal examination her cervix was slightly posterior but fully effaced and 3-4cm dilated. The baby’s head was presenting. Mrs Taylor was transferred to the Hospital’s Central Delivery Suite at 08.00.
17. At 10.30 a vaginal examination was carried out to rupture the membranes. The cervix was 4cm dilated. Clear liquor was draining but Mrs Taylor was only contracting irregularly.
18. At 13.45 Mrs Taylor’s contractions were recorded as being irregular and mild to moderate only. Therefore, a plan was made to commence the use of syntocinon to stimulate uterine activity.
19. At 14.00 Mrs Taylor’s care was taken over by student midwife Godfrey and Mrs Rawson.
20. At 14.45 a syntocinon infusion was started.
21. At 17.40 a vaginal examination was performed. Mrs Taylor’s cervix was found to be 6cm dilated and the forewaters were found to be intact. These were ruptured, releasing clear fluid. The lack of progress of cervical dilatation was noted, with a plan to reassess in two hours. The foetal heart showed a good trace.
22. At 19.30 Mrs Taylor is recorded as saying that she was feeling “pushy” . The partogram records strong contractions every 2 minutes at this point.
23. At 20. 00 a vaginal examination was performed. The cervix was fully dilated with strong contractions every 2 minutes.
24. At 20.10 active pushing is recorded as having commenced.
25. At 20.30 an entry made by student midwife Godfrey recorded the “controlled delivery of head”. The timing of this entry was subsequently changed to “20.32 approx” by Mrs Rawson. The explanation for this change was explored in cross-examination.
26. Rebeccah was born at 20.35. She weighed 4.93 Kgs (10 lb 14 oz). Mrs Taylor needed 40 stiches to repair extensive second-degree tears.
27. What happened between the delivery of Rebeccah’s head at 20.30 (or approximately 20.32) and the rest of her body between 3 and 5 mins later is in dispute.
Mrs Rawson’s note
28. A significant portion of the trial was spent exploring the following note in the Medical Records made by Mrs Rawson:
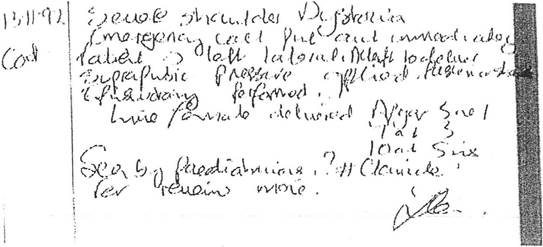
29. In her evidence Mrs Rawson said she thought she would have written this note at the end of her shift (at around 21.00) on 13 November 1992. I accept that evidence. It was eventually agreed that this note was to be read as follows with numbers in [ ] to indicate line numbers.
[1] Severe shoulder Dystocia
[2] Emergency call put out immediately
[3] Patient → left lateral. Attempt to deliver posterior shoulder
[4]Suprapubic pressure applied
[5]Episiotomy performed.
[6] Live female delivered Apgar 5 at 1
[7] 7 at 3
[8] I O at 5 mins.
[9] Seen by paediatricians. ?[fracture] clavicle
[10] for review mane.
[Signature of Mrs Rawson]
30. There was originally a dispute about when the words “ Attempt to deliver posterior shoulder” were added. However, Mrs Rawson explained in evidence, and it was accepted by Mr Kemp on behalf of the Claimant in his closing submissions, that these words were added at the same time as the rest of the notes were written (i.e. at the end of her shift that evening) but after the words “ Suprapubic pressure applied” had already been written down. They were inserted midway along line [3] and continuing into [4] in order to indicate to any reader that the step took place after Mrs Taylor was put on her left side but before any suprapubic pressure was applied.
31. It was common ground that at 20:30 when Rebeccah’s head was delivered, there were only four people in the delivery room: Student Midwife Godfrey, Mrs Rawson, Mr Taylor and Mrs Taylor. Dr Dobbs and some other (unidentified) staff entered the room only after an alarm was sounded at 20.32.
THE LAW
32. The legal principles applicable to medical negligence cases in general are not in dispute. They derive from Bolam -v- Friern Hospital Management Committee [1957] 1 W.L.R. as confirmed by the House of Lords in Maynard -v- West Midlands Regional Health Authority [1984] 1 W.L.R. 634.
33. It is common ground that the qualification to the Bolam test introduced by Bolitho -v- City and Hackney Health Authority [1998] AC 232 pursuant to which an act done in accordance with a respectable body of professional opinion can still lead to a finding of negligence if that body of opinion has no logical basis is not engaged in this case.
34. The relevant principles in the context of a claim of this type have recently been succinctly summarised by Haddon-Cave J. (as he then was) in Sardar v NHS Commissioning Board [2014] EWHC 38 (QB) at [25] in the form of four propositions, which I gratefully adopt:
(1) The test to be applied is the standard of the ordinary skilled man or woman exercising and professing to have that special skill.
(2) It is sufficient if he or she exercises the ordinary skill of an ordinary competent person exercising that particular art.
(3) He or she is not negligent if he or she has acted in accordance with a practice accepted as proper by a responsible body of medical people skilled in that particular art.
(4) The standard by which the individual doctor, nurse or midwife is to be judged is the standard of a reasonably competent doctor, nurse or midwife carrying out the functions expected of him or her in the delivery suite of a general district hospital.
35. It is common ground that the standard by which the actions of Dr Dobbs and the midwives are to be judged are those which prevailed in 1992.
THE FACTUAL WITNESS EVIDENCE
36. I heard evidence from three factual witnesses: Mrs Taylor and Mr Taylor (for the Claimant) and Mrs Rawson (for the Defendant). A witness summary was served in relation to Mr Dobbs. I will return to the status of this evidence below.
37. With the agreement of counsel, I also read the witness statements served on behalf of the Claimant in support of the quantum part of the case.
Mrs Taylor
38. Mrs Taylor is 56 years old. She is a graduate in Business Studies from Bristol University. Before studying for this degree, she trained as a nurse. She worked for a year and a half at a children’s hospital. She now runs an animal care business.
39. Mrs Taylor has very strong memories of what happened during Rebeccah’s birth. It was not suggested to her in cross-examination or in closing submissions to me that she was making up any of her evidence to assist her daughter’s claim. Her witness statement was short and to the point. It contained only what she could actually remember. She gave oral evidence and responded to questions put to her in cross-examination in a composed and measured manner. She did not seek to embellish her evidence or claim to remember further details, such as the emergency bell sounding, which she could easily have done without being effectively challenged. I found her an entirely credible witness.
Mr Taylor
40. Mr Taylor was until last year a director of a family retail butchery business based in Rotherham. He began working at the age of 16. He was at his wife’s side throughout the delivery of Rebeccah. He also had firm memories and strong mental images of what occurred at the Hospital. He could remember precisely where he was standing and the layout of the room and its lighting (the accuracy of which was confirmed by Mrs Rawson in her evidence). His witness statement signed in May 2017 also appropriately contained only what he could personally remember.
41. As with Mrs Taylor, it was not suggested that he had fabricated any part of his evidence. He was, in my judgement, seeking to assist the court by recounting his own memory of events.
Mrs Rawson
42. Mrs Rawson is 57 years old. She qualified as a nurse in 1979 and became a midwife in 1984. By the time of Rebeccah’s birth she had been a midwife for 8 years. She still works for the Trust as a bank midwife, having retired from full-time work in 2018.
43. Mrs Rawson had no recollection of Rebeccah’s birth. Her evidence comprised a detailed explanation of the notes that were taken by her and others and a very helpful description of the practices and procedures at the Hospital at the time. She was able to identify precisely who had made which manuscript entries on the original medical records and why they were in the form that they were.
44. Mrs Rawson was an impeccable witness. She answered all questions put to her in cross-examination in a straightforward and open fashion. She clearly did not see it as her role to defend the Trust or her colleagues. On a number of occasions, she unhesitatingly provided answers in cross-examination which tended to corroborate points of detail in Mr and Mrs Taylors’ evidence. She had clearly given anxious and conscientious thought to every part of the medical records. Her evidence was measured, thorough and practical. She came across not only as a highly competent and conscientious midwife (and supervisor of trainee midwives) but also as a highly empathic and caring person. She was of great assistance to the court.
Dr Dobbs
45. On the first day of trial, the Defendant applied for an order under CPR 32.9(4) extending time for the service of a witness summary in relation to the evidence of Mr Dobbs. In support of that application, the Defendant served copies of emails which had been exchanged between the solicitors acting for the Defendant and Dr Dobbs. The application was not opposed. A signed consent order was presented to me. I accordingly granted the application and extended the time for service of the witness summary to the first day of trial. However, the Defendant had not issued or served a witness summons on Dr Dobbs and did not call him as a witness. In these circumstances, the main purpose of serving the witness summary, which is to give notice to the other party of what the witness was expected to say when called to give evidence, fell away. This then raised the question of what evidential value the witness summary document had.
46. For the Claimant, Mr Kemp submitted that the witness summary had no evidential value and furthermore adverse inferences ought to be drawn against the Defendant as a result of the fact that Dr Dobbs was not called as a witness. For the Defendant, Ms Mauladad submitted that I ought to admit into evidence what Dr Dobbs had told the Defendant’s solicitors (directly in his emails and as summarised in the witness summary) as hearsay evidence under s. 1 of the Civil Evidence Act 1995 without drawing any adverse inference. I will return to this below.
THE EXPERT EVIDENCE
The obstetricians
47. I heard live expert evidence from two obstetricians: Mr Roger Clements FRCS (Ed), FRCOG, FAE for the Claimant and Mr David Howe DM, FRCOG, FRCS (Ed) for the Defendant.
48. Mr Clements is an eminent obstetrician who has published a number of articles. He was a consultant obstetrician and gynaecologist and clinical director at the North Middlesex Hospital at the time the events in this case occurred. He is the author of many books, articles and papers in the course of his long and distinguished career. He expressed his views (both in writing and in cross-examination) in a forceful manner.
49. In an Appendix to his report, he used some unnecessarily pejorative language about a particular line of research in the United States. Ms Mauladad submitted that Mr Clements had not been objective in his approach to this case and had crossed the line into advocating for the Claimant. She pointed to the fact that Mr Clements is almost exclusively instructed by solicitors acting for Claimants.
50. I accept that Mr Clements’ use of language in the Appendix to his report was in places inappropriately strident, e.g. in paragraph 80 & ff. where he refers to ‘researchers’ (in inverted commas) producing literature on behalf of a ‘defence industry’ in the United States the effect of which was to permit Defendants to ‘escape responsibility’ for obstetric brachial plexus injury. Mr Clements had critically reviewed the same line of research in far more measured and balanced language in an article published in 2006. [2] An expert report prepared for court proceedings is not the place to pursue a campaign against particular lines of research or to impugn the motives of those who have funded that research. The offending passages were not germane to the issues in this case because of the agreed evidence of the orthopaedic experts on causation, so I feel able to simply ignore them.
51. However, I reject the more general submission that Mr Clements had crossed the line into advocacy. He was, I find, seeking to assist the court by presenting his own views based on many years of research and practice at the highest level.
52. Mr Howe’s written and oral evidence was measured and balanced. He was a senior registrar in a busy hospital and a research fellow at the time the events in this case took place. He was thus in a very similar position to that of Dr Dodds. His day to day contact with birthing mothers and accoucheurs was therefore somewhat greater than that of Mr Clements, who by 1992 was already a consultant and clinical director. As Mr Clements accepted in cross-examination, as a consultant in the NHS in 1992, he was only rarely involved in the actually delivery of a baby. However, he did retain more direct involvement with his private patients.
The midwives
53. I heard evidence from two midwifery experts: Fiona Sommerville, for the Claimant, and Susan Brydon, for the Defendant. In her written report, Ms Brydon had not listed Mrs Taylor’s liability witness statement dated 12 May 2017 as being one of the documents which she had read when preparing her report. She referred only to Mrs Taylor’s quantum witness statement dated 29 March 2018, which of course said nothing about the birth itself. When challenged about this in cross-examination, Ms Brydon initially dismissed this is a mere oversight and suggested that she “must have seen” Mrs Taylor’s liability witness statement. However, it soon became clear that she had not. She had failed to refer to Mrs Taylor’s own account of what the midwives had done anywhere in her report. This was a serious failing. It meant that Ms Brydon had only considered the factual evidence of the Defendant and Mr Taylor in coming to her conclusions. This basic failure ought to have been picked up by those representing the Defendant as well as Ms Brydon herself well before trial.
54. Ms Sommerville’s report was not marred by any such failing. In both her written and oral evidence she assisted the court in clarifying the midwifery standards and practices in place in 1992. In cross-examination, she withdrew her assertion (set out in para. 6.15 of her Report) that Mrs Rawson’s evidence suggested that excessive traction may have been applied by the midwives.
55. As a result of the concession made by Mr Kemp on behalf of the Claimant that the application of suprapubic pressure in the left lateral position was not contrary to accepted practice in 1992, which I have already referred to above, the relevance of the expert midwifery evidence was greatly reduced.
The orthopaedic experts
56. I was invited to read the reports of the consultant orthopaedic experts instructed by the parties, Professor B.C. Bainbridge for the Claimant and Professor G.E.B. Giddins for the Defendant. Their reports dealt with the likely cause of the OPBI in this case. Neither gave live evidence because a joint memorandum adequately set out the matters on which they agreed. One of the key matters they agreed upon was that the OPBI was caused by the distraction force applied by an accoucheur during the process of delivering Rebeccah.
57. Amongst other points, they agreed the following in their Joint Statement:
“8.a. The severity of the injury cannot show whether there was a short, sharp force applied or a sustained traction. The severity of the injury can, however, imply that there was a higher peak force, i.e. if it is a very severe grade III or IV injury then it is likely that there was a higher peak force applied across the brachial plexus than with a less severe injury as in this case. It is not, however, possible in either case to know whether there was a short, sharp traction or sustained traction.”
8.b. It is not possible to know whether the baby’s head was pulled towards the floor on the basis of the injury sustained. This is, however, very important. It is now established that it is safer to pull on the baby’s head axially i.e. in the line of the baby’s spine rather than applying downward traction which is now avoided. The experts understand that in 1995 that was not so clearly understood.”
Shoulder dystocia: its nature and treatment
58. In 1991, the following was said about shoulder dystocia in Gibb , a leading medical reference book:
“This term has never been satisfactorily defined. Difficulty with the shoulders precedes shoulder dystocia. In the mechanism of vaginal delivery the head may be delivered at the end of a contraction. The shoulders under these circumstances are delivered with the next contraction. Failure to achieve this constitutes shoulder dystocia” [3]
59. The Confidential Enquiry into Stillbirths and Deaths in Infancy (‘ CESDI ’) set up in 1992 considered fatal cases of shoulder dystocia. It commented as followed:
“There is no universally accepted definition of shoulder dystocia, which partly accounts for the different reported incidences between 0.23% and 1.1% of vaginal vertex deliveries …”
The figure given for the incidence of shoulder dystocia in England and Wales by Mr Clements was 1 in 1000 births.
60. Notwithstanding the lack of a universally agreed definition, there can be no doubt that in 1992, shoulder dystocia was recognised as an obstetric emergency. CESDI itself reviewed 56 cases of death during delivery from shoulder dystocia. Research carried out as part of CESDI found that the interval between the head of the baby being delivered and the body of the baby being delivered in these fatal cases was less than five minutes in 47% of cases. [4]
61. The findings of CESDI may be contrasted with the studies referred to by Mr Clements which indicate that a foetus in good condition can withstand 5-10 mins of total oxygen deprivation (anoxia) and still be resuscitated. In his evidence, Mr Howe made the point that in a shoulder dystocia case, the foetus may well have already experienced some oxygen deprivation before the condition is diagnosed. While he agreed with Mr Clements that 10 minutes was the standard period recognised in 1992 for the period a foetus might be expected to survive anoxia, obstetricians confronted with a case of shoulder dystocia in 1992 would not have regarded 10 mins as a reasonable period to allow themselves for delivery of the body following diagnosis of shoulder dystocia. His evidence was that a reasonably competent obstetrician would have wanted to get the baby out as soon as possible and in closer to 5 mins than 10 mins from diagnosis. I accept his evidence in this respect. As the CESDI study commented: “Given the short interval between delivery of the head and the delivery of the body in some of these fatal cases, the need for rapid response is obvious”.
62. The urgency of the situation is also emphasised in Dewhurst, one of the leading textbooks for postgraduate students of obstetrics and gynaecology, which says this in its 4 th edition (the one current at the time of Rebeccah’s birth):
“Time is of the essence. The accoucheur is faced with the difficulty of discovering on which side the foetal back lies. He must exclude any unsuspected localized abnormality which may be affecting the neck, chest or abdomen. There is little enough time to make even a cursory examination. Not only is the foetal cord compressed but also the foetal chest. Neither clearing the nasal and oral passages of mucus, nor the insertion of an oral airway will enable the child to breath. If the baby is to be saved prompt action is required” [5]
63. One of the other problems with shoulder dystocia is that it is very hard to predict. Having a large baby with a weight in excess of 4 Kg is a risk factor, as is maternal diabetes, but it has not been possible to identify robust predictive criteria for the condition. [6] Dewhurst says of shoulder dystocia that it “still constitutes one of the unsuspected hazards of an otherwise well-conducted pregnancy and labour”. [7]
64. A paper, albeit dating from 1943, accurately sums up the practical challenge presented by shoulder dystocia, as applicable in 1992 as when it was published, as follows:
“Very few of our mechanical problems in obstetrics require emergency treatment. Difficulty in the delivery of shoulders, however, usually comes as a complete surprise. We have no warning, a real emergency exists, and the minutes we have in which to make a safe delivery usually pass much faster than expert help can arrive” [8]
65. The following points were agreed by the obstetric experts:
· In 1992, there were no national guidelines in place for handling shoulder dystocia. The first such guideline was not published until 2005.
· The application of forceful traction on the baby’s head without changing the mother’s position would not have been acceptable in 1992.
· The application of traction by the midwives before calling for help and turning the mother on her side would have been seen as inappropriate in 1992.
· Applying simultaneous suprapubic pressure and some moderate traction was an acceptable practice in 1992.
· In 1992 there was no recommendation to limit traction as much as possible to axial traction in line with the baby’s spine. Traction with a downward component was acceptable.
· Moving the mother onto her left side or into a lithotomy position [9] was an appropriate manoeuvre in 1992.
· Performing an episiotomy as a response to shoulder dystocia was an acceptable practice in 1992.
Diagnostic traction
66. Mr Clements emphasised in his evidence that ‘excessive traction’ ought to be avoided at all stages because of the risk of causing a brachial plexus injury. He used the term ‘diagnostic traction’ to describe the sort of gentle traction which was required to see whether the use of a manoeuvre such as a change in the position of the mother or the application of suprapubic pressure had brought about a situation in which the shoulders of the baby were freed. He pointed to the following comments in support of his view. First, in Dewhurst : “Excessive rotation or traction must not be used as it is easy to fracture the cervical vertebrae or tear the brachial plexus and leave the child with a permanent Erb’s palsy”. Secondly, in Schwartz and Dixon : “if any of the above manoeuvres succeed, one can usually proceed with the delivery, using moderate traction and pressure …” [10]
67. There was a disagreement between Mr Howe and Mr Clements about whether ‘diagnostic traction’ was a term of art or not in 1992. Mr Howe said that it was not. In his oral evidence Mr Clements emphasised that he was using the adjective ‘diagnostic’ in its ordinary sense. His use of the term in connection with shoulder dystocia was supported by a paper delivered in 1955, in which the following appears (with emphasis added):
“Whatever may be the objections to making traction upon the neck of the child – and there are many – there is no doubt that as a first step it is safe and prudent to begin by making very gentle traction on the delivered head, drawing it gently backwards without forced rotation and without excessive angulation, at the same exhorting the conscious patient to bear down. This is essentially a diagnostic procedure ….
It is important to make the traction smooth and continuous and to avoid the application of sudden jerks. The duration of tractive effort should rarely exceed 4 – 5 seconds. One effort is enough. If it fails, the attempt at delivery should be abandoned in favour of other methods” [11]
68. Mr Howe accepted that excessive traction ought to be avoided but made two points:
a. In 1992 it was standard practice to apply suprapubic pressure together with some traction which was more than mere diagnostic traction (in the sense in which Mr Clements used the term).
b. The emphasis in 1992 was on getting the hypoxic baby out quickly (i.e. in the order of 3 – 5 minutes) in order to avoid brain damage or death.
69. I accept these two points. They were amply supported by the literature to which I was referred.
ISSUES
70. In his closing submissions on behalf of the Claimant, Mr Kemp pointed out that it was common ground that the Claimant’s OPBI was caused by traction being applied. He invited me to consider two separate periods after the Claimant’s head was delivered in which he submitted excessive traction was applied:
a. Period 1: from the delivery of the head when only the midwives were in attendance until Dr Dobbs arrived.
b. Period 2: Between the arrival of Dr Dobbs and Rebeccah’s delivery at 20.35.
71. On behalf of the Defendant Ms Mauladad accepted in her closing submissions that if Mr and Mrs Taylor’s evidence of what had occurred during Period 1 was found to be both reliable and accurate, then the Claimant’s claim would succeed.
72. As to Period 2, the main issues were: (a) how much reliance could be placed on Dr Dobbs’ signed note; (b) what, if any, adverse inference could be drawn from the fact that he was not called as a witness; and (c) whether he applied excessive traction. Mr Kemp referred to Period 2 as his ‘primary case’.
APPROACH TO THE FACTUAL WITNESS EVIDENCE
73. Ms Mauladad drew attention to the fact that Mr and Mrs Taylors’ witness statements were signed over 24 years after the events in question.
74. She referred me to a number of recent authorities in which warnings have been given about the need for judges to be cautious about the reliability of witness evidence about events which took place many years ago.
75. These authorities have recently been helpfully reviewed and summarised by Stewart J in Kimathi v. Foreign and Commonwealth Service [2018] EWHC 2066 (QB) as follows:
“95. In recent years there have been a number of first instance judgments which have helpfully crystallised and advanced learning in respect of the approach to evidence. Three decisions in particular require citation. These are:
• Gestmin SGPS SA v Credit Suisse (UK) Limited [2013] EWHC 3560 (Comm)
• Lachaux v Lachaux [2017] EWHC 385
• Carmarthenshire County Council v Y [2017] 4 WLR 136
96 Rather than cite the relevant paragraphs from these judgments in full, I shall attempt to summarise the most important points:
i) Gestmin :
• We believe memories to be more faithful than they are. Two common errors are to suppose (1) that the stronger and more vivid the recollection, the more likely it is to be accurate; (2) the more confident another person is in their recollection, the more likely it is to be accurate.
• Memories are fluid and malleable, being constantly rewritten whenever they are retrieved. This is even true of "flash bulb" memories (a misleading term), i.e. memories of experiencing or learning of a particularly shocking or traumatic event.
• Events can come to be recalled as memories which did not happen at all or which happened to somebody else.
• The process of civil litigation itself subjects the memories of witnesses to powerful biases.
• Considerable interference with memory is introduced in civil litigation by the procedure of preparing for trial. Statements are often taken a long time after relevant events and drafted by a lawyer who is conscious of the significance for the issues in the case of what the witness does or does not say.
• The best approach from a judge is to base factual findings on inferences drawn from documentary evidence and known or probable facts. "This does not mean that oral testimony serves no useful purpose… But its value lies largely… in the opportunity which cross-examination affords to subject the documentary record to critical scrutiny and to gauge the personality, motivations and working practices of a witness, rather than in testimony of what the witness recalls of particular conversations and events. Above all, it is important to avoid the fallacy of supposing that, because a witness has confidence in his or her recollection and is honest, evidence based on that recollection provides any reliable guide to the truth".
ii) Lachaux :
• Mostyn J cited extensively from Gestmin and referred to two passages in earlier authorities. I extract from those citations, and from Mostyn J's judgment, the following:
• "Witnesses, especially those who are emotional, who think they are morally in the right, tend very easily and unconsciously to conjure up a legal right that did not exist. It is a truism, often used in accident cases, that with every day that passes the memory becomes fainter and the imagination becomes more active. For that reason, a witness, however honest, rarely persuades a judge that his present recollection is preferable to that which was taken down in writing immediately after the incident occurred. Therefore, contemporary documents are always of the utmost importance…"
• "…I have found it essential in cases of fraud, when considering the credibility of witnesses, always to test their veracity by reference to the objective fact proved independently of their testimony, in particular by reference to the documents in the case, and also to pay particular regard to their motives and to the overall probabilities…"
• Mostyn J said of the latter quotation, "these wise words are surely of general application and are not confined to fraud cases… it is certainly often difficult to tell whether a witness is telling the truth and I agree with the view of Bingham J that the demeanour of a witness is not a reliable pointer to his or her honesty."
iii) Carmarthenshire County Council :
• The general rule is that oral evidence given under cross-examination is the gold standard because it reflects the long-established common law consensus that the best way of assessing the reliability of evidence is by confronting the witness.
• However, oral evidence under cross-examination is far from the be all and end all of forensic proof. Referring to paragraph 22 of Gestmin , Mostyn J said: "…this approach applies equally to all fact-finding exercises, especially where the facts in issue are in the distant past. This approach does not dilute the importance that the law places on cross-examination as a vital component of due process, but it does place it in its correct context."
97. Of course, each case must depend on its facts and (a) this is not a commercial case and (b) a central question is whether the core allegations happened at all, as well as the manner of the happening of an event and all the other material matters. Nevertheless, they are important as a helpful general guide to evaluating oral evidence and the accuracy/reliability of memory.”
76. Mr Kemp did not seek to challenge the accuracy of Stewart J’s summary of the cases or the principles enunciated in them. I therefore accept it as a helpful general guide to the correct approach to the witness evidence in this case.
FINDINGS OF FACT
Period 1
77. Mrs Taylor’s recollection was that the midwives were pulling so hard on Rebeccah’s head that she was pulled down the bed with each tug. In her oral evidence, she described this as a “whole body experience” and that it felt “out of control”. She was sure that she experienced this extreme pulling before other people rushed into the room and being thrown on her side. She did not recall any pulling after being put on her left side and the episiotomy cut being made.
78. In his witness statement Mr Taylor said that after Rebeccah’s head came out, “one of the midwives started pulling on the head, extraordinarily forcefully.” He thought both mid-wives may have “had a go”. He gave this graphic account:
“I could not believe that you could pull so hard on a baby’s head; it was like a scene in a farmyard when a calf is pulled out using ropes. The more senior-looking midwife was exerting so much force on my baby’s head that her arms were visibly shaking. The whole scene was so shocking”.
79. Mr Taylor was sure that all this occurred before the emergency bell was pressed.
80. Mr Taylor maintained this account in cross-examination. He said he recalled the “absolute brutality of the pulling” and said it was “extremely excessive”. He said the midwives alternated and both used the same force.
81. He contrasted the extreme pulling of the midwives with what happened after the registrar arrived. In relation to that, he said this in his oral evidence: “It wasn’t the same sort of pulling. It was a gentler pulling. Nothing like the farmyard scene”. He said that after Rebeccah had been put in an incubator he went out to smoke a cigarette and saw the student midwife on her own sobbing.
82. In cross-examination Mrs Rawson confirmed that she had no memory at all of Rebeccah’s delivery. She could easily identify her handwriting on the notes, which were in a standard format in use at the time.
83. Mrs Rawson also said she had no recollection of student midwife Godfrey. She thought that student midwife Godfrey was a woman because in 1992 they only had one male student midwife and that was not him. She said though that it was clear from the notes that it was the student who was delivering the baby with Mrs Rawson supervising. This meant that student midwife Godfrey was a senior student.
84. Mrs Rawson’s evidence was that “20:30” had been inserted in the notes by the student midwife but that she had changed it to “20:32 approx”. She said this change would have been because it was her practice to check with the switchboard to find out when the emergency call had been put out. She said they must have told her it was 20:32 so she corrected the original time. I accept her evidence about this and, given the change was made only 30 minutes later at the end of her shift, there is no reason to doubt that it is accurate. She added the word approximately because there was clearly some time spent by her and student midwife Godfrey diagnosing shoulder dystocia between Rebeccah’s head emerging and the emergency alarm being sounded. As she readily accepted, it was possible that the original entry of 20.30 may in fact have been correct for actual delivery of Rebeccah’s head.
85. Nothing in the end turned on the alteration. It was not suggested to Mrs Rawson that there was an attempt being made to “lose” 2 minutes in order to cover something up. All that happened was a perfectly ordinary correction of a time entry based on information received from the switchboard when the final notes were written up.
86. Mrs Rawson said that she was very familiar with shoulder dystocia. She had been trained how to respond as a student and in her career to date she has experienced it 30-40 times. She explained that the following three elements were part of her repertoire (in 1992): (i) change of maternal position (ii) episiotomy (iii) supra-pubic pressure.
87. From the midwife’s perspective, once shoulder dystocia had been encountered the standard response was to press the emergency alarm. She added that if a student identified or suspected it, she as a supervising midwife would have checked personally before sounding the alarm.
88. The evidence of Mr and Mrs Taylor of extreme pulling by her and student midwife Godfrey was put to Mrs Rawson fully and forcefully by Mr Kemp on the Claimant’s behalf. Mrs Rawson’s response was:
a. That extreme pulling of the type described by Mr and Mrs Taylor was not something that she would ever have done herself or permitted a student to do in her presence. It was not how she was trained and it was not how she behaved in any of the 30 – 40 shoulder dystocia cases which she had experienced.
b. If she had seen a student start to apply traction in anything like the way described by Mr and Mrs Taylor, she would have immediately intervened to stop it and take over. It would have led to a report being made about the student. She explained that the supervising midwife stands next to the student throughout so there is no chance of missing anything.
c. The student midwives, if anything, tended to be too cautious in their physical handling of delivery rather than the opposite.
d. There is no reason for midwives to go it alone or apply traction when they can so easily summon help. When the alarm sounds, everyone on the ward who is available would come very quickly. The layout of the department meant that help was close by.
e. The most important thing the midwife can do is to summon help quickly.
f. Once the registrar or other senior clinician enters the room, he/she takes over from the midwives.
g. She accepted that by the end the delivery might well have appeared to Mr Taylor like a farmyard scene, with Mrs Taylor having been cut and torn in the course of the delivery.
h. As to Mr Taylor’s evidence that the student midwife was sobbing afterwards, Mrs Rawson thought this was entirely possible. Shoulder dystocia is a grave emergency. The baby’s life is at risk. It is distressing.
89. In deciding, as I must, on the balance of probabilities what occurred in that delivery room over 25 years ago in the course of 2 minutes between Rebeccah’s head emerging around 20.30 and the point at which Dr Dobbs entered the delivery room, I have to have regard to all the evidence, including in particular the contemporaneous notes.
90. I have no hesitation in accepting Mrs Rawson’s evidence. I have no doubt at all that she would not have allowed a student midwife to apply excessive traction to Rebeccah and would not have done so herself. If anything untoward had happened during the delivery, I am satisfied she would have recorded it. I do not believe that Mrs Rawson would have acted contrary to her own training as a midwife or that she would have allowed a student under her supervision to have applied extreme traction. I accept Mrs Rawson’s evidence about the tendency of students to be overcautious. An extreme exception to that general rule would not have been overlooked by her.
91. I have no doubt that Mr and Mrs Taylor were doing their best to recall the traumatic birth of their daughter and that they genuinely had strong memories and mental images of what happened. They recalled many details such as the layout of the room, the lighting and who was in the room. I accept Mr Kemp’s submission that the parental evidence was internally consistent. However, I suspect the main explanation for this is that, as Mrs Taylor accepted in cross-examination, they had discussed the events many times.
92. I also accept Mr Kemp’s submission that neither Mr or Mrs Taylor attempted to fill in or gild their evidence. They were, as I have already observed, entirely honest and credible witnesses. However, the key question is whether I accept their evidence about extreme pulling by the midwives 25 years after the event in question as reliable. I do not. I prefer the evidence of Mrs Rawson on this key issue. As the case law I cited above emphasises, strength of belief, in particular in relation to flash bulb type memories of traumatic events, is not a reliable guide to the accuracy or reliability of that memory. This is particularly so when the events in question lie many years in the past.
93. I find Mrs Rawson’s evidence to be more reliable than that of Mr and Mrs Taylor for three principal reasons: (a) it is consistent with the contemporaneous notes of the delivery; (b) it is consistent with the inherent probabilities of the situation, in particular given Mrs Rawson’s training, experience and practice; and (c) I found Mrs Rawson’s oral evidence during cross-examination so convincing and trustworthy.
94. I accordingly make the following findings of fact in relation to what occurred during Period 1:
a. At the point at which Rebeccah’s head was delivered at around 20.30 both midwives were at the foot of the bed. Mr Taylor was on the other side of the bed near the chair holding Mrs Taylor’s left hand. The door was on the opposite side of the room.
b. Student midwife Godfrey had delivered Rebeccah’s head. Mrs Rawson was standing next to her supervising.
c. They were expecting a normal delivery.
d. Rebeccah’s body did not follow with the next contraction. Shoulder dystocia was diagnosed by the student midwife and then confirmed by Mrs Rawson.
e. As part of the diagnosis some traction was applied to Rebeccah’s head. The traction applied by the midwives was diagnostic as part of forming a clinical judgement that the shoulders were stuck. There was no extreme or excessive traction applied at any time by either midwife.
f. As soon as shoulder dystocia was diagnosed, Mrs Rawson ordered the alarm in the room to be activated.
g. The alarm was sounded without delay at 20.32.
h. Within a very short period of time (less than one minute) other staff summoned by the alarm began to arrive. There was a sense of urgency to deliver Rebeccah once the shoulder dystocia was diagnosed but no panic.
i. Mrs Taylor was repositioned on the bed and rolled onto her left side by the midwives with a degree of urgency and force (which was not unreasonably perceived by Mrs Taylor as her being dragged down the bed and ‘thrown’ onto her side). The midwives were possibly assisted in these manoeuvres by one or more other medical staff as they arrived.
j. As soon as Dr Dobbs arrived he took over.
k. Mrs Rawson wrote up her notes only half an hour after the delivery at the end of her shift at 9 pm. In doing so she changed the time of the delivery of Rebeccah’s head to 20.32 based on the time at which she was told that the emergency call was put out by the switchboard.
Period 2
95. I turn now to the Period between Dr Dobbs entering the delivery room shortly after the alarm was sounded at 20.32 and Rebeccah’s delivery at 20.35.
96. Dr Dobbs’ contemporaneous manuscript note in the operative delivery section of the medical notes, which he then signed, read:
“ Shoulder dystocia – [head] delivered
episiotomy cut + ant. shoulder del.
[with] suprapubic pressure + traction”.
97. Mrs Rawson’s note records:
[3] Patient → left lateral. Attempt to deliver posterior shoulder
[4] Suprapubic pressure applied
[5] Episiotomy performed.
[6] Live female delivered Apgar 5 at 1
98. There is on the face of the two notes a conflict of sequencing. Mrs Rawson has suprapubic pressure being applied before the episiotomy whereas Dr Dobbs has them the other way round. The other inconsistency is that Mrs Rawson’s note does not refer to traction at all whereas Dr Dobbs’ note refers to traction being applied in addition to suprapubic pressure.
99. Neither Mrs Rawson nor Dr Dobbs had any memory at all of the delivery.
100. Mr Taylor’s view of events in period 2 was reduced because more people were in the room, he was pushed to one side and the lighting was reduced. However, his evidence was that traction was applied after Mrs Taylor was cut and while she was on her side but that this was gentler than before.
101. Mrs Taylor recalled the pain of the episiotomy as being “almost immediately” after being “thrown” onto her left side. Mrs Taylor did not know what the doctors did to deliver Rebeccah.
102. Mr and Mrs Taylor’s evidence is thus consistent with Dr Dobbs’ contemporaneous note.
103. A letter written only nine days after the delivery to Mrs Taylor’s GP by the Hospital stated:
“The anterior shoulder was delivered with the aid of suprapubic pressure and generous episiotomy. Moderate traction was required to deliver the shoulder and the body”
104. Mr Kemp submitted that there was no clear evidence of what Dr Dobbs did when he entered the delivery room. I disagree. Dr Dobbs’ signed contemporaneous note is very clear and the sequence of events he sets out in that note is consistent with Mr and Mrs Taylor’s own evidence.
105. Based on the evidence I have referred to above I consider that I can safely and properly make the following findings of fact as to what occurred in Period 2:
a. Dr Dobbs entered the delivery room very shortly after the alarm was sounded at 20.32. Mrs Taylor was either already on her left side or that change of position was in the process of being completed.
b. Having been briefed that, in the view of the midwives, there was shoulder dystocia, Dr Dobbs took charge.
c. The general lights were turned off and the central spotlight turned on.
d. Dr Dobbs checked the diagnosis of shoulder dystocia. To do so diagnostic traction was applied.
e. Dr Dobbs gave instructions to Mrs Rawson. The student midwife played no further part in the delivery.
f. An episiotomy was performed either by Dr Dobbs or possibly by Mrs Rawson at Dr Dobbs’ direction.
g. Rebeccah was delivered at 20.35 by Dr Dobbs using a combination of suprapubic pressure (applied by Mrs Rawson at the direction of Dr Dobbs) and moderate traction applied to Rebeccah’s head. Mrs Taylor remained in the left lateral position throughout.
h. Given Mrs Taylor’s position, the traction was not applied entirely along the axis with Rebeccah’s spine but had a downward component.
i. There was no panic.
j. There was no extreme or sharp traction applied by Dr Dobbs at any stage.
106. I have come to these conclusions without making any reference to the witness summary served in respect of Dr Dobbs or the material I have seen served in support of the application for an extension of time to serve that summary. I prefer to rely on Dr Dobbs’ signed manuscript note taken together with the evidence of Mrs Rawson and Mr and Mrs Taylor. In placing reliance on Dr Dobbs’ signed manuscript note, I have firmly in mind the following observation of Tomlinson LJ in Synclair v East Lancashire Hospitals NHS Trust [2015] EWCA Civ 1283:
“Clinical records are made pursuant to a clear professional duty, serious failure in which could put at risk a practitioner’s registration. Moreover, they are not compiled simply as a historical record, they fulfil an essential and ongoing purpose in informing the care and treatment of a patient. Contemporaneous records are for these reasons inherently likely to be accurate.” [14].
107. As to the inconsistencies between Mrs Rawson’s note and Dr Dobbs’ note, I regard Dr Dobbs’ note as being the more reliable account of what he did and the order in which he did it. Mrs Rawson accepted in cross-examination that her note was not as full as it might have been. I do not feel compelled to read her note as meaning that suprapubic pressure was applied only once before the episiotomy and then not again. The natural reading of Dr Dobbs’ note is that Rebeccah was delivered using suprapubic pressure in combination with traction. This was the standard practice in 1992 so it is inherently likely that he would have followed it, quite apart from the fact that this is exactly what he has recorded in his own signed note.
Adverse inference
108. Mr Kemp invites me to draw an adverse inference from the fact that the Defendant did not call Dr Dobbs as a witness. He relies on Wisniewski v Central Manchester Health Authority [1998] 4 WLUK 14, in which the Court of Appeal upheld the drawing of an adverse inference by the trial judge as a result of the failure of the Defendant to arrange for a Dr Renninson to give evidence.
109. In that case, Brooke LJ reviewed a line of cases which considered the issue of when it was appropriate to draw an adverse inference from the absence of a witness. He derived the following four principles:
(1) In certain circumstances a court may be entitled to draw adverse inferences
from the absence or silence of a witness who might be expected to have material evidence to give on an issue in an action.
(2) If a court is willing to draw such inferences they may go to strengthen the
evidence adduced on that issue by the other party or to weaken the evidence, if any, adduced by the party who might reasonably have been expected to call the witness.
(3) There must, however, have been some evidence, however weak, adduced by the former on the matter in question before the court is entitled to draw the desired inference: in other words, there must be a case to answer on that issue.
(4) If the reason for the witness’s absence or silence satisfies the court, then no such adverse inference may be drawn. If, on the other hand, there is some credible explanation given, even if it is not wholly satisfactory, the potentially detrimental effect of his/her absence or silence may be reduced or nullified.
110. These four principles have recently been considered and applied by the Court of Appeal in Manzi v. King’s College Hospital NHS Foundation Trust [2018] EWCA Civ 1882. Lord Justice Sales emphasised this point:
“ Wisniewski is not authority for the proposition that there is an obligation to draw an adverse inference where the four principles are engaged. As the first principle adequately makes plain, there is a discretion i.e. “the court is entitled [emphasis added] to draw adverse inferences”.”
111. The fact that a potential witness has no recollection at all of the events in question may be considered a good explanation for not calling him or her – see e.g. Welds v Yorkshire Ambulance Service NHS Trust [2016] EWHC 3325 (QB) at [58], HHJ Freedman sitting as a Deputy Judge of the High Court:
“Similarly, given that Ms Piper has no recollection of the incident and was reluctant to be involved, that again seems to me to be a good reason for the defendants not calling her to give evidence. Whilst it is true that the defendants called Mr Lee to give evidence even though he had no independent recollection of the incident, it does not follow that the defendants should be reasonably required to call evidence from a former employee who can give no independent account of what occurred. In short, I find that there were proper reasons and credible explanations as to why the defendants did not call the midwives and that therefore it would not be right to draw any adverse inference.”
112. It is not appropriate to treat the four principles set out by Brooke LJ in Wisniewski as if they were a statute or Welds as establishing a rule that no adverse inference will ever be drawn where the witness who is not called says he or she has no recollection of events. Whether or not it is appropriate in any case to draw an adverse inference from the absence of a witness will be a highly fact sensitive matter which will depend on all the circumstances of the case, both procedural and evidential.
113. Among the particular factors in play in Wisniewksi were the following:
a. The Defendant had been slow to serve any witness statements at all. An unless order had to be obtained.
b. There was a six day break in the proceedings. Just before the break, the trial judge made clear that he was unlikely to give any weight to the statement of Dr Renninson unless he gave evidence either live or via video link. Despite the indication given by the trial judge, no further efforts were made to contact Dr Renninson and he was not called.
c. No other member of the medical staff was called. The Court of Appeal noted: “In addition to Dr Renninson’s absence, there was also a deafening silence from the other members of the relevant medical team at the hospital. Neither the registrar who had been on call that night nor the consultant with overall responsibility for the team attended to tell the judge what the practice at that hospital was for handling situations like the one that presented itself at 3.40 a.m.”
d. The trial judge concluded that the Defendant had taken a decision not to call evidence from Dr Renninson for tactical reasons.
e. The Claimant’s expert evidence had identified a course of action which ought to have been adopted by a doctor and the hearsay statement served by the Defendant (after the expert report in question had been served) was silent on this point.
114. In the present case I am not persuaded to draw any adverse inference from the absence of Dr Dobbs for the following reasons:
a. This is not a case where the Defendant has chosen not to call a witness for tactical reasons. The Defendant has chased Dr Dobbs and sought on numerous occasions to obtain his co-operation and attendance at trial.
b. The Defendant has been open and transparent about the timing and content of its communications with Dr Dobbs. All the email communications were disclosed as part of the application for an extension of time and the witness summary itself accurately reflected the nature of what he had told the Defendant’s solicitors. There is nothing in the substance or tone of those communications to suggest that Dr Dobbs had anything to hide.
c. Dr Dobbs has confirmed that he has no independent recollection of Rebeccah’s delivery and had ceased to work in obstetrics 15 years ago, so there is nothing he could usefully add to his own contemporaneous note.
d. The Defendant in this case has called live evidence from the midwife who was present throughout the whole delivery and who was able to speak to and explain the hospital’s procedures and records.
e. The Claimant could have served a witness summons on Dr Dobbs but did not.
f. The consent order, signed by the Claimant’s solicitor immediately prior to the commencement of the trial, was in the following terms: “The Defendant has permission to serve the witness summary as sufficient evidence in the matter of the witness evidence of Dr Stephen Dobbs, consultant obstetrician and gynaecologist.” (emphasis added). The terms of this consent order suggest that the Claimant’s solicitors had satisfied themselves that the reasons given for not calling Dr Dobbs were good ones and that there was no basis on which they could object to the evidence of Dr Dobbs being admitted and evaluated alongside all the other evidence in the case.
g. The Claimant has not identified a specific allegation on which the contemporaneous documentary evidence was silent and in relation to which Dr Dobbs might reasonably be expected to be able to provide helpful oral evidence.
115. I accept the Defendant’s submission that Dr Dobbs’ witness summary and the materials underlying are admissible under the Civil Evidence Act 1995. However, I have been able to come to firm conclusions about what happened in the delivery room while Dr Dobbs was present without recourse to his witness summary or the underlying e-mails.
FINDINGS ON THE ALLEGATIONS OF BREACH
116. In light of the foregoing findings of fact as to what the midwives did during Period 1, the Claimant’s case of negligence based on an allegation of excessive traction necessarily fails.
117. As to the case based on excessive traction by Dr Dobbs in Period 2, having found that Mrs Taylor was put in a left lateral position and Rebeccah was delivered by means of an episiotomy and a combination of suprapubic pressure and (moderate) traction, the claim of negligence in this period also fails in light of the expert obstetric and orthopaedic evidence set out in paragraphs 47 – 69 above.
118. It is now recognised that downward traction should not be applied because of the risk of nerve avulsion [12] . However, in 1992 the application of moderate downward traction (e.g. with the mother in a left lateral position) was an accepted practice which was documented in textbooks such as Dewhurst . [13] It is very unfortunate that Rebeccah was born before the danger of downward traction was recognised but it was common ground that negligence had to be proved by reference to the standards and practices in place in 1992 rather than by the standards of today.
119. There is no factual evidence to support the allegation that Dr Dobbs applied excessive force. The letter sent only nine days after the birth to Mrs Taylor’s GP, which was not challenged at the time, referred to ‘moderate traction’. Mr Taylor’s own evidence was that the traction applied after the alarm was sounded was gentler than the traction he recalled seeing earlier. Had Dr Dobbs delivered Rebeccah using unusual or excessive force I am confident that Mrs Rawson would have said something about this at the time, recorded it and/or remembered it.
120. In summary, I conclude that Rebeccah was delivered by Dr Dobbs, following a correct diagnosis of shoulder dystocia, using a combination of three techniques accepted at the time as appropriate, namely an episiotomy, suprapubic pressure and moderate traction. The reason why Rebeccah suffered a brachial plexus injury was that the traction applied had a downward component. This was accepted practice at the time but is something which is now avoided precisely because of the risk it carries of causing brachial plexus injury.
DISPOSAL
121. The Claimant’s claim is dismissed.
[1] Narakas A., ‘Obstetrical brachial plexus injuries’ in Lamb DW, ed. ‘The paralysed hand’, Edinburgh: Churchill Livingston (1987) pp. 116 – 135.
[2] Clements, ‘ Obstetric brachial plexus injury’, Clinical Risk (2006) vol. 12, pp.3-11.
[3] Gibb, ‘Common Obstetric Emergencies’ (1991) p. 69.
[4] Hope et al, ‘Fatal shoulder dystocia: a review of 56 cases reported to the Confidential Enquiry into Stillbirths and Deaths in Infancy’, B.J.O.G Dec 1998 Vol 105 pp. 1256 – 1261 at p. 1259.
[5] ‘Dewhurst’s Textbook of Obstetrics and Gynaecology for Postgraduates’, ed. C.R Whitfield 4 th edition 1986. p. 382.
[6] Acker, Sachs and Friedman (1985) found that the two-factor combination of diabetes and foetal weight of 4000 + g provided the best predictability. Their conclusion though was that “the use of flagging criteria is valuable for screening out gravidas who are not likely to develop shoulder dystocia but they cannot be relied upon completely for anticipating the condition”.
[7] Op cit. p. 382.
[8] Wood and Westbury, ‘A Principle of Physics as Applicable to Shoulder Delivery’ (1943) American Journal of Obstetrics and Gynaecology 45, pp. 796-804.
[9] I.e. mother lying on her back with legs bent at 45 degrees usually in supports.
[10] Schwartz and Dixon, ‘Shoulder Dystocia’ (1958) Obstetrics and Gynaecology Vol 11 No. 4 pp. 468 – 471.
[11] Morris W.I.C (1955) Reports of Societies, Journal of Obstetrics and Gynaecology of the British Empire Vol 62 pp. 302 – 306 at p. 304.
[12] Royal College of Obstetricians and Gynaecologists, Shoulder Dystocia Guidelines, 2005
[13] At p. 382: “ If positioning and an adequate episiotomy does not allow sufficient rotation and downward traction to be made, even with assistance from above….”
