Freely Available British and Irish Public Legal Information
[Home] [Databases] [World Law] [Multidatabase Search] [Help] [Feedback]
England and Wales High Court (Queen's Bench Division) Decisions
You are here: BAILII >> Databases >> England and Wales High Court (Queen's Bench Division) Decisions >> Macaulay v Karim & Anor [2017] EWHC 1795 (QB) (14 July 2017)
URL: http://www.bailii.org/ew/cases/EWHC/QB/2017/1795.html
Cite as: [2017] EWHC 1795 (QB)
[New search] [Printable PDF version] [Help]
QUEEN'S BENCH DIVISION
Strand, London, WC2A 2LL |
||
B e f o r e :
____________________
| IBIYINKA MACAULAY | Claimant | |
- and - |
||
| DR ABDUL KARIM (1) CROYDON HEALTH SERVICES NHS TRUST (2) |
Defendants |
____________________
Jane Mishcon (instructed by Brachers LLP) for the 1st Defendant
Bradley Martin (instructed by Capsticks LLP) for the 2nd Defendant
Hearing dates: 26-28 April, 2-5 May, 8-9 May and 11 May 2017
____________________
Crown Copyright ©
- The Claimant ('C'), who was then aged 53, was admitted as an emergency to King's College Hospital ('KCH') in the very early hours of the morning of 15 October 2011 in septic shock. He underwent extensive surgery later that day, probably commencing at about 10.00 or 11.00 or thereabouts.
- The net effect of the surgery that day (from which he was fortunate to survive) and of subsequent operations and/or surgical procedures thereafter was that it was necessary for his left leg to be amputated below the knee and for his right toes and his right fingers and thumb also to be amputated. He is plainly significantly disabled and disadvantaged in consequence.
- He had in fact visited his GP, Dr Abdul Karim ('D1'), at what was then the South Croydon Medical Centre, on 12 and 14 October and had presented himself at the A & E Department of what was then known as the Mayday Hospital in Thornton Heath, South London, on 13 October, making various complaints about the way he felt, but none of these attendances resulted in a diagnosis and treatment of the condition that led ultimately to the surgery referred to above.
- The essential issue in the case is whether Dr Karim and/or the Mayday Hospital (now known as Croydon University Hospital), for which Croydon Health Services NHS Trust ('D2') is responsible, were negligent in not identifying the underlying problem or its general nature sooner and taking steps to bring forward treatment, including surgery, that would have prevented or reduced the serious consequences summarised above.
- That broad issue in the case is easy to identify. For reasons that will emerge, it is far less easy to resolve. One major issue is the question of precisely what the underlying condition was that led to the need for surgery: put shortly, was the very significant infection that became apparent on his admission to KCH one that commenced in the pelvis (as a result of a perforated sigmoid colon diverticulum) and tracked down (as has been suggested on behalf of D1 and D2 since November 2016) or one that started in the perianal region, became more severe in the form of necrotising fasciitis and in consequence tracked upwards (as is contended on behalf of C)?
- The distinction between these aetiologies is said by D1 and D2 to make a material difference to the likely presentation of C's symptoms at important times in the chronology and to the potential effectiveness of any earlier operative intervention. Ms Jane Mishcon, for D1, submitted in her opening Skeleton Argument that the finding "as to the aetiology of the sepsis will be pivotal to the outcome of [the] case", a proposition she repeated in her closing submissions. Mr Simeon Maskrey QC, for C, whilst accepting that the issue might be important to one part of the claim against D1, does not accept that it alters materially the overall case he advances against D2 in respect of 13 October 2011 or against D1 in respect of 14 October 2011. He maintains that the case advanced by C in relation to the aetiology is, in any event, correct. I will revert to this debate in due course, merely noting at this stage that I received evidence from experts in six different specialities at least three of which had some bearing on this issue. (For convenience, I identify those experts in Appendix 1 to this judgment.) It is also a case where the boundaries between the various specialities arguably overlap. Clearly though, in line with the directions applicable to a trial such as this, the evidence of each expert must be addressed on the basis of whether the particular expertise is relevant to the issue being considered.
- Whatever the outcome of the case, it is right to acknowledge that C appears to remain a very cheerful character who does not look for sympathy. Nonetheless, Ms Mishcon and Mr Bradley Martin, for D2, both prefaced their cross-examinations of him (and indeed his wife) with appropriately generous expressions of sympathy for what he and his wife, and thus their family, have been through. Anyone who knew of the circumstances of the case would wish to do the same. I have referred already (see paragraph 2) to early concerns about whether he would survive, but it is to be noted that he remained at KCH initially for about 14 weeks (during which period he spent a prolonged period in intensive care) before being transferred to Guys and St Thomas' for reconstruction and rehabilitation in the plastic surgery unit. He returned to KCH for a further 10 weeks before being discharged in early April 2012. He is now left with the permanent consequences to which I have referred.
- I will turn to the background to the eventual admission to KCH in more detail. There are several material issues of fact which I will identify as I set out the background without, at this stage, necessarily seeking to resolve all of them. This is one case in which standing back from a detailed analysis of the individual components of the narrative and looking at the broader picture with the assistance of the expert evidence may prove necessary to enable findings of fact to be made based on the balance of probabilities. In some particular respects, I will be able to indicate my findings as I proceed through the chronology, but many of the more difficult issues will have to await determination until the broader picture has been examined. The resolution of these issues is rendered less easy because the general quality of many of the clinical notes (including issues of pure legibility) at material times is poor and timings are, in some respects, unclear. A number of the experts had difficulty in interpreting features of the notes. That makes the court's position particularly difficult.
- In relation to the account of events given by C, it will be important to bear in mind that it was not until his discharge from hospital 6 months after the dramatic events of October 2011, and thus after 6 months of prolonged treatment and hospitalisation, that he will first have had a reasonably settled opportunity to piece together his recollection of what occurred over those few days in the preceding October. He would not have had any records available with which to check his memory when putting together that recollection. As will emerge, this has some significance in determining what happened.
- C was born on 11 August 1958. His wife, Victoria, was born in 1975 and was thus 36 at the time of the material events. At that stage they had two daughters, aged nearly 5 and nearly 2 respectively. Since then they have had a third daughter born in November 2016.
- C had a medical history of Type II diabetes (which did not require insulin). He was regarded as "obese" by medical standards. On 23 September 2011, and thus less than 3 weeks before the material events, his weight was recorded by his GP practice as 135 kgs, which is a little over 21 stone. On 27 July 2011 he was 142 kgs (22 stone 5 pounds) with a Body Mass Index of 46.37 which was undoubtedly very high (evidencing "severe morbid obesity", according to Professor Sells). His diabetic management was generally good and it was monitored at the surgery where D1 was a practitioner. The fact that C was an obese diabetic is said to be relevant to the way his presentation in October 2011 should have been addressed.
- C's recollection is that he started feeling unwell on 11 October 2011 (which was a Tuesday) and on the following day he telephoned the South Croydon Medical Centre. D1, who had dealt with C on previous occasions (including recently in July, August and September 2011 for hay fever, cough/sore throat and gout respectively), telephoned him back at about "lunchtime" (according to C) and "after 1 pm" (according to D1). It was a day when the surgery closed at 1 pm and D1 says that he would stay on to carry out other work after the rest of the staff had left. The precise timing of the telephone conversation does not matter for this purpose.
- C's evidence is that he told D1 that he felt unwell and had flu like symptoms. He also said that he told D1 that he "was struggling to pass urine and was suffering from constipation." His account is that D1 said he needed antibiotics and that he should go to the surgery to collect the prescription.
- D1's account has some similarities, but there are differences. His note of the telephone consultation is that C was complaining of a cough, fever, sore throat and shivering. It records that C had been taking paracetamol and was feeling better, but that he felt "unwell". The note concludes with the words "also dm needs abx." The "dm" refers to the diabetes and the expression "needs abx" means "needs antibiotics". In fact, the note does not record which antibiotics were prescribed, but there is another internal record of the practice that indicates that he was prescribed Amoxicillin tablets (500 mg) three times per day, an antibiotic that he had also prescribed in August. The note recorded by D1 indicates that C had also been prescribed Loratadine, an antihistamine. That was provided, apparently, because C had suffered from hay fever in the past, though this was not recorded in the note.
- The note does not record any complaint of difficulty passing urine or of constipation. Equally, the note does not contain any record that a review or follow up appointment on Friday, 14 November was contemplated.
- There is a dispute of fact (probably not particularly relevant) about the circumstances in which the prescription came to be handed over. C's account, supported by his wife, is that she drove him to the surgery and that he picked up the prescription from the receptionist and did not see D1. D1 says that C went to the front door of the surgery sometime after 14.00 which, by then, was closed and he (D1) came to the door and handed over the prescription. According to D1, C returned to his car and drove himself away. D1 says that he told C that if there was any problem he could go to A & E or could come to the surgery the following day (though he, D1, would not be there on the Thursday) or Friday when he would be there. According to D1, C said that he would come in on Friday. C did not agree that any pre-arrangement for a further visit was made for the Friday. I think it is unlikely that any arrangement to come in on the Friday was contemplated at that time and I prefer C's recollection on this issue.
- Notwithstanding that, C did indeed go to the surgery again on the Friday, but I must deal next with what happened in between his departure from the surgery on the Wednesday afternoon and then.
- C said that, despite taking the two types of medication prescribed by D1, he woke up the following morning feeling worse. He said, and his wife again supports him, that he was unable to get out of bed to take his daughter to school as he usually did. He did not want his breakfast, a very unusual event since, as he put it in his witness statement, "I love my food". He could, of course, have gone back to his GP's surgery, but he asked his wife to telephone for an ambulance because of the pain he was in. His wife said he was complaining of pain.
- The records of the ambulance service show that a call for an ambulance was made at 09.36. Although there is an entry that might suggest that it was C who made the call, to the extent that it matters I think, on the balance of probabilities, that it was his wife who made the call since the mobile telephone number recorded was one she used. The brief description of the problem noted by the person taking the call was that C was a diabetic who had "body and joint pains", was "very weak" and that he had not been eating or taking his medication. It was recorded that he had "pain behind his eyes". There was no mention, it seems, of pain in the rectum or anus at this time, but there was such a reference when the ambulance arrived (see paragraph 21 below).
- The ambulance arrived at 09.46 and left with C at 10.18, arriving at the Mayday Hospital at 10.26. The clinical handover was at 10.36 and the patient handover was at 10.39.
- The ambulance crew noted that C was alert when they arrived, but was complaining of feeling unwell. They recorded a four-day history of "being unwell, reduced appetite, [no] diarrhoea and [complaining of] pain in the rectum." It was noted that he found it "difficult to sit normally due to pain in rectum." This record certainly suggests that he was complaining of pain in the rectum before he got into the ambulance and also suggested that there had been some history of that pain, along with other symptoms, prior to the day in question. Over two readings about twenty minutes apart, his respiratory rate was 28 (and thus raised), his pulse rate was about 120 (and thus raised representing a tachycardia) and his blood pressure was 133/75 and 123/79. His blood glucose level was 8.2 and his temperature was 37.9.
- The one entry on the ambulance record that is difficult to make out is the pain score on the scale of 0-10. It looks as if a zero was placed there originally for each timed assessment, but that would not make sense given the other observations to which I have referred. One interpretation is that a '4' had been put in each box, though that is by no means clear. Another interpretation is that it is a '9'. As will appear (see paragraph 25 below), that was the score given shortly afterwards at the hospital at the triage stage and would, therefore, be consistent with the position some 30-45 minutes earlier. However, an earlier score of 4 escalating to 9 might also be consistent with C's first witness statement where he said that "by the time I got to hospital I was suffering from severe pain in my bottom and that was the dominating issue." By then he would have been in the ambulance for a while and transferred to a trolley on arrival at the hospital. Nonetheless, since the precise pain score given to the ambulance crew is unclear it would probably be safer not to form any conclusion about it since it is not, in my view, crucial to the outcome of the case. What may be important is that there is no doubt that C was saying at the time the ambulance crew saw him that it was difficult to sit because of pain in the rectum and that this is a theme picked up when he got to hospital shortly afterwards (see paragraph 34 below).
- Although there is an entry in the Triage Notes (see paragraph 26 below) which suggests that C's wife accompanied him to hospital, Mrs Macaulay's recollection is that she did not do so, nor did she follow him there, because she had their younger daughter to look after. Nothing really turns on this because by the time he left the hospital later that day (see paragraph 51 below), it is clear that she had to be contacted to go to collect him. To the extent that it matters, I think she is probably correct in her recollection that she did not accompany C to hospital. As will appear below, she kept in touch with C, so far as was possible, via their mobile telephones.
- C's recollection, and this is borne out by other evidence, is that he was delivered to the A & E Department through the back door. Although some aspects of the descriptions given by some of the witnesses from the hospital were a little confusing, I believe it was common ground that at that time the back door led to the reception desk in the "majors" reception area which is where ambulance admissions took place. The patient would be clerked in and then triaged by a nurse.
- The triage nurse who saw C on his arrival (Nurse Shee), and whose assessment was carried out at 10.30, recorded his complaint in the Triage Notes as "pain in anus for the past two days and feeling generally unwell." The brief clinical findings were that he was alert, but had a headache, there was no nausea or vomiting, but there was pain. The "new" pain score was given as 9 which was categorised as "severe" and "excruciating, worst ever". His obesity and Type II diabetes were noted.
- The part of the Triage Notes headed 'Triage Requests' has ticks against the following: observations, blood sugar, urine, ECG and bloods. There was some speculation or debate amongst the experts called to give evidence about the implications of those requests (Dr Campbell-Hewson, the Consultant in Emergency Medicine, who gave evidence for D2, saying that he regarded it as a "suggestion" rather than a "request"), but in my view the best evidence comes (a) from the form itself and (b) the Consultant in Emergency Medicine at the Mayday Hospital at the time, Dr Oliver Spencer. Dr Spencer had been appointed Consultant in September 2011, but had some previous experience of the practice of the A & E Department of the hospital, including a year from August 2010 until August 2011 as a Speciality Registrar (at ST6 level) in Emergency Medicine.
- So far as (a) is concerned, it is plain, in my view, that (i) a request is a request and (ii) the existence of a column adjoining the column where the ticks referred to above can be placed headed "Done" (with a space for another tick) suggests that it is contemplated that the tests requested will be carried out rather than simply may be carried out. As to (b), Dr Spencer (who was not called to give evidence) said in a letter dated 19 June 2012 (in the context of an investigation into a complaint from C about what occurred on 13 October 2011) that "[the] triage documents further observations to be performed, blood sugar, urine, ECG and blood samples be taken" (my emphasis). (His witness statement, to which the letter was attached, was put in evidence on behalf of C pursuant to CPR 32.5(5).) It follows, therefore, that at some stage thereafter all those tests should have been carried out to inform a further examination and assessment of C in due course. When that should have been is a matter to which I will have to return (see paragraph 159 below).
- The Triage Notes (which appear as the second page of the CAS card to which I will refer in paragraph 30 below) contained provision for the assignment of a PAR ('Patient at Risk') score, but none was recorded in this document. It was recorded in another document to which I will refer below (see paragraphs 32 - 36).
- As will become clear, none of the tests requested at the triage stage had been carried out before C was seen either by the A & E Registrar shortly before 13.00 (see paragraph 37 below) or by Dr Michael Uhercik, the surgical Senior House Officer ('SHO'), shortly after 14.00. Before I come to that, however, I must deal with what happened after the triage assessment.
- At or about the time of admission a Casualty Card (called a 'CAS card' for short) was completed. The front page contained certain information about C and identified the Triage Nurse by number (188) and the time of the triage as 10.39 (the admission having been noted to have been at 10.26). The complaint was noted briefly as "pain in rectum", the duration of which is said to have been 2 hours 26 minutes. This conflicts with what appears in the records of the ambulance staff and what was said to the triage nurse (see paragraph 25 below). The document does not appear to be a document of clinical significance and this entry can, I think, safely be ignored.
- The document contains an entry which indicates that C was assigned to cubicle 4 on the left side of the "majors" area. It also indicates that the PAR score was 2. As will emerge in due course (see paragraph 58 below), the original CAS card remained in the A & E Department, but when C was referred to the surgical team (see paragraph 37 - 38 below) a copy of the CAS card (including the Triage Notes) was taken and accompanied C when he was seen by the surgical team.
- Before continuing with the sequence of events in the hospital, I should give a little more detail about how the PAR score is arrived at. There is a document in the clinical records which shows the way in which the PAR score is achieved. There are six parameters as follows: conscious level, respirations per minute, heart rate per minute, systolic blood pressure, temperature and urine output over the last 24 hours. Each parameter is given a normal range for example, a heart rate in the range 51 - 100 is normal to which a zero score is given. However, if the reading is outside the normal range as given (either too high or too low), a score of 1, 2 or 3 is assigned depending on how far from the normal that it is. For example, a heart rate of 101 110 is given a score of 1 and a heart rate of 111 129 is given a score of 2. The higher the overall score given all the parameters, the greater is the risk to which the patient is said to be subject.
- That PAR score of 2 was derived from a series of observations recorded on an observation chart at 10.50. It appears from that chart that C's respiratory rate was about 16 at this time, which scored 1, and his heart rate was about 105, which also scored 1. That resulted in the PAR score of 2. (It might also be noted that his blood pressure at that time was 110/40 which meant that the systolic pressure was normal, but the diastolic pressure at 40 was low. Although it does not appear that a low diastolic pressure was a factor to be included in the PAR score, a diastolic pressure of less than 50 was said on the observation chart to require the attention of a senior member of staff to be drawn to it because the "patient is potentially unstable".)
- C was seen by a nurse at about 11.15. The note records that C stated that he was "unable to get off trolley" and that he said "his back and hips [were] painful". The note records that he said he had been unable to pass urine "since last night" and that he was refusing Co-codamol since he had that at home and he wanted "stronger analgesia". He was prescribed 1 mg of Voltarol (a non-steroidal anti-inflammatory drug) at 11.25, according to the medication chart. No bloods were taken at this time.
- Nothing else happened until another set of observations was undertaken at 12.40. His blood pressure was 148/59, his respiratory rate was 20 and his heart rate was 120. His temperature appears to have been 37.5°C. As a result of this, and probably as a result of the increased heart rate, he was given an overall PAR score of 3.
- Although it is not clear from the records, it would seem likely that the increase in PAR score from 2 to 3 generated the decision on the part of the nursing staff that a doctor should be informed because the nursing documentation records at 12.43 that the sister was informed and she informed the Registrar.
- Although his note is untimed, it would appear that the A & E Registrar, a Dr Partiban, examined C, presumably a little while after 12.43. The note is very difficult to read, but the consensus is that it records a complaint of pain in the anus "for the last few days" and that he had been "having difficulty passing urine". The note records a rectal examination which demonstrated "mild tenderness laterally", but "no definite abscess" or "no definite ulcer" (it is difficult to determine which). The general condition was said to be "well", that he was alert and that his chest was clear. The diagnosis was "? perianal abscess" and the plan was to refer C to the surgeons.
- C was then seen by the Surgical SHO on call, Dr Uhercik. Again, the note is untimed, but since the time of the request for bloods made by Dr Uhercik (see below) was 14.36, it would suggest that he was seen between about 14.00 and 14.30. Before I describe what Dr Uhercik did, I must refer to a very odd feature of the narrative to this case, whether looked at from C's point of view or from D2's point of view.
- Although the letters of claim were dated November 2014, and despite the fact that C had sent a letter of complaint to the hospital in May 2012 (soon after his discharge from KCH), the fact of the examination by Dr Uhercik (and the record evidencing it) did not emerge until February 2017, some 3 months before the commencement of the trial when D2 disclosed the clinical record. C had made no reference to any further examination after having seen the A & E doctor (see paragraph 37 above) and D2 had itself proceeded on the basis that, whatever that doctor had said concerning referral of C to the surgical team, that referral had not taken place and that C had left the A & E Department before it took place.
- I have alluded to C's letter of complaint written after his final discharge from KCH. Although undated, it seems clear that it was written (with legal assistance) in May 2012 because the hospital received it on 28 May 2012. The relevant part for present purposes was as follows:
- This certainly conveys the impression that the only doctor he saw was the A & E Registrar and that C decided to leave after 6 hours in the A & E Department, having been told that, whilst he could wait for a "second opinion", that doctor's assessment was that there was nothing wrong with him. C did not say in that letter that he had asked the receptionists in the A & E Department what the position was and that he had been told that he had or may have been discharged (see paragraphs 56 - 57 below), but the general sense of the letter was that he was not assessed to be in urgent need of further review. The letter does refer to C being told to "go and sit in the A & E Department", something that does broadly accord with what happened, but probably at a later stage than having just seen the A & E Registrar (see paragraph 56 below).
- At all events, the hospital's response (dated 22 October 2012) to the letter of complaint, following an investigation carried out by the Matron for the A & E Department to which Dr Spencer contributed, was (in relation to the material matters) as follows:
- A letter from the Chief Executive, Mr John Goulston, to C dated 16 October 2012 contains the following paragraph:
- Both those letters reflected what Dr Spencer had said in his letter to the Service Manager of the hospital dated 19 June 2012. That letter contained the following paragraph:
- None of these letters refer to the examination by Dr Uhercik and each comments only on the actions of the A & E Registrar. I will have to return to the significance or otherwise of that in due course, but it is clear that no-one had at that stage found the record made by Dr Uhercik although it was clear from the notes that were available that a referral to the on-call surgical team had been made.
- By the time the letter of claim to D2 dated 11 November 2014 was formulated, C did allege that at about 16.00 on 13 October 2011 he asked the A & E receptionist what was happening and was told that there was no record of any referral of him to another doctor having been made and that, as a result, he left without receiving any treatment. However, the position remained that, from his perspective, he had only seen the A & E doctor.
- The hospital's response to that letter, dated 16 April 2015, was that "the lack of surgical review appears to have been a result of [C] leaving the department."
- This assertion and counter-assertion was carried forward into the pleadings initially exchanged in late 2015 and remained the position until a flurry of amendment and re-amendment in March 2017 after the revelation of the examination by Dr Uhercik.
- The failure to disclose the clinical record relating to that examination until February 2017 was not explained at the trial, but there is no suggestion that it was other than inadvertent. It is not wholly unusual in clinical negligence cases for certain records to "go missing" for a time. Equally, there is no suggestion from D2 that C's failure to mention this feature of the events of 13 October 2011 was in any sense deliberate. It was sensibly and sensitively recognised by Mr Martin that C had been through an extremely stormy passage in the six months I mentioned in paragraph 7 above and the prospect of him recalling accurately the events in those early few days was bound to have been affected by that period. I am sure that represents the explanation for his failure to remember what took place, but there are, of course, two particular consequences of this: first, it does reinforce the need to approach any aspect of his evidence concerning the events of those few days with caution and generally to look for other evidence, whether direct, circumstantial or medical, which might throw light on whether what he asserts now is correct. That is no reflection on his honesty, merely on his reliability as an historian of the material events. Second, it is undoubtedly the case that he was seen by a Dr Uhercik between about 14.00 and 14.30 on that day and the case against D2 and the circumstances in which C came to leave the hospital must be assessed on that basis.
- Reverting to the chronology on 13 October 2011, as I have indicated, according to the clinical records, Dr Uhercik must have seen C between about 14.00 and 14.30. Not surprisingly, Dr Uhercik has no independent recollection of the examination. His notes indicated that he elicited a 3-day history of "anal pain", that C had experienced no shakes or shivers, that he had never had similar pain previously and that there had been no change in bowel habit. Dr Uhercik noted that the heart rate was 120, the blood pressure was 148/60 and the temperature was 38°C, but those results were taken, he confirmed, from the previous observations at 12.40. His note indicates that he performed a digital rectal examination with the clinical observation that there was tenderness at the lateral border of the prostate. This, he noted, was at "10 11 o'clock" which means that the tenderness was noted on the upper right side of the anus. He noted that there were "no palpable masses" and that there were no external signs. He made the differential diagnosis of "evolving ischiorectal abscess/prostatitis", with a question mark against each. He commissioned blood tests for CRP (in other words, C-reactive protein), urea and electrolytes and a full blood count. A raised CRP level is a non-specific marker of infection and inflammation.
- Precisely what happened thereafter is not easy to determine. C did leave the hospital before the blood tests were carried out and the balance of the evidence suggests that he left at or about 16.30. Although there are aspects of the history of what took place that day which were omitted from his first account or accounts (see paragraph 41 above), he has said consistently (and his wife supports him) that he contacted her to go to collect him when he thought that nothing else was going to happen to him by way of treatment or investigation that afternoon. She says that she received a call on her mobile telephone when she was on her way back from collecting their five-year old daughter from school. She explained in her evidence her movements that afternoon and the likely timings and it certainly appeared to be the case that she would have arrived at the hospital at or about 16.15. Her recollection was that she had to go into the hospital, taking the two children with her, to find C in order to bring him home.
- It is, however, what happened before then that is of significance. There are no hospital records which assist and Dr Uhercik, who was first asked to cast his mind back to October 2011 in March 2017 (and thus some 5½ years after the material events), has no independent recollection of anything that took place. He has had to rely upon his notes and upon what would have been his usual practice. None of the receptionists have any specific recollection of what happened and C has no recollection of the examination by Dr Uhercik.
- A number of things can be said with a degree of certainty: first, Dr Uhercik will have seen and examined C in a cubicle since he performed a digital rectal examination and that would only have been conducted in the privacy of a cubicle. This is consistent with the document referred to in paragraph 31 above. Although C says that he does not recall ever being in a cubicle, I think his recollection must be wrong in that regard. Second, Dr Uhercik would plainly not have intended to discharge C because there were outstanding results from the blood tests to be reviewed before deciding what, if anything, to do further. What he recorded in his clinical note was transposed to the Pathology Order Form which indicated that the clinical details were "perianal pain", and "? abscess ? prostatitis". It does seem to me more likely than not that Dr Uhercik told C that he wanted the blood tests carried out in order to decide what to do next, but I do not think he could have said this with enough emphasis to ensure that C knew what might happen thereafter. I will return to this below (see paragraphs 55 and 186).
- Whatever Dr Uhercik said must have been said at or around 14.30. His belief is that he would have left C in the cubicle after the examination. If C was moved subsequently, that would have been a decision for the nursing staff. This seems more likely than not to have been the case. The evidence that leads me to infer that this took place after C was seen by Dr Uhercik is that the reference to him being in cubicle 4 in the majors section (see paragraph 31 above) on the CAS form retained by the surgical unit was crossed through and the letters "WR" inserted next to the deleted entry. "WR" stands for waiting room and, according to Mrs Ashley (see paragraph 58 below) it would have been written by someone in the surgical unit to indicate that C had been moved. (The same deletion did not appear on the CAS form retained in the A & E Department.)
- I have already questioned the impact made on C by Dr Uhercik's communication to him that he wanted the blood tests performed. C's evidence, which is largely mirrored by the clinical notes for the day in question, is that he was in considerable pain and discomfort in the area of his anus throughout the whole day. He was taken in an ambulance to hospital because of pain in that region and because he was not feeling at all well. However impatient he may have become, it is very difficult to believe that he would have left the hospital if he thought that there was a further diagnostic test to be carried out which might have led to some treatment to relieve the pain which he had scored as 9 earlier that day. His wife might also have wanted to know why he was leaving the hospital if there was a relevant test outstanding. Whilst, as I have said, it seems more likely than not that Dr Uhercik did say to C that he wanted to see the result of the blood test, I think it is also likely that this was not said with much emphasis and did not make much of an impact on C who had by then been in the hospital for 4 hours in, what I am prepared to accept, was considerable pain and discomfort. It is fair to say, though it is of marginal relevance, that Dr Uhercik did not record in the clinical notes his plan for C, but it is tolerably clear that the next step would depend on the results of the blood test. I do not believe C had appreciated that.
- The essential thrust of C's letter of complaint (see paragraph 40 above) was that he was in so much pain that he did not want to wait sitting in the A & E Department for the "second opinion" he said he was told to await. I can accept that an expression like "second opinion" might have been used by Dr Partiban because that was, in effect, what he was suggesting should happen when C was referred to the surgical team. Equally, it is, I suppose, possible that Dr Uhercik said something like this, thinking that the surgical registrar might have to review the position once the blood test results were available. However, if it was Dr Partiban who referred to a second opinion, I consider it unlikely that he (who was called to see C because of the increase in his PAR score) would have told him to get off the trolley, leave the cubicle and go to sit in the A & E waiting area whilst awaiting that opinion. As I have indicated, I think the same applies to Dr Uhercik (see paragraph 38 above). I have already concluded that C was asked by the nursing staff to leave the cubicle and go and wait in the A & E waiting area, but that occurred after he had been seen by Dr Uhercik. It is impossible to say precisely when that occurred, but I can understand, on the basis that he was still experiencing anal pain, that this was very uncomfortable. He was waiting there for blood tests (which he may have thought had been ordered on his admission to hospital, which they were: see paragraphs 26 - 27 above), but the tests did not materialise. I consider that to be the most likely background scenario in the lead up to him leaving the hospital as well as being told something by the receptionists that suggested there was no further investigations to be carried out.
- I do not consider that the reception staff told him positively that he had been discharged; that would be well beyond their remit. However, it is possible to see why a receptionist in A & E who was asked by C what was to happen to him next might look at such notes as there were available and indicate that they did not suggest that he was due to be seen by anyone else. The records are lacking in a number of respects (see further at paragraphs 163, 166 and 182 below), but that seems to me on the evidence to be the most likely explanation.
- There is a further unexplained entry in the hospital records which might have a bearing on what occurred that afternoon. On the original CAS card (namely, the one retained in the A & E department), there is an entry timed at 14.00 with the letters "DNA" beside it. That was written by someone within the A & E Department and must be taken to indicate that C did not attend something that whoever wrote it must have been expecting him to attend. It cannot have been for the blood tests ordered by Dr Uhercik because they were not commissioned until after 14.30. Mrs Ashley, who was an A & E receptionist at the time, believes that it would have been a member of the clinical staff who would have written this entry. It is an odd entry because as from the end of Dr Partiban's examination of C, he was to be transferred to the surgical team and there was nothing, certainly at that stage, left for the A & E Department to do. The only outstanding matter was the carrying out of the blood tests commissioned by the Triage Nurse (see paragraphs 26 - 27 above). It is impossible for me to make any meaningful finding about what the entry related to other than to say that it was possibly entered by a nurse or phlebotomist who had come eventually to take the blood sample.
- However it came about, C did leave the hospital that afternoon and went home at about 16.30. I will return to the implications of this later (see paragraph 182 et seq), but I do not consider that his decision to do so was a fully-informed decision.
- His account is that he had "a pretty rough night", "couldn't sleep and was in dreadful pain". As a result he telephoned the GP surgery in the morning and, according to him, "secured an appointment". His recollection is that this was not a pre-arranged appointment from the Wednesday (see paragraph 16 above) and I have accepted that recollection. His account is that he told D1 that he had a terrible pain the rectum, that he was constipated and that he was having difficulty passing urine.
- D1's note begins by noting that C had been "seen yesterday" (which cannot have been a reference to C's attendance on 12 October), but then the words "telephone consultation and [antibiotics] given and came to pick [up] that day" appear. There is no reference to C's attendance at the Mayday Hospital the day before. D1 says that he would have recorded it if told about it; C says he told D1 and that he has assumed that the reference to "seen yesterday" referred to that attendance.
- The note continues "today feeling pain in lower abdomen and says that he is constipated and [has] difficulty in passing urine". It adds that he has taken "co-codamol up to 8 or 10 in a day". It was noted that he was not vomiting and was not sick. His temperature was recorded as 37.5ºC, his blood pressure as 120/70 and his blood sugar as 8.2. His weight was recorded as 133 kgs, nearly 21 stone.
- The note indicates that D1 carried out a rectal examination which simply indicated that the rectum was "empty". C says he does not recall that, but does recall being in tremendous pain; indeed he effectively denied that a rectal examination took place because he said he was in so much pain he would have remembered it. He believes he could not have tolerated a rectal examination. The note does not record "rectal pain" nor does it record an abdominal examination, but D1 said in his witness statement dated 29 June 2016 that C told him of "new symptoms of constipation, difficulty passing urine and lower abdominal pain." He did not, according to D1, "repeat his concerns regarding the 'flu-like symptoms of which he had complained 2 days earlier." D1's witness statement indicates that, in addition to the rectal examination, he did perform a "full abdominal examination" which revealed "some discomfort but no tenderness or guarding". This is not recorded in the notes. Equally not recorded in the notes is the suggestion that he asked C to supply a urine specimen, but he was unable to do so as he had just passed urine. That appeared in his witness statement.
- D1's witness statement says that C was accompanied by his wife, something he repeated and enlarged upon in his oral evidence. She is adamant that she did not accompany him into the surgery: she remained in the car, she said, with her small daughter. She did say that C was in considerable pain.
- For the first time, when being cross-examined, D1 revealed that he had carried out a full chest examination as well as the full abdominal and rectal examinations to which I have referred. His explanation for there being no record of it in the notes was that it was a lengthy consultation and a busy morning and he did not have the time to record it. He also said that it revealed no abnormalities and he often did not record "positive findings". He accepted that he should have recorded the discomfort revealed during the abdominal examination. He said that his view was that the constipation and the urinary symptoms were causing this discomfort.
- Reverting, for the moment, to what is recorded in or can be deduced from D1's note, he advised C to drink more fluids and to take paracetamol rather than co-codamol "as it causes constipation". He also prescribed Trimethoprim tablets and a Lactulose solution. The former is an antibacterial medicine used to treat urinary tract infections and he confirmed in his evidence that that is what he thought was causing the difficulty in passing urine. Lactulose is a laxative used for treating constipation.
- The precise time of this examination is unclear. D1 said it was about 10.00, but no appointment record was produced to confirm this. C thought it was nearer midday.
- It is obviously of some concern that D1 gave a much fuller picture, as he recalls it, of the examination than his notes reveal. Mr Maskrey suggested positively to him that he had "made up" the account of carrying out a chest examination because he had realised that it would have been completely wrong not to carry out such an examination on someone who, only two days before, had presented with what he (D1) had thought was a chest infection requiring antibiotics. D1 denied this strongly. I do not think that D1 was being deliberately dishonest about this, but I do think that there was an element of him persuading himself that he "must have" performed the chest examination because it was illogical for him not to have done so. Whether he did or he did not do so is not material to the outcome of this case, but evidence of this nature does mean that the fact-finding mission of the court must be approached with a degree of caution when it comes to placing reliance on D1's account of events.
- My essential approach, given this background, is to attach more significance to what is in D1's notes than what is not in the notes when credibility and reliability issues relating to the clinical course of events are concerned. There has been no suggestion that D1 has altered his notes more accurately to fit with what is now known. The nearest Mr Maskrey came to making any such suggestion was when he put to D1 that "if [he] performed a rectal examination, it was a cursory one and not an examination that checked for mass or tenderness of the buttocks and around the anus" (my emphasis). I will deal with the quality of the examination and the conclusions to be drawn from it later (see paragraph 205), but I do not doubt that some form of rectal examination was carried out. I think it unlikely that C's wife was present, even on the other side of the curtains in the consulting room, as D1 suggests. This was not recorded in the note and was not asserted in the response to the letter of complaint which had been sent in May 2012. I will return to the issue of whether C made a positive complaint of rectal pain in due course (see paragraph 151).
- At all events, just as the time of the examination on 14 October (and some aspects of it) is (and are) uncertain, the precise timings of various events later that day are also uncertain. (I will revert to what C has said about his dealings with D1 below: see paragraphs 205 - 210). The only certainty is that at 23.52 that evening an ambulance was called to an address in SE19 (where C's wife's sister lived) and it arrived at 00.22 on 15 October. I will deal with the immediate observations undertaken by the ambulance crew and on admission to KCH and the course of events thereafter below (see paragraphs 73 - 95), but the events leading to the call for the ambulance fall to be considered first.
- Mrs Macaulay was due to help her sister prepare for a catering engagement. This had been planned for some months. Because of the timings involved, it was not immediately apparent what this arrangement required in practical terms when this evidence was first given. However, she explained in her oral evidence that the catering was required for an event of a religious nature the following morning and the cooking had to be done overnight. The children of both families would sleep at her sister's property overnight. Because C was in such pain, she said she wanted to abandon her plans, but he insisted she went ahead.
- The combined evidence of C and his wife is unclear about the precise build-up to the calling of the ambulance, but they suggest that he was in considerable discomfort on the journey from home to SE19. Since there was far less emphasis on rectal/anal pain and much more emphasis on abdominal pain in the notes when C went to KCH later that evening/in the early hours of the next day, I am not sure that I can accept the evidence that it was primarily from that region that most of the pain emanated. I do not doubt that he was in some general discomfort. Nonetheless, the contemporaneous records indicate that he started to feel pain again at about 18.00 that evening (see paragraph 73 below).
- Whatever the precise background, the ambulance arrived at 00.22. The notes made by the ambulance crew reveal that C walked downstairs to the lounge, the record indicating that his wife and "son" were present. Apparently, C's wife's sister has a son and that is possibly the reason for this entry. The presenting complaints were "back pain", "urine retention", "hypogastric abdominal pain" and "constipation". It was recorded that he had experienced those complaints for six days. Reference was made to the fact that he saw his GP who had prescribed antibiotics which caused a "reaction" in the form of a "skin rash" and the medication was thus "discontinued". It was noted that two days previously he had "pain again" which prompted the call of an ambulance and his attendance at the Mayday Hospital. The note says that he was discharged with "further antibiotics". It continues with a note to the effect that he experienced "pain again tonight" which led to the calling of the ambulance. The onset of the symptoms was recorded as being at 18.00.
- The examination conducted suggests that ABC (airway, breathing and circulation) were "clear", that there was haematuria (blood in the urine) for six days and that the urine had a "strong smell/colour". It was, however, recorded that the patient "[had been] unable to urinate for [six days]". The note said that an inconsistent history had been described. In relation to the abdomen, it was noted that the patient was "morbidly obese" and that it had been impossible to palpate the abdomen because the patient declined "due to pain". It was noted that C was "dissatisfied with Mayday" and, at his request, was conveyed to KCH.
- In relation to the usual observations, his pulse rate at 00.25 and 01.00 respectively were 115 and 121, his blood pressure 98/67 and 102/71, his temperature at 00.25 was 37.1 and his blood sugar level was 7.3. The words "not understood" were put against the pain score. His Glasgow coma score was 15.
- During the period when the ambulance crew were present in the property, Entonox (the well-known pain-relieving agent) was administered at 00.50, shortly before the ambulance departed with C at 00.54. The ambulance arrived at KCH at 01.08 and the clinical handover was at 01.16.
- As Dr Campbell-Hewson observed in his report, the timings in the KCH notes are difficult to follow because it appears that the medical assessment took place twenty minutes before the triage assessment. On one view, indeed there appear to be two different triage assessments. Nonetheless, at 01.14 there is an initial assessment which notes a one week history of "pain upon urination, haematuria, constipation, ? haemorrhoid, urinary retention for [3 days]". There is also reference to abdominal pain. The other assessment (which is positively identified as a triage assessment) is timed at 02.00 where the history is said to have been that C's symptoms "started with headaches on Friday, then had flu, then [abdominal] pain started yesterday when passing urine, complains of stinging." At that stage his respiratory rate was 28, blood pressure 88/49, pulse rate 125, temperature 36.8 and a blood sugar level of 5.6. The note indicates that he was short of breath on exertion. The POTTS ('physiological observations track and trigger system') score was 5. His oxygen saturations were reduced at 94%.
- There is an untimed entry in the clinical records (which appears to have been completed by the Senior Staff Nurse in the Emergency Department), but before the entry at 01.40 referred to below, indicating that a 'FAST' scan was done and that, following a discussion with the Registrar, C was to have a CT scan of the abdomen. The entry at 01.40 (completed by a doctor) records a two-day history of lower abdominal pain radiating to the back. It was recorded that there was "no vomiting, no diarrhoea/constipation, no urinary symptoms." The observations revealed identical findings to those referred to above for respiratory rate, oxygen saturations and blood pressure. The heart rate was 134 bpm. The examination revealed that his abdomen was distended and tender in the suprapubic region, both in the right iliac and left iliac fossa regions. C was "guarding +", but the bowel sounds were normal.
- The impression was of an abdominal aortic aneurysm ('AAA') or a perforation. An urgent CT scan was to be carried out.
- There is a note of a verbal report on the scan added to this record which was that there was no abdominal aortic aneurysm, but there was "free gas in [the] pelvis tracking up [the] abdomen" and the expression "? small bowel perforation" was also added. That note was enlarged upon in the full written report, the relevant parts of which were in the following terms:
- I will return to the imaging at a later stage when dealing with the evidence of the radiological experts. I will describe the features of necrotising fasciitis at a later stage too (see paragraphs 105 - 106).
- It is not entirely clear when that report was available, but its general thrust was obviously known by the clinicians relatively early. The Senior Staff Nurse in the Emergency Department was pressing for a surgical referral and C was indeed seen by the Surgical SHO on call at 03.45 and he noted that he had discussed the results of the CT scan with the duty radiologist. C was seen by the Surgical Registrar at 04.00 who also noted the result of the scan. The SHO noted a left indurated lump in the perianal region and the Registrar also noted induration though its location is less clear from the note. The SHO's provisional diagnosis was expressed as "? perianal abscess and sepsis". He did record that C said that he had developed left lower abdominal pain, with gradual onset, 5 days previously, something C apparently repeated to the Registrar. This is rather different from the history given at the Mayday Hospital on 13 October when no reference was made to abdominal pain (see paragraphs 22 50 above) and I will revert to this later (see paragraph 153).
- By the time of the Registrar's examination at 04.00 the results of the blood tests taken at 01.53 were available which, inter alia, showed a creatinine level of 237µmol/L (the upper limit of normal being 120 µmol/L) and a platelet count of 118 which is low. He noted that the patient reported a 5-day history of abdominal pain, but a little lower in his note he recorded "developed pain in perianal region" which was then followed by a note reading "abdominal pain". The Registrar's impression (which largely mirrored that of the SHO) was of sepsis, the origin of which was in the perianal region.
- The plan at that stage was for debridement and incision and drainage of the perianal abscess/induration. C was put on intravenous fluids and antibiotics and directed to be nil by mouth. He was also to be the subject of an HDU ('High Dependency Unit') review. He was transferred to the Liver Intensive Therapy Unit (LITU) at 09.00. The notes seem to indicate that he went almost immediately to theatre. Indeed in a letter to Dr Ansari, the principal in the South Croydon Medical Centre dated 27 October, Dr Christopher Willars, Consultant in Intensive Care Medicine in the LITU, confirms this and the letter contains a helpful summary of the events leading up to and including the initial surgical intervention:
- The letter also indicated the very serious position that existed when C arrived in the Liver Intensive Care Unit. There was, he recorded, "significant metabolic derangement" and a "significant ischaemic hepatitis and coagulopathy." He was treated in accordance with the Unit's established approach to dealing with "acute liver failure". Dr Willars recorded that, given the need for "substantial circulatory support and dialysis in the context of septic shock and profound metabolic disarray", his wife was told that the prognosis at that time "was uncertain and death was a possible outcome."
- Whilst the subsequent history is not directly relevant to the issues that I have to resolve, as indicated previously (see paragraph 7 above), C had a very difficult period for the next 6 months or so.
- Dr Willars summarised what occurred in the initial surgery. What was discovered radiographically before the surgery and what was discovered during the surgery are matters of potential significance in determining precisely the underlying condition that led to the ultimate admission to hospital. I need, therefore, to elaborate a little on Dr Willars' summary. I will do so by reference to the operation notes (see paragraphs 88 - 89 below), but it is informative to see how Dr Willars' colleague, Dr Julia Wendon, Clinical Director for Critical Care in the LITU, described the position in a letter to Dr Ansari dated 8 November 2011. She said that, having gone to theatre, C "underwent debridement and subsequent packing of an ischiorectal cavity and abscess" and that he also underwent "laparotomy and formation of a defunctioning colostomy." She repeated what Dr Willars said, namely, that he was "left with an open abdomen" which was appropriately dressed whilst it remained open. When he returned to the ITU "he was significantly unwell" and the "clinical picture was that of profound septic shock with an ischaemic hepatitis." Her letter contained a list of diagnoses (a list that was repeated in subsequent letters) which began with the first two in the list of "septic shock" and "ischiorectal abscess with spreading sepsis and gas tracking into the pelvis". It is, of course, to be observed that it is essentially this latter explanation of the aetiology of C's condition for which his legal and medical teams contend in these proceedings.
- The Operation Sheet indicates that a cruciate incision was made over the left iliac fossa. Professor Sells describes the incision as a cross-shaped incision which was made in the left buttock. This revealed an ischio-rectal cavity of approximately 15 20 centimetres extending up to the root of the scrotum. The note records "no pus" and "some necrotic tissue".
- Another part of the Operation Sheet dealing with the midline laparotomy, records "pus +++", described as "foul smelling", having been found in the "ante-bladder pre-prostate area". The note continues by recording that the pus was drained, the cavity was irrigated with saline and that "some necrotic tissue [was found] on the wall of the bladder." A large drain was inserted into the retropubic area. The following was also noted:
- That note is of potential significance because Ms Mishcon suggested to Professor Sells that if there was no communication between the retropubic and perianal areas, pus could not have tracked upwards from the perianal area into the retropubic region. Professor Sells did not accept this and I will return to the issue later (see paragraphs 142 - 150 below).
- One further matter of potential significance is that, following further surgery on 19 October 2011, C's sigmoid colon was resected and an end colostomy was created. Subsequent histological examination of the sigmoid colon showed an area of perforation measuring 30 mm which was 110 mm from one resection margin, the adjacent bowel appearing "dusky and necrotic for an area of approximately 50 mm proximally and distally from the area of perforation." It was noted that "[diverticular] disease is not seen." The microscopic details given in the histology report indicate that the specimen shows "extensive ischaemic necrosis involving the full thickness of the mucosa and focal submucosal necrosis." It is said that there is "nodular hypertrophy of the muscularis propria with features of diverticular disease."
- Before turning away from the chronology of events, it is to be noted that by 8 November (when Dr Wendon wrote her letter: see paragraph 87 above), C was said to be "fully orientated and is communicating with his family." That would seem to be confirmed by a note in the GP records which record a telephone call made to Dr Ansari by C's wife on 22 November 2011. The precise accuracy of what she said must be open to question because it is a second-hand account of things said to her by C (or indeed by people she spoke to at the hospital) at a time when C must have been very distracted by his circumstances.
- Translating the note into narrative form, it referred to the fact that C had seen D1 "several times", that he "had abdominal pain", that he could not pass urine and suffered from constipation. It was recorded that he had "retention". Reference was made to the fact that Lactulose was prescribed. The note refers to the suggestion that on the day he went to the A & E Department at KCH he had been complaining of "severe abdominal pain". C's wife appears to have passed on the perception (either his or that of someone to whom she spoke at the hospital) that his underlying problem was an abscess in his abdomen. She told Dr Ansari that the Claimant wanted to know the circumstances of his admission.
- Although D1 said in evidence that he became aware of this telephone conversation at or about the time it was received, there is no record at that stage of his response to it. It was not until the formal complaint was made in May the following year (see paragraph 69 above) that he set out in written form his recollection.
- That comprises a recitation of the factual history so far as it emerged from the evidence and notes made at the time. There are uncertainties in the history and the question arises as to whether the expert evidence can throw any light on how those uncertainties can be resolved.
- As I have indicated (see paragraph 87), the position seemed relatively straightforward from the point of view of the treating physicians at KCH: what they perceived that they were dealing with, based upon the CT scan, began as an ischio-rectal abscess with consequent sepsis, the development of necrotising fasciitis and the production of gas that tracked into the pelvis. The sepsis was such that C was in septic shock at the time of admission (evidenced by low blood pressure and a rapid pulse rate) and he was in a perilous state for some time thereafter until his situation was stabilised. It does not appear that anyone questioned this diagnosis and construction of events at the time, although it has to be observed that there would have been no reason necessarily to do so at the time given the need speedily to try to resolve the very serious position that C was in.
- The starting point, namely, of an ischio-rectal abscess was along the lines of the provisional views expressed by Dr Partiban and Dr Uhercik on 13 October.
- Until Professor Winslet formulated his opinion (see paragraph 109 et seq below), the suggestion that C's problems began with an ischio-rectal abscess had not, as I understand it, been questioned on behalf of D1 or D2.
- However, the joint position now taken by both defendants in relation to the aetiology of C's condition is, as I have indicated, derived from the opinion of Professor Winslet. He was instructed on behalf of D1, along with Professor Cartwright and Dr Bell, to express an opinion about causation. He was not originally instructed by D2 either to express an opinion about causation or about breach of duty. The expert opinion from the perspective of a colorectal surgeon for D2 was given by Professor Phillips and that related solely to breach of duty. I am unaware of any report for D2 on causation other than knowing that by the time the pleadings of both defendants were amended in November 2016 (see paragraphs 110 - 111 below) to assert what was in effect Professor Winslet's view, D2 was adopting Professor Winslet's position also. By the time of the joint discussion between Professor Winslet and Professor Sells in April 2017, Professor Winslet was recorded as being an expert on the issue of causation for both D1 and D2. Had D2 put forward an expert report taking the position that Professor Winslet took, it would have involved taking a different position from that taken by the treating physicians and surgeons at KCH and, at least to some extent, from the provisional views of Dr Partiban and Dr Uhercik who saw C at the Mayday Hospital on 13 October 2011.
- At all events, whatever the background to the emergence of this part of the defendants' cases, the case itself must be considered.
- Some understanding of the anatomy of the region is necessary to appreciate the nature of the argument. Ms Mishcon helpfully produced some diagrammatic representations of the male anal region taken from the Internet, one of which I reproduce as Appendix 2 to this judgment.
- Although not labelled as such on this diagram, the ischio-rectal fossae are the slightly grey areas of (in a two-dimensional representation) a broadly triangular shape bordered on one side by the levator ani muscle and on the other by the obturator internus muscle. The base of the triangle is the perineum.
- Each ischio-rectal fossa contains fat and supports the other structures in the region. If part of the ischio-rectal fossa becomes infected and pus develops, an abscess can form if the pus is confined to a particular area. Where this occurs, gas may be found if the abscess perforates. The presence of gas may also evidence the presence of a bacterial organism.
- A diverticulum is a small bulge or pocket that develops in the lining of the colon. The plural of diverticulum is diverticula. Where someone has colonic diverticula he/she is said to have diverticulosis. Diverticulitis is the expression given to the condition when diverticula become inflamed or infected. Where a diverticulum becomes, or diverticula become, inflamed and infected, pus can form and if confined in a particular space an abscess is said to be formed. An infected or perforated diverticulum may produce gas.
- Necrotising fasciitis ('NF') is a form of gangrene and sometimes popularly called a "flesh-eating disease". It starts with a wound infection (such as that which gives rise to an abscess) the bacteria from which spread rapidly through and destroy the fascia by the release of toxins. The fascia is a layer of the body's connective tissue. The tissue becomes necrotic and liquefies into a greyish liquid that is often referred to as "dishwater pus". NF is extremely serious if unchecked and leads to septic shock.
- A rather more detailed and authoritative description appears in a review article published in 'Frontiers in Surgery' in September 2014 entitled 'Current concepts in the management of necrotizing fasciitis' produced by Dr Power, the Introduction containing this passage:
- The meaning of the words "proximally" and "distally" are important in understanding the opinions expressed. "Proximal" means closest to and "distal" means farthest away from some anatomical point. For the purposes of this case, the word "proximally" is used effectively to mean higher up, in other words, further away from the rectum. "Distally" means lower down and closer to the rectum.
- The levator ani muscle (which is depicted on the diagram in the Appendix 2) is a muscle that forms part of the pelvic floor, in other words, the floor of the pelvic cavity.
- In the circumstances to which I will refer, it does appear that Professor Winslet's opinion developed in terms of its detail over a period of time. Professor Winslet himself accepted that, having been instructed to provide an opinion, he thought it appropriate to "think outside the box" and, having done so arrived at the hypothesis to which I will refer in more detail. With, in my view, some justification, Mr Maskrey has complained about the way the case to which C has had to respond has developed based upon this emerging opinion. That will become apparent as I identify the stages in the process.
- In D1's Amended Defence dated 3 November 2016 it was asserted, for the first time, that "[for] the avoidance of doubt, it is [D1's] case that [C] was not suffering from a perianal/ischiorectal abscess on 12 October 2011." The particulars given under the heading 'Particulars of Causation' were, in the material respects, as follows:
- D2's Amended Defence, also dated November 2016, averred that C's condition was "an occult pelvic infection (probably caused by a perforated diverticulum), rather than simple perianal/ischiorectal abscess."
- In Professor Winslet's report dated October 2016 (the substance of which was apparently available to the defendants in June 2016), and upon which the foregoing amendments to the pleadings were doubtless made, the relevant view on causation was expressed as follows:
- It is to be noted that at that stage Professor Winslet was relying upon the CT scan obtained at KCH on 15 October for the proposition that there were diverticula in the rectum and sigmoid. Although not said expressly in the passage of the report quoted, the inference (and indeed the case pleaded) is that he was saying that the likely cause of the pelvic sepsis was a perforated diverticulum. The report on the CT scan (see paragraph 80 above) does not, of course, say that there is evidence of a perforated diverticulum and contains the opinion that there was "[no] convincing sign of intestinal perforation".
- Before turning to Professor Winslet's Supplementary Report, it is, perhaps, helpful to note the position of the radiology experts who have given evidence, Professor Steve Halligan (on behalf of C) and Dr Hartley Euinton (on behalf of the Defendants). From a purely radiological imaging perspective, they were substantially agreed on all issues. These can be summarised as follows:
- Professor Halligan does add a factor for consideration, based upon his experience, to which I will refer in paragraph 116 below, but the "pure" radiology evidence is substantially agreed and affords no evidence to support a bowel perforation and/or a perforated sigmoid diverticulum.
- Professor Halligan said in his report and repeated in the joint statement with Dr Euinton that he had encountered necrotising fasciitis of the perineum/anus/rectum/pelvis in both his personal clinical and medico-legal practice and that the features of free gas combined with its distribution in the present case "suggest necrotising fasciitis" and that "the absence of imaging features of perforated diverticulitis weigh heavily against this being an initiating factor". Professor Halligan also said that the CT scan demonstrated free gas within the roof of the ischiorectal fossa bilaterally, something which he said would be "exceptionally rare if the primary pathology was diverticulitis."
- Following the emergence of the notes relating to Dr Uhercik's examination, Professor Winslet added these observations in a Supplementary Report dated 9 March 2017:
- These two reports were, of course, available before he and Professor Sells held their joint discussion on 5 April 2017 and represented the full extent of Professor Winslet's opinion on this issue. Professor Sells produced a report on causation dated February 2017 which commented (a) on the Amended Defences advanced and (b) on Professor Winslet's first report. He disagreed with Professor Winslet's view. In cross-examination he was later to accept that some of the factors upon which he relied were factually incorrect, but he did make the point that, according to the records, symptoms of abdominal pain (and thus symptoms of diverticulitis) were not the presenting symptoms on 13 October. The essential complaints that day relating to pain were complaints (going back over a few days) of pain in the rectum and anus.
- As will be apparent from the quotation from his first report (see paragraph 112 above), the starting point in Professor Winslet's analysis is that when C presented to the A & E Department on 13 October, there were no symptoms "localised" to the anus, perianal or ischiorectal areas. Indeed, when he gave his oral evidence, Professor Winslet emphasised that the day before (on 12 October) there were no complaints made of anal or rectal pain: the complaint was of generalised feverish symptoms and on the following day pain in the hip and back. That latter aspect, he said, was atypical of the presentation of an ischiorectal sepsis and far removed anatomically from a perianal or ischiorectal sepsis.
- As he explained in his oral evidence, Professor Winslet's perspective was that C's presentation at various times was "variated". He accepted that the references in the clinical records to anal or rectal pain could be compatible with perianal or ischiorectal sepsis, but these symptoms, he said, could occur with other pathologies as well. He did not identify precisely what the relevant alternative pathology for the anal or rectal pain was in either his original report or his Supplementary Report. In the Defendants' Agenda for their joint discussion, he and Professor Sells were asked whether they agreed that C's "reported pain in the rectum/anus could be attributed to referred pain from an infective/inflammatory process higher within the pelvis generating irritation of nerve roots or proctalgia fugax from irritation of the levator ani muscle." Professor Sells agreed that an infective process "higher in the pelvis may uncommonly generate irritation of the nerve roots and pain", but said he was unaware "of any evidence that proctalgia fugax is a common presentation of pelvic infection." Professor Winslet agreed with the proposition in the question, namely, that the reported pain "could" be so attributed. There was no further discussion about this between him and Professor Sells and it was not until Professor Winslet gave his oral evidence (when, as it happens, Professor Sells was not in court) that what appeared to be a positive suggestion that the episodic anal pain was caused by, or was a manifestation of, proctalgia fugax was first made. Professor Sells was not cross-examined about this suggestion and so I do not have the benefit of an informed debate on the issue between the surgical experts.
- Ms Mishcon said in her closing submissions that the expert intensivists "agreed with this hypothesis in their Joint Statement", the hypothesis being that proctalgia fugax was the most likely explanation for the reported complaints. I will refer to this agreement below (see paragraph 126), but for the reasons I will give I am not sure that I can give it as much weight as she would suggest.
- The expression proctalgia fugax had not appeared in any of the expert reports on either side. However, significantly it did not appear in the report of Dr Dominic Bell, the Consultant in Intensive Care/Anaesthesia instructed on behalf of D1. The furthest he went in that report can be seen from these paragraphs where he posited the compatibility of the recorded complaints in the rectum and anus with "referred pain from nerve root irritation in the lumbosacral plexus":
- He repeated a few paragraphs later in the report something said earlier, namely, that the issue warranted "definitive resolution by surgical experts".
- In his Supplementary Report, Dr Bell said this:
- As will be apparent, Dr Kenneth Power, the Consultant in Anaesthesia and Intensive Care instructed on behalf of C, did not mention proctalgia fugax in his report (or indeed irritation of the nerve roots arising from an infective/inflammatory process higher in the pelvis) as being possible reasons for the anal/rectal pain and, to the extent that he commented on Dr Bell's overview of the pathology involved in C's case, he said that "these were very much surgical issues" on which he would defer to his "co-experts in surgery".
- Somewhat surprisingly against that joint background, they gave what appears to be a definitive answer to the following question as indicated:
- That agreement does, of course, relate to the "reported pain in the rectum/anus" (my emphasis), but what that reported pain constituted is not described in any detail. The overall problem, as I see it, with the way the evidence about this issue has emerged, given that there has been no informed debate about it and no literature produced to assist, is that the fullest description given to the symptoms of proctalgia fugax that I have received is that the person affected experiences "fleeting pain" in the anus or rectum. This was how it was described by Professor Winslet and by Dr Budd, who is D1's GP expert and who apparently has some experience in its diagnosis. Dr Bell does not describe it. However, I was not told what period of time constitutes "fleeting" for this purpose or how severe the pain generally is. As things stand, I must take the word "fleeting" for what it is, namely, descriptive of something that is transient and passes quickly.
- The question is whether that is what C experienced. If, for present purposes, one leaves out of account his more recent descriptions of the intensity of the pain and focuses on what was recorded at the time about his complaints in this regard (see paragraphs 22 - 50), I do not consider that the rectal pain was "fleeting". I can accept that its intensity fluctuated to some extent and that at times it did not wholly dominate his symptomatology, but I am unable to find on the evidence that it ever went away fully once it began although by 14 October it had undoubtedly ceased to be the dominant focus of pain. I cannot see, therefore, how that pain can be described as "fleeting". In my view, it over-states the meaning of the record that "his back and hips [were] painful" (see paragraph 34 above) to say that he was primarily complaining of pain in those regions given that shortly before and shortly after he is recorded as complaining of pain in the rectum. Furthermore, Dr Partiban conducted a rectal examination. Why would that have been carried out if there was no complaint of pain in the rectum? The same question, of course, arises in relation to the examination by Dr Uhercik.
- I have obviously looked at the issue of whether this aspect of Professor Winslet's hypothesis helps me to form a view about the nature of C's actual complaint and whether it assists in forming an opinion about his evidence when he emphasises, as he does, that a pain in the bottom was his principal concern. This represents part of the overview to which I referred in paragraph 8 above. Whilst there is an element of circularity about it, I do not consider that it does demonstrate that the pain in that area was secondary to pain in the back and abdomen or that it emerged later rather than earlier in the chronology of the material days in October 2011, indeed the chronology is the reverse of that.
- That represents one difficulty with the aetiology for which Professor Winslet contends. Another problem is that none of the radiological evidence supports the existence of a perforated diverticulum in the pelvis (paragraphs 113 - 114 above). Professor Halligan, whose expertise is not in doubt and who was plainly well known to and respected by Professor Winslet, said, in response to a suggestion from Ms Mishcon that a "very small perforation of [a] diverticulum [would not] necessarily show on a CT scan", that a CT scan is "exquisitely sensitive for extraluminal gas, so that fractions of a [millilitre] can be demonstrated with pretty much utmost certainty." The conclusion, therefore, must be that, if there was a perforation of a diverticulum, it would almost certainly have been picked up on the CT scan. It was not so identified. Furthermore, there is nothing in the operation notes, completed by the surgeons who carried out the surgery, that evidences the existence of such a perforation.
- Ms Mishcon has submitted that the histology report (see paragraphs 91 - 92 above), which refers to "features of diverticular disease", directly contradicts the agreed evidence of the radiologists. I believe she made this observation in the context of being critical of Professor Sells' evidence and not as a suggestion that I should disregard the considered evidence of the radiologists. Neither was asked when giving their evidence questions that suggested that the histology evidence "trumped" the radiological evidence despite what might have been thought to be a suggestion to that effect by Professor Sells. Professor Halligan said that the features referred to were only seen on microbiology and that fitted with CT images of "very minimal diverticulosis".
- I have referred to Professor Halligan's expertise already (see paragraph 130 above). When cross-examined by Ms Mishcon, he said that, the imaging features that he saw were "overwhelmingly in favour of a necrotising fasciitis with an anal or perianal origin." He said emphatically that the images, in his view, conveyed an "overwhelming diagnosis [of] a synergistic infection of an event that started around the anus." In his report, he said that he reached this conclusion "on a very large balance of probabilities", which he explained meant that every time he saw images similar to those on 15 October 2011, he would regard them as showing necrotising fasciitis.
- Whilst this view has to be seen from purely the radiological perspective, it was very persuasive evidence from a distinguished expert that I have not seen convincingly refuted by other evidence in the case.
- Whilst neither of the two particular factors to which I have drawn attention (the radiological evidence and the unconvincing suggestion of proctalgia fugax) is definitive from the point of view of a clinician looking for a "unifying hypothesis that explains both symptomology, signs, investigations and the operative finding" (as Professor Winslet described it), when a court looks at the totality of the evidence and applies the balance of probabilities test, each combines with the other to diminish the prospects of the hypothesis being the likely explanation for what occurred: there is no identifiable triggering mechanism for the infection and the proffered explanation for one of the consequences of the suggested triggering mechanism does not in any event marry up with the contemporaneous evidence about those consequences. If anything, the contemporaneous records suggest that the pain in the abdomen was first experienced after the rectal/anal pain had emerged which, though he is not enamoured with the proposition, is at variance with the sequence of clinical events forming the structure of Professor Winslet's hypothesis and more in line with the upward progression of an infective process beginning in the perianal region. It is agreed between the microbiologists on each side in this case that the infection began on 11 October 2011, thus two days before the entries in the clinical records of 13 October upon which particular reliance is placed in this context.
- No other feature of what might be termed the alleged positive indications in favour of a primary pelvic infection has persuaded me that this hypothesis is correct. However, merely because that hypothesis has been rejected on the balance of probabilities does not of itself mean that the construction of events relied upon by the Claimant is necessarily established on the balance of probabilities. The aetiology might simply be unexplained.
- The other side of that coin, of course, is that the undoubted infection (which developed into necrotising fasciitis) must have started somewhere and the only other obvious location, on the evidence, is in the perianal region. One matter relied upon by Professor Winslet to suggest that this is not so is that the presentation was atypical for the location being perianal or rectal. He said that the presentation of perianal or ischiorectal sepsis is normally very straightforward "such that even a medical student would be able to diagnose the majority of cases because it presents with local pain, tenderness and swelling." If one leaves to one side for a moment the actual presentation confronting Dr Partiban on 13 October, it is to be noted that his first thought was "perianal abscess" (see paragraph 37 above). He was not a colorectal specialist - merely, at that stage, the A & E Registrar.
- What is atypical (and acknowledged by Mr Maskrey to be so) is that C is not recorded as (nor recalls) suffering excruciating pain on any of the three occasions when he was subjected to a digital rectal examination. Equally, there were no obvious external signs of an abscess. Dr Partiban recorded some "mild tenderness" (see paragraph 37) and Dr Uhercik recorded "tenderness" at the lateral border of the prostate (see paragraph 50). Neither recorded anything that indicated severe pain on examination. D1's record for 14 October indicated no such pain.
- The question is whether this undermines sufficiently the aetiology for which C contends to result in the conclusion that the aetiology is not established. Doing my best to piece together the various considerations that arise in this context, I have concluded that it does not. C will forgive me for emphasising that he was very substantially overweight at the time which may have resulted in it being less easy to conduct an effective digital rectal examination. Nonetheless, whilst there is no record of severe or excruciating pain on such an examination by either Dr Partiban or Dr Uhercik, each does record a degree of tenderness on examination. That must have been caused by something. That no tenderness of any sort was recorded by D1 during his examination on 14 October is suggestive of a less than thorough or effective rectal examination than there being no anal or rectal pathology at all given the examinations of Dr Partiban and Dr Uhercik and what was recorded on examination at KCH in the very early hours of the following morning (see paragraphs 78 and 82).
- Professor Sells expressed the view that C's diabetes reduced his immune response system (which Professor Winslet to some extent accepted) which may have slowed the abscess formation or even prevented it, albeit an infected process being present. That might, he suggested, have diminished the prospect of finding any "palpable mass" and any true abscess. He thought that Dr Uhercik was correct when using the expression "evolving ischiorectal abscess".
- I am unable to reject that explanation as a possibility, although it does appear to have a somewhat tenuous physiological basis. The only realistic conclusion, in my view, is that if there had been an abscess (which overall remained the impression of the treating physicians at KCH), it was either remote from where the digital rectal examinations reached or was such that C, who was plainly complaining of some considerable pain on 13 October (see paragraph 34 above), did not feel any more obviously intense pain during the examinations.
- Whatever the explanation, and accepting that the recorded location of the tenderness by Dr Uhercik (on the right side) was not where it might been anticipated given the eventual discovery of the left-sided ischiorectal cavity, there can be little doubt that there was pathology in the perianal region and the substantial cavity exposed by the surgery confirms this. It is, of course, to be noted that the indurated lump recorded by the surgical SHO at KCH was left-sided (see paragraph 82 above).
- The final issue in this connection is the location of a good deal of pus in the rectropubic space, as found during the initial surgery on 15 October, and the lack of any pus in the ischiorectal fossa (see paragraphs 84 - 90 above) although there was some necrotic tissue and the cavity itself was consistent with gas having been present. It is said on behalf of the Defendants that the absence of pus (which is acknowledged to be surprising) negates C's proposed sequence of events and supports that advanced by Professor Winslet. Mr Maskrey was, however, justified in saying that this factor did not appear in Professor Winslet's first report as supporting his hypothesis (see paragraph 112 above). One would have thought that if it was a significant factor, it would have been mentioned. At all events, I must try to address the issue.
- Again, I would have welcomed an informed debate (preferably at the joint discussion stage) between Professor Sells and Professor Winslet about this rather than endeavouring, as I have to do, to piece together various threads of their evidence and the evidence of the radiologists in order to reach a conclusion. This is one of a number of issues that might, with the benefit of hindsight, have been better dealt with by some suitable form of "hot tubbing" of the relevant experts.
- I will endeavour to describe what I perceive to be the differences between them, but despite the proposition put to Professor Sells by Ms Mishcon to which I referred in paragraph 90 above, I do not think it was ultimately in dispute that the infective process could permeate the levator ani, whether in an upward direction or a downward direction. Dr Euinton had at one stage suggested that the infection "tracked down to the ischiorectal fossa, across the levators and then to the perineum" which, though he changed his view on the direction of travel subsequently, does suggest that he thought that the physiological process was possible and, of course, if the process could operate in one direction, the likelihood is that it could operate in the other. As I understood Professor Winslet's evidence, he did accept this broad proposition. He also accepted that when pus becomes the subject of necrotising fasciitis it becomes less viscous and assumes a characteristic "dishwater pus" consistency. Cells are killed in this process and when the cells are killed, fluid can permeate through whatever membrane may be involved. However, his thesis, as eventually expressed during cross-examination, was that if the ischiorectal fossa was the original source of the infection, by the time of the surgery (when the necrotising fasciitis had been active) he would still have expected to see some fluid in the ischiorectal space. He says that no such fluid was evident. He also asserted that there would have been "fluid all over" and that it would not go "preferentially from one place to another place and leave the initial place arid."
- Unfortunately, this view emerged when Professor Sells was not present in court and he had not been asked specifically about Professor Winslet's views when he was cross-examined. Professor Sells' general position was that once the necrotising fasciitis commenced within the ischiorectal fossa, the tissues would begin to be damaged by the process to which Professor Winslet referred (and articulated more fully in the article referred to in paragraph 106 above) and that this would happen very quickly. It would, he said, result in the ischiorectal space becoming full of gas under considerable pressure which would have been enough to promote the upward movement of the pus and fluid such that it permeated the levator ani thus creating, as I understood him, the pocket of pus in the retropubic area and leaving behind some gas and a little fluid in the ischiorectal space.
- Professor Winslet said that there was no evidence of fluid in the ischiorectal fossa at the time of the surgery. However, Professor Halligan and Dr Euinton were asked to say whether they agreed that "no fluid (pus) was seen on the CT scan of 15 October in those areas where one would expect to see fluid if there was an ischiorectal abscess". Their joint reply was that what they saw on the scan was "a 2.5 cm (longest axis) fluid collection against the right obdurator internus that might represent an abscess" and they agreed that "there is scattered fluid elsewhere throughout the lower pelvis but that the volume of free gas greatly exceeds the volume of free fluid." They also agreed that "there is no substantial fluid collection in either ischioanal fossa."
- It appears that they agreed that there was some fluid generally in this region, albeit not much and the largest area was on the right side. This is not inconsistent with what Professor Sells said was his understanding of the position.
- I have endeavoured to set out what appear to have been the differences between Professor Sells and Professor Winslet on this issue, but to the extent that it was discussed at the joint discussion between them, there seems to have been broad agreement. The relevant question and answers were as follows:
- My understanding is that, whatever the original source of the infection, Professor Sells and Professor Winslet are agreed that there was "severe synergistic sepsis" which, if that is so, would explain the lack of pus in the ischiorectal fossa. That might not explain the absence of significant quantities of residual fluid in the space created by the necrotising fasciitis, but it may go some way to doing so and to explaining the presence of some fluid. At all events, there is little doubt that there are aspects of C's presentation and its aetiology that are atypical on the assumption that all the clinical records are accurate in what they record, but notwithstanding Professor Winslet's rather lately expressed reservations about this particular feature, I can see nothing intrinsically illogical with Professor Sells' description of what probably occurred. Whilst Professor Sells had to accept that there were a few aspects of his report that were inaccurate, he is a surgeon of great distinction and experience who articulated his views clearly and with authority, but with an engaging modesty. In my judgment, his synopsis of the likely sequence of events fits more closely with what I perceive to have been the true history of the symptoms experienced by C and with what is reported by the radiologists in the case as being seen (or, more accurately, not seen) on the CT scan even though Professor Sells acknowledged that, in his personal experience, the presentation was very unusual (though not totally unique). I do not consider, therefore, that the discovery of a substantial quantity of pus in the retropubic space and the lack of any in the ischiorectal fossa alters the conclusion that the sequence of events put forward on behalf of C is more likely than not to be the correct one.
- Thus, having reviewed the extensive evidence relating to medical causation, I remain satisfied, on the balance of probabilities, that the original source of C's infection was in the ischiorectal fossa, that it developed into necrotising fasciitis and in consequence, as part of the development of that condition, it tracked upwards into the pelvic cavity. It was that sequence of events that led to the initial and continuing complaints of pain in the rectal and anal region and then the abdominal pain. Given what C said at the Mayday Hospital on 13 October (when his perception of the development of his systems was probably more accurate than it subsequently became), there are clear records that he said that he had been suffering pain in the anal/rectal region for 2 3 days. He said it to the ambulance crew (see paragraph 21), the triage nurse (see paragraph 25), to Dr Partiban (see paragraph 37) and to Dr Uhercik (see paragraph 50). This seems to me to be consistent with the developing infection which the microbiologists agree began on 11 October. I consider that this evidence demonstrates that the anal/rectal pain was the dominant pain that C experienced at this time, though by the middle of 13 October he was beginning to experience also some pain in the back. I should say that I do not consider that because there is a nursing record at 11.15 on that day which speaks only of pain in C's "back and hips" (see paragraph 34) it means that the rectal pain had disappeared. Within one and a half hours of that he had been telling Dr Partiban that he suffered pain in the anus for the last few days (see paragraph 37), something he repeated not long after to Dr Uhercik.
- The only feature of the period referred to in paragraph 150 above that is not wholly consistent with that analysis is the telephone consultation conducted by D1 on 12 October. It contains no record of a complaint of rectal pain and if C had been suffering from it from at least the day before, it is surprising that he did not complain about it. As indicated above (see paragraphs 61 - 69), I have reservations about the accuracy of D1's note-taking, but I think there are one or two possible explanations that fit with this omission. C may not have mentioned the pain because it had not developed to the point that it did by 13 October, that it was not the dominant feature, his general position being that he felt unwell, or that he was embarrassed to mention it (thinking that any complaint of constipation covered it). Equally, he could have mentioned it, but in a way that made no impression on D1, or possibly that the latter did not understand what was said: the telephone is not the easiest medium by which to pick up the nuances of a conversation about presenting symptoms. C's evidence was that he told D1 that he could not "poo or wee". If he used that expression, it is possible that D1 simply missed it.
- Since the criticism of D1 is that he failed to act on a clear complaint of constipation and urinary problems made on the telephone (not that it was wrong to have had a telephone conversation with C per se), it is not possible to suggest that his failure to pick up this aspect of what C said was itself a breach of duty. Nonetheless, whatever the reason for there being no specific reference to a complaint of rectal pain in D1's notes for 12 October, it does not, in my judgment, undermine the construction of events set out in paragraph 149 above.
- Furthermore, in addition to the records made at the Mayday Hospital, there is also a record when he presented at KCH in the very early hours of 15 October, when the abdominal pain was undoubtedly dominating the complaints he made, that the abdominal pain "started yesterday" (see paragraph 77 above). It is not clear whether "yesterday" referred to 14 October or 13 October, but there is no record on 13 October of any complaint about abdominal pain which, on balance, suggests that he was indeed referring to 14 October.
- Mr Maskrey accepted openly in his original Skeleton Argument that C is "not now and was not then a clear and precise historian" - by "then" I infer that he meant at the time of the material events in October 2011. I agree with that assessment. As I have already said, C's current account may have been shaped by his belief that certain things happened in a certain way at the time when, in reality, it is extremely difficult for him to remember precisely because of the very difficult times he experienced in the immediate aftermath of the events of October 2011 and the subsequent few months. Doing the best I can to give meaning to the sequence of complaints recorded in the Mayday Hospital and KCH notes, I think that his reliability as a historian became less as time moved on. This may have been to do with his worsening condition about which there can be no doubt. Although his level of consciousness, assessed by reference to the Glasgow Coma Scale, showed that he remained alert throughout, it is difficult to believe that someone in septic shock, having been rushed to hospital at midnight, will be the best and most reliable historian. I consider that, when looked at as a whole, what he is recorded to have said to the ambulance, nursing and medical staff on 13 October is likely to be the most reliable account of the progression of his symptoms until about 14.30 on 13 October. Equally, in my judgment, the evidence does demonstrate that by the time he got to KCH, the abdominal pain was predominating. Whilst not every piece of the clinical jigsaw fits perfectly into place, all that is, as I have said, consistent with the way an ischiorectal abscess that developed into necrotising fasciitis and then tracked upwards into the pelvis would have manifested itself in terms of the symptoms experienced.
- So far as assessing the issue of breach of duty is concerned, the case against D2 falls to be assessed largely by reference to what can be deduced from the notes to which I have referred against the background of a more general appreciation of where the evidence leads. I will turn to that shortly (see paragraph 156 et seq). The case against D1 is rather more problematical in terms of the factual matrix within which it is to be assessed. Again, I will turn to that shortly, but I will begin with the case against D2 and the circumstances of 13 October.
- As a matter of fact, it is not in dispute that C arrived at Mayday Hospital at about 10.30 and left at 16.30 with no blood tests having been administered and no intravenous antibiotics being commenced. Mr Martin places a great deal of emphasis on the proposition that it was C's own decision to leave the hospital before the blood test had been carried out and thus that he (C) deprived himself of the opportunity of further investigation and treatment. He relies upon the case of Darnley v Croydon Health Services NHS Trust [2017] EWCH Civ 151. I will, of course, deal with the implications of that case in due course, but Mr Maskrey's response to that, in general terms, is that it was incumbent on D2, through its clinical or nursing staff, to ensure he knew what the position about the blood test and its relevance was and/or to contact C by telephone once it had been discovered that he had left to remind him that he needed a blood test.
- However, I need to consider first whether the way C was dealt with before he left was below acceptable standards.
- I have already concluded (see paragraph 27) that the triage nurse requested blood tests at the outset. I have not heard from the nurse, but he/she plainly felt that this was necessary. He/she knew that C had been suffering from pain in the anus for two days, was feeling generally unwell, had a slightly raised temperature and a raised respiratory and pulse rate. He was, of course, an overweight diabetic. On the basis of everything that has been said in the case about diabetics being more susceptible to infection than non-diabetics, it does seem to me to be entirely logical to investigate whether there was evidence of an underlying infection, preferably before the patient was seen and examined by a doctor. At least the examination would be informed by the results of a blood test. The one test that would be a marker for infection is the CRP level (see paragraph 50 above). Although Mr Maskrey submitted that the consensus amongst the experts other than Dr Campbell-Hewson was that the CRP level would have been included in this test, I do not think it is clear on the evidence that it would have been part of the test requested by the triage nurse. Mr Peter Richmond, the Consultant A & E surgeon called for C, only said that the usual blood tests at this stage "sometimes" included the CRP level. Dr Campbell-Hewson, the equivalent expert for D2, did not regard it as usually included in this kind of test. Whilst, as I have said, it seems entirely logical to include it if an infective process is suspected, I cannot on the evidence find that this part of the test would necessarily have been included or that a failure to do so fell below generally accepted standards. D2 has called no evidence which enables me to say whether, in this hospital at that time, it would have been included and Dr Spencer's letter does not give enough detail for me to be able to draw a conclusion on the matter (see paragraph 27 above). I do not consider that the material exists for me to be able to draw an adverse inference against D2 on this issue: cf. Keefe v. The Isle of Man Steam Packet Company Limited [2010] EWCA Civ 683 and Wiszniewski v. Central Manchester [1998] PIQR P324.
- Nonetheless, based upon Mr Richmond's evidence, I do consider that it did fall below an acceptable standard not to have carried out the requested blood test within two hours of C's admission. Whilst I am prepared to take judicial notice of the fact that A & E departments, particularly in densely-populated urban areas, are usually very busy, I have no convincing evidence before me that this was a particularly busy day or busy time and C was, on any view, unwell when he arrived. Had the blood test been carried out and had it included the CRP result, given the agreed evidence of the microbiologists and the intensivists that the CRP (and indeed the white cell count which is also an inflammatory marker) would have been raised on 13 October, this would have been something known to Dr Partiban when he saw C shortly before 13.00. If the CRP was not included, should the fact that it was not included have alerted Dr Partiban to the need for this aspect of the blood to be tested if, as he correctly decided, C should be seen by the surgical team because of a possible perianal abscess?
- The circumstances in which Dr Partiban saw C was set out in paragraph 37 above. C's condition overall had deteriorated in the period he had been waiting and there is evidence that he was in considerable pain. Dr Partiban concluded (perfectly reasonably) that a perianal abscess was a possibility and, equally reasonably, referred him to the surgical team. However, as indicated above, there were no blood results of any kind available at the time and Mr Richmond said that Dr Partiban should have "chased up" the blood tests. I am bound to say that I can see no logical reason for not doing so and, more specifically, asking for the CRP result indeed, quite the converse: all logic pointed in favour of wanting the CRP result. Had this been chased up, there was at least the chance that the result would have been available by the time Dr Uhercik saw C an hour or so later. Dr Spencer was of the view that Dr Partiban had not appreciated how unwell C was and this failure to chase up the appropriate blood test is, in my view, a further reflection of that failing. Had the CRP result not been available to Dr Uhercik, but was known to be "on the way", he would at least have known (as he could have made clear to C) that the important test had been carried out and that the answer would be available soon.
- As it was, Dr Uhercik effectively started afresh some 3½ hours after C was first admitted to the hospital. Nonetheless he did have available the clinical records made thus far. His actions, strictly speaking, fall to be assessed by reference to what someone with appropriate surgical expertise should have done in the situation. On that basis, the views of Professor Sells and Professor Phillips are the most relevant for present purposes, bearing in mind, of course, that Dr Uhercik was not expected to bring to bear the skills and expertise of a specialist colorectal surgeon.
- I have already indicated the differential diagnosis made by Dr Uhercik on the evidence available to him at the time (see paragraph 50). Both Professor Sells and Professor Phillips agreed that this was a reasonable differential diagnosis to make at the time. However, Professor Phillips accepted (as indeed did Dr Uhercik) that Dr Uhercik should have carried out a further set of observations personally to see whether there had been any material change since the last set of observations that had been obtained at 12.40. Naturally, one does not wish to be over-critical of a junior doctor covering many areas in the hospital (as Dr Uhercik was at the time), nor to be over-critical with the wisdom of hindsight, but given the variability in the previous observations of C, it would seem logical to have checked again at this stage. Not to have done so must be seen as falling below an acceptable standard. However, the failure to do this cannot be said on the evidence to be directly causative of any injury to C, but it tends to confirm a general lack of urgency in dealing with someone with potentially worrying signs.
- There is a debate between Professor Sells and Professor Phillips about whether Dr Uhercik should have gone further than simply requesting the blood tests that he did (to which I will return below see paragraph 167), but I will focus on the blood tests for the moment. Dr Uhercik did request the test to include the CRP level which would have assisted in determining whether there was an infective process (see paragraph 50 above). It is not in dispute that he was right to commission this aspect of the test. Given the history (see paragraph 160) and the observation made in paragraph 161 above, logic might have suggested that he should have marked the request "very urgent", but neither Professor Sells nor Professor Phillips suggested that it was unreasonable for him to proceed on the basis of an expectation that he would receive the results within an hour (which is what Dr Uhercik anticipated). Had that expectation been satisfied, the result would have been available shortly after 15.30. As it was, given that C left the hospital about 16.30 and there is nothing in the records to indicate that he was not available for taking the sample when the staff were ready to take it, the only reasonable inference is that the "system" failed to deliver the result within that period (or even to have taken the specimen), a period which arguably should, in any event, have been foreshortened earlier in the chronology of the day.
- As I understood his evidence, Professor Philips accepted that where one part of the differential diagnosis was "an emerging ischiorectal abscess" it was necessary to exclude the possibility that there was such an abscess before C was discharged. He agreed that at the time C was seen by Dr Uhercik it was not possible to rule out the presence of an infective process that had gone beyond a localised abscess. He also accepted that the diagnosis of an abscess was high on the differential diagnosis at this time. Again, as I understood his evidence, he accepted that if the blood test had revealed an increased CRP level (which it would have done), there would have been evidence of an infective process which required investigation and/or treatment. In other words, C would not have been discharged immediately. If prostatitis had been demonstrated, that would not, in his view, have required admission necessarily and the likelihood is that C would have been discharged home.
- I will deal with what ought to have been the next step if this blood test had been received within the period that it ought to have been received in due course (see paragraph 168 et seq below). Dr Uhercik accepted that the outcome of the blood test would have informed his own decision about what to do next which would probably have involved reference to the registrar and, ultimately, to the consultant.
- I have characterised what occurred as a "system failure" rather than something that can fairly be attributed to the breach of duty of some individual or individuals. On the evidence I can do little else: the relevant records for the period under consideration are sparse and it will be apparent that some of the records for earlier in the day are difficult to interpret, certainly in relation to the sequence of events. Standing back from the roles of various individuals, so far as the circumstances of those roles can be ascertained, the general impression one gains is that C had "slipped through the net" by the time he was beginning to question whether he should remain in the hospital or ask his wife to come to collect him. He seems to have been lost to the system at an important time. I will deal with the consequences of his decision to leave below, but if my analysis of the sequence of events is correct then, had the system operated properly, clear evidence of the existence of an infective process should have been available to Dr Uhercik before C decided to leave.
- It was Professor Sells' view (much along the lines of the view expressed by Dr Spencer) that C should have been put on intravenous antibiotics pending the blood test results. However, Mr Richmond, having reflected on the matter, said that he acknowledged that some would have started antibiotics whilst others would have waited until the blood test results were available. On that basis there could be no breach of duty by not introducing intravenous antibiotics in the circumstances that presented themselves to Dr Uhercik, though I would, for my part, add the proviso that that would be acceptable only if the blood test was to be carried out in the timescale contemplated by him. Since Dr Partiban does not appear to have addressed the question of the blood test, it might be said that he was at fault in not starting intravenous antibiotics. However, he did refer C on to the surgical team and there is no real basis for concluding that a breach of duty in not starting intravenous antibiotics had any causative impact. I say nothing more about it.
- If the blood results had been available by shortly after 15.30 (which would have involved C knowing that the sample had at least been taken) then, even if there was some delay in conveying to him the outcome of the test, in all probability (as I so find) C would have remained in the hospital until he had been seen again by Dr Uhercik and/or by the registrar/consultant. It is clear on the evidence that, at a minimum, he would have been admitted and put on intravenous antibiotics given the evidence of an infective process and also on intravenous fluids. Given the result of the test, there should not have been any further delay in active consideration being given to what should be done next.
- The effect of the intravenous antibiotics would simply have slowed the infective process which by then had been continuing for about two days or so and would have stabilised C's condition. If, as I have found, C's primary pathology was an ischiorectal abscess, the first question to be addressed is whether that could and should have been diagnosed and drained surgically on 13 October.
- Given the existence of a differential diagnosis that included an evolving ischiorectal abscess as one possibility, subject to the contrary view of Professor Winslet, there was a consensus amongst the relevant experts that a CT scan was required to establish whether this was or was not so. Professor Sells says in his reports that a CT scan ought to have been considered and he repeated this in his oral evidence. Mr Martin challenged it on the basis of the suggestion that because there were no physical signs of an abscess (no palpable mass and no external signs) there would have been no reason to carry out a CT scan. Professor Sells disagreed that there was no "sign", given the tenderness of which C complained on rectal examination, but emphasised that if there was a high index of suspicion, a CT scan must be carried out because it would be "absolutely discriminatory". The scenario being considered here is that Dr Uhercik had considered that an evolving ischiorectal abscess was a possibility, a suspicion that would have received some support from the raised CRP that would have emerged from the blood test. Against that background, the case advanced on C's behalf is that the next obvious step was an urgent CT scan.
- I did not understand Professor Philips to challenge this view in principle. It was, as I have indicated, Professor Winslet who raised objections to the suggestion of a CT scan at that stage. A raised CRP and a raised white cell count would have indicated, he accepted, the presence of an underlying sepsis, but what would have happened in, as I understood him, his specialist colorectal unit, would be to admit the patient for assessment whilst giving fluids and antibiotics and no immediate CT scan would be undertaken. He also suggested that in a district general hospital or even a teaching hospital the earliest time at which a CT scan would have been mandated in this case would have been on the morning of 14 October after further clinical assessment and another set of blood results. Even then he suggested that it might take up to 24 hours for such a scan to be obtained in an NHS hospital, though he did ultimately accept that it might have been done late on 14 October.
- I regret to say that I cannot accept that this represents a logical position to adopt in relation to the circumstances of this case given what would have been the position at or about 15.30 on 13 October if the blood test had been carried out. The registrar or consultant (and it would doubtless have been one or other at this stage) would soon thereafter have been presented with an obese diabetic who had been complaining of anal/rectal pain for 2/3 days, whose observations were variable (at one stage earlier that day he was classified as "unstable" within the internal hospital guidelines), whose blood results indicated an underlying sepsis and in respect of whom a credible differential diagnosis of an evolving ischiorectal abscess was made. There is no evidence of any risk involved in carrying out a CT scan, but there is evidence of a risk of the further development of the infective process, even with the administration of intravenous antibiotics, if something was not done. If it is the case (as it is) that the clinical presentation was unusual, there is, in my judgment, all the more reason, as Professor Sells said, to isolate the location of the underlying lesion. This was supported by the intensivists, Drs Power and Bell. Mr Maskrey made the point, which has some force, that a CT scan would have shown if the problem was merely prostatitis: if it was, C could have been discharged home, thus sparing the hospital the need to admit him.
- Professor Winslet was not, of course, called as witness on matters of breach of duty and his observations could arguably be treated as irrelevant on that basis. However, given his undoubted distinction, I would be reluctant to treat his evidence in that way. Nevertheless, I do consider, for the reasons I have given, that it is not a sustainable and logical position to take in relation to the circumstances in the late afternoon of 13 October as they should have been and I consider the countervailing expert views to be more persuasive. It may be that he has been substantially influenced by his own perception of the underlying condition and what his view of C's presentation was at that time. At all events, Professor Winslet's position might have been strengthened if D2 had called either the registrar or the consultant to say that if he/she had been confronted with this position, a CT scan would not have been mandated with good, sustainable reasons for not performing one. However, no such evidence was forthcoming and I have received no evidence to suggest that either the registrar or the consultant might not have been available to give evidence.
- My conclusion, therefore, is that it would not only have been in accordance with the requirement to provide C with reasonable care to commission an urgent CT scan on 13 October, but that a scan would, more probably than not, have been commissioned within an hour or so of it being requested. When something is urgent, it should be dealt with urgently. This is, of course, on the factual basis that C had remained in the hospital after having been seen by Dr Uhercik. I will deal with the alternative scenario namely, of C having left the hospital, below (see paragraph 182 et seq).
- What would the CT scan have revealed? I do not believe the radiologists were asked to address this specific scenario, but Professor Sells said that it would have revealed inflammation in the left ischio-rectal fossa. In his first report he had said that a CT scan on 12 October would have revealed "an inflammatory swelling of the left ischio-rectal fossa" and such a scan on 13 October would have "shown a mass to the left of the rectum and surrounding oedema." In the joint statement with Professor Winslet, when addressing the question of what a CT scan on 14 October would have shown, he said that it would have shown "a large inflammatory mass in the left ischiorectal fossa and extension of inflammatory tissue upwards."
- These observations are, of course, made in the context of his view that the source of the infection was indeed the left ischio-rectal fossa (which had started on 11 October), a proposition which, on the balance of probabilities, I have accepted (see paragraph 149). To that extent, it is logical to assume that there would be indications of such an infection on the CT scan and I find that this would indeed have been so.
- Allowing some time for the CT scan to be obtained and reported on, even if only orally, the position is that the surgical team should have been in possession of the result by, say, 17.30 to 18.00. What would have happened next? Professor Sells is undoubtedly of the view that urgent surgery would have been required in this situation and I accept that: there would plainly have been a risk of the sepsis progressing quickly, as indeed did occur later the following day. It is very difficult to know whether C could realistically have been prepared for surgery on the evening of 13 October. There is no evidence about whether he had eaten during the day, what his blood sugar level was, what the state of his blood pressure was and so on. When he was admitted to KCH in the early hours of 15 October and the decision to operate was taken, he had to be stabilised before he went to theatre (see paragraph 84 above).
- On balance, I think that, on the assumed scenario of the CT scan result being available at or around 17.30 to 18.00 on 13 October, the likelihood is that his surgery would be delayed overnight whilst steps were taken to have him ready for theatre first thing the following morning. In the meantime, he should have been monitored closely in case of any obvious deterioration with the possibility of emergency surgery being kept in mind. Since the preponderance of the evidence (see paragraphs 191 - 199 below) is that operative intervention early on 14 October would have secured a good outcome, it follows that whether it might have been carried out earlier is not really material. It is, of course, possible that the view would have been taken that surgery was necessary late on 13 October (though C would have to have been made ready for surgery before the surgery took place), but I do not consider, on the scenario I have described, that it would have been negligent to delay the surgery until the following morning provided that C was monitored closely throughout the night.
- My essential conclusion, therefore, is that it was negligent for D2 not to have arranged for C to be in theatre for surgery to deal with a suspected ischiorectal abscess by first thing in the morning of 14 October. This has to be based on the factual scenario (that ought to have happened if D2's system had operated correctly) that C would have been aware that Dr Uhercik had asked for a blood test and that a sample had been taken shortly afterwards such that the result was available by shortly after 15.30.
- Standing back from the individual periods of time that go to make up the period from 10.30 to 17.30-18.00, it does not seem to me to represent an unreasonable demand that C should have emerged with a reasonably clear way forward within 7-7½ hours.
- Of course, he did not do so because he left the hospital at about 16.30. It is necessary to consider whether that should have been allowed to happen when there was an important test outstanding and, in any event, whether something should have been done thereafter to suggest that he returned to the hospital.
- Leaving aside the issue of precisely when the blood test commissioned by Dr Uhercik should have been done, the fact that it was not done before C left the hospital should plainly have been noted in the hospital records. By "noted", I mean (i) that his absence when called for taking the specimen was noticed and (ii) that it was noted in the clinical records. Mr Richmond said that this should have been done and I do not think it was seriously disputed by Dr Campbell-Hewson. There is no note about this and it leads to the inference that either C was never called to provide a specimen for the test because the request for the blood sample went unheeded (as had the request made by the triage nurse earlier in the day) or that he was called, but his absence was not recorded in the notes. Each of these alternatives would represent a "system failure".
- Had this aspect of the system not failed, what, if anything, should have been done by the hospital when it noted that C was not present to give the blood sample? Again, it needs to be borne in mind that he was an overweight diabetic who might have an ischiorectal abscess and who was awaiting a blood test that included the CRP level. Whilst I do not underestimate at all the pressures that the clinical, nursing and general staff face in a busy A & E Department, I cannot accept that a telephone call to one or other (or, if necessary, each) of the numbers on the records could and should not have been made in this case. The purpose would be to convey to C the message that the hospital had been expecting to see him to give a blood sample and inviting him to return to provide one. This matter was the subject of evidence by Mr Richmond and Dr Campbell-Hewson. The former took the view that, in the particular circumstances of this case, largely for the reasons I have already indicated, a telephone call would have been what he would have expected and would have reflected the practice in his own department. Dr Campbell-Hewson was of the view that telephoning "absconders" simply does not happen and the most that will occur is that a letter is written to the patient's GP indicating what happened. (There is, incidentally, no evidence that this was ever done.) I will return to this below, but it is, perhaps, instructive to note what was alleged in the Amended Particulars of Claim in this regard. The matter was put somewhat compendiously in the following terms:
- Notwithstanding that allegation, no statement from anyone (including Dr Spencer) was forthcoming dealing with how the situation of a patient who was waiting for further tests, but who leaves before they are carried out, was dealt with within the Mayday Hospital at the time. Mrs Ashley said that if anyone would pursue by telephone someone who had left the A&E department before a test had been carried out, that would be done by the clinical staff, not the receptionist. That may be so, but that does not suggest that pursuing such a patient by telephone was never done and the responsibility for deciding whether to contact someone would plainly be a matter for the clinicians. In this case there is no note or record of consideration being given to the issue by any clinician.
- Mr Richmond said that the purpose of having the telephone numbers of the patient and/or members of his family within the emergency department is that so the patient may be contacted if necessary. That is, of course, an obvious statement, but there seems to be a reluctance on D2's behalf to acknowledge that pursuing a patient who has left before a test has been carried out is something that even ought to be considered. In his written closing submissions (which he adopted orally) Mr Martin, having made the forensic point that the issue of a telephone call did not appear in the earlier pleaded version on the Claimant's case or in Mr Richmond's first report said this:
- This, as it seems to me, is endeavouring to extend the effect of the decision in Darnley beyond what was intended. It does seem to me that the situation in this case is not one that can be swept aside by the assertion that this was all the responsibility of C and that telephoning him would have the effect of imposing an excessive obligation on a busy A & E Department. I accept that his decision to leave the hospital might mean that C cannot rely upon what was said by the receptionist as an actionable misstatement (following Darnley), but this situation is different: it involves the "system" failing (i) to identify the fact that an important test had not been done on C and (ii) to alert him to or to reinforce the desirability of making himself available for it to be carried out. At the risk of repetition, it should be emphasised that he was an overweight diabetic who it was thought might have an ischiorectal abscess. Even if he was told by Dr Uhercik that a blood test was required (which is likely), there is no evidence (because neither C nor Dr Uhercik remember the examination and any conversation) that C appreciated fully the importance of the test. Since he had been waiting since 10.30 in the morning, possibly anticipating a blood test in the light of the triage nurse's request, he may well not have seen this further request for a blood test as any advance in trying to find out what was wrong with him. But whether something said by the receptionist encouraged him to think that there was no point in staying any longer (see paragraph 57), in my judgment, there was a duty on the hospital to check that there was a good reason for him not being there to provide the specimen and then to warn him of the risk of not having done so. Only then could it truly be said that he had made an informed decision about ceasing to place reliance on the hospital that day for finding out what was wrong with him. If that had happened, the decision in Darnley may have prevented him from pursuing a claim.
- As I have said, I am unable to accept that imposing a duty to make contact in a case such as this places an unreasonable burden on a hospital. That people do leave A & E Departments before they are treated is a well-known phenomenon: see, e.g. the review article in the Emergency Medicine Journal, 2011, entitled 'Patients who leave emergency departments without being seen: literature review and English Data analysis' and 'The patient who absconds' 2013, guidance given by The College of Emergency Medicine. Mr Richmond has said that those who come within the cohort of cases to which C would belong for this purpose represent a very small proportion of those who leave an A & E Department before treatment: Mr Richmond is (or at least had been for a number of years) in charge of a busy A & E Department in Poole and had extensive experience in A & E Departments in Wales prior to that. I do not suggest that Dr Campbell-Hewson does not have relevant and appropriate experience, but it is less than that of Mr Richmond, and more importantly his view does not seem to me to address the question of what to do about someone who, like C, has been in the system for the best part of a day, in respect of whom an important diagnostic test has been commissioned and who, for some reason, has left before the test is carried out when there is no record in the notes that he had "gone missing" at the material time.
- All this arises, of course, only if it is established that the hospital realised that C was not present when the sample was to be requested. There is no evidence that this was the case and, as I have said, it is a legitimate inference that no step was ever taken to obtain a sample.
- However, assuming that such a step was taken and C's absence was noted, for the reasons I have given, I do regard it as falling below reasonable standards for no attempt to contact him by telephone to have been made. There is no evidence available to suggest that such a call would not have been successful. Equally, given that C was still feeling very unwell, there is no reason to suppose that he would not have complied with a suggestion that he should return to the hospital. He has said that he would have obeyed the doctors. Since he had been seeking help from the hospital throughout the day (against the background of having sought the help of his GP the day before), I consider that he would, more probably than not, have returned to the hospital to provide the blood specimen. It may have taken a little while to do so because of the family commitments, but I think it likely that he would have returned that evening.
- If that is correct, the sequence of events leading up to commissioning the CT scan would have started and the same scenario as that set out in paragraph 168 et seq above would have arisen albeit somewhat later in the evening. The net effect is that he would have been set for surgery early the following morning with his situation being monitored overnight.
- As the evidence from the experts emerged at the trial, it became the consensus that C did not go into septic shock until quite late in the evening of 14 October, probably around the time of the ambulance being called or arriving where C was staying. The development of the sepsis was recognised to be a gradual, albeit synergistic, process, but there was no one obviously identifiable moment when C was not in septic shock and then was. Nonetheless, during the earlier part of the day the sepsis that had been developing continued to develop. However, what this means is that any surgery undertaken in the morning of 14 October would not have taken place in the context of a patient in septic shock. What was actually revealed when the surgery took place 24 hours later may well have still been in the process of developing, but it can safely be assumed that competently performed surgery would have identified and dealt with anything that may have required attention.
- In their joint statement prior to the trial, Dr Gray and Professor Cartwright were of the view if C had gone to surgery during the morning of 14 October and the matters that were found 24 hours later had been addressed to the extent that they had progressed at that stage, C would have made what they each described as "essentially a good recovery". I will return to deal with what that means below (see paragraph 194). Professor Cartwright took this position though he disagreed with the proposition that the original source of the infection was an ischiorectal abscess. Dr Power was of the view that surgery on 13 October would have led to a successful outcome. In relation to 14 October he said this:
- Dr Bell, however, was of the view that by 14 October "given the inevitability of established infection within the pelvis on this date, the outcome would be broadly similar regardless of primary source."
- Professor Sells confirmed in his evidence that his view was that had surgery been performed up to around lunchtime on 14 October, none of the digital amputations or the leg amputation would have been necessary, although the laparotomies would probably not have been avoided. His view was that provided there was intervention before septic shock occurred, that would have been the outcome. Indeed, as I understood his evidence, surgery somewhat later than midday on 14 October (early afternoon) would, more probably than not, have avoided any amputations. He remained of the view that by about lunchtime on 14 October the need for further abdominal procedures would not have been avoided because of the sepsis that had taken place by then which is likely to have increased pressure in the abdomen.
- This approach is predicated on what I described as the consensus that septic shock did not set in until late on the evening on 14 October. There was evidence that C had maintained his blood pressure up to that time which is not what is expected if septic shock had occurred. It is also the case that disseminated intravascular coagulation ('DIC'), which causes blood clots in the small blood vessels, had not fully set in by that time.
- The contrary view of Professor Winslet was, in effect, that the "die was cast" as long ago as 13 October and, in any event, by 14 October. The laparotomy would, in his view, have sparked off what is often called the "septic shower" which would have led to the same outcome as in fact occurred. Professor Sells response was that, whilst this reaction was a possibility, the earlier the surgical intervention the greater the likelihood of the surgical team being able to address the issue. Dr Power's evidence was to similar effect.
- These competing views are, of course, impossible to reconcile. However, the scenario I am addressing is the bringing of C to surgery in the morning of 14 October when, as is now known, C was not then near to moving into septic shock, but whose risk of doing so would, on competent analysis, have been identified. As Professor Sells said, the surgical team would have been alert to the risk and would have been ready to deal with it. Against that background, I consider it unduly pessimistic to say that the die was already cast and that the amputations could not have been avoided. Obviously, as with a number of issues in this case, it is possible that the pessimistic analysis is correct, but I must deal with it on the basis of what I perceive to have been the probable outcome. I consider it more probable than not that surgery carried out in the morning of 14 October would have been successful and would have avoided any of the amputations.
- It follows that I find liability established against D2 on the basis that had C received proper care and attention at the Mayday Hospital on 13 October, he would not have suffered the amputations that were necessary following his surgery. He may have faced other consequences, but those permanently disabling consequences would have been avoided.
- That conclusion, strictly speaking, renders it unnecessary to consider the claim against D1 in relation to the consultation on 14 October: had D2 discharged its duty of care, C would not have presented to D1's surgery that day. However, should I be wrong about D2's liability, I should consider that claim against D1. I need also, of course, to consider the case against D1 in relation to the events of 12 October because, without going back over the ground covered in relation to 13 October, the prospects of entirely successful surgery would have been even greater had he been admitted and treated correctly on 12 October.
- I have focused on 13 October because, in my view, the factual scenario is easier to resolve for that day than either of the others for the reasons which will be apparent.
- The essential accounts of what took place on 12 October are set out at paragraphs 12 - 16 above.
- I can take the issue in relation to 12 October shortly. It is agreed between the GP experts that if C told D1 that, in addition to the symptoms recorded by D1, he had constipation and was having difficulty passing urine that it would have been negligent for D1 not to have arranged a face-to-face consultation at which further questioning would have been carried out and a digital rectal examination probably carried out.
- Did C mention these matters? I am sure he now believes he did, but for the reasons given in paragraphs 151 - 152 above I do not think that I can be satisfied on the balance of probabilities that he did or, at least, did so in a way that made an impression on D1. As I have said, I do not consider that D1's note-taking generally was of the requisite standard, but I doubt that he would have missed either complaint if it had been made or made in a way that made an impression on him. However, there is a further, more significant, factor: I have already indicated that the records at the Mayday Hospital on 13 October are probably the most reliable source of evidence of C's complaints and they do fit in largely with the most likely physiological explanation for the condition he was found to be in when seen at KCH. There is no record in those records of a complaint of constipation or urinary difficulty. He did say that day that he had suffered from rectal pain for 2-3 days, but (perhaps surprisingly) he has not said that he said that to D1 on 12 October. The first complaint of urinary difficulty, according to the records at the Mayday Hospital, was that the difficulty started "last night", in other words, after he had seen D1. So far as any complaint of constipation is concerned, (a) none was made at the Mayday Hospital and (b) the first recorded complaint was in fact made by D1 when he saw C on 14 October (see paragraph 62). Although there were records at KCH suggesting that he had urinary problems and constipation for several days, I have indicated why I do not think I can place much reliance on C's recorded history at that time (see paragraph 154).
- Given that I do not find that C complained of either constipation or urinary difficulties or did so in a way that made an impression on D1, I do not consider that D1 was negligent on 12 October (see paragraph 202 above). Prescribing antibiotics over the telephone may not have represented good practice, but that is not the issue in this case.
- Turning to 14 October, I have already alluded to some unsatisfactory features of D1's record keeping and that undoubtedly applies to the note he made of the consultation on 14 October. I have already indicated what I am prepared to accept that he did and what I am not prepared to accept that he did. I have accepted that he did perform a rectal examination and indeed that would be consistent with the complaint of constipation that C is recorded as having made. It is surprising that D1 elicited no tenderness during that examination because two doctors at the Mayday Hospital the day before had each elicited a degree of tenderness on rectal examination. That does call into question the adequacy of the examination, but that is not, in my judgment the central part of the issue.
- The question is whether C's overall presentation required D1 to arrange for his admission to hospital. One fact that needs to be considered is that, as indicated previously (see paragraph 191), it became common ground that, whilst C would have been suffering a developing sepsis during 14 October, he did not go into septic shock until late that evening. Indeed, despite what must have been a very advanced stage in the development of sepsis, he could walk down the stairs to meet the ambulance crew before being taken to KCH (see paragraph 73 above). Against that background, it is not such a persuasive case against D1 that he should have realised how ill C was: his presentation may not have been of an obviously unwell man even though he was complaining of feeling unwell and being in pain.
- The other factor of some significance, in my judgment, is that C was complaining of lower abdominal pain according to D1's note. He was not complaining of rectal pain. It does have to be said that the KCH's notes suggest that by the evening of 14 October it was abdominal pain that was the dominant feature of the presentation and that, of course, is consistent with the aetiology of the condition that is contended for on C's behalf and which I have found to be the most likely aetiology.
- It was accepted by the GP experts that if D1's note, as it stands, represented what C was complaining about and reflected the examination he conducted, there was no basis for referring C urgently to hospital. If there had been a report of rectal pain, it would have required urgent referral to hospital.
- I have not found the resolution of the factual issues surrounding this examination entirely easy, but overall I consider that C probably did not complain of rectal pain at that consultation. As I have said, the site of pain was moving from the rectal region to the abdominal region that day, in accordance with the aetiology to which I have referred, and that may well constitute the explanation. But I am unable to find on the evidence that he did indeed complain of rectal pain. Equally, whilst he says now that he mentioned to D1 that he had been to the Mayday hospital the day before, I find it impossible to believe that D1 would have failed to record that if it had been said. Indeed, it might have alerted him to the possibility of something more serious underlying C's complaints. Quite why C did not mention it is unclear, but he may have thought it would not be very persuasive to tell D1 that he had been to the hospital and had left because it looked as if the hospital thought there was nothing wrong with him.
- Whilst there are, as I have indicated some considerable reservations about D1's notes and the examination he conducted on 14 October, I do not think it has been established that he should have referred C to hospital that day and, accordingly, the case in negligence against him is not made out.
- It follows that liability and causation to the extent indicated in paragraphs 198 above are established against D2.
- Liability is not established against D1.
- The resolution of the factual and medical issues in this case has been as difficult an exercise as I can recall in quite a few years of dealing with cases of this nature. The experienced experts contended for two different aetiologies with equal conviction that their view, at least from the clinical perspective, was correct and the factual issues were rendered far less easy to resolve than in some cases because of the poor quality of some of the note-taking and C's difficulty (quite understandably) in remembering the sequence of events clearly.
- Whether I have reached the "right" conclusion will doubtless be a matter of debate between those involved in the case. However, one advantage of the judicial viewpoint is that it is possible to take an overall view of all aspects of the evidence, expert and otherwise, and reach a decision where most issues are resolved on the basis of what is more probable than not. That is what I have endeavoured to do and I should like to express my appreciation to Mr Maskrey and Mr Pratt, Ms Mishcon and Mr Martin, together with their teams, including the experts, for their assistance in helping with that process.
- I should also say that it would have been very much less easy to review the evidence (which has been necessary in order to prepare this judgment) without the daily transcripts that were obtained. I am grateful to those parties who agreed to meet the expense of this and, of course, to the transcribers for their efforts. I am sure significant time was saved during the trial by having this facility.
Mr Justice Foskett :
Introduction
Background in more detail
"I attended your hospital by ambulance as I had abdominal pain, "flu" like symptoms, was feverish and was unable to pass urine or open my bowels. I was already suffering with an abscess on my lower spine.
I was seen by a junior doctor who informed me that there was nothing wrong with me. No blood or urine tests were undertaken. I was adamant that I was feeling incredibly sick and the doctor said that if I wished I could go and sit in the A&E department for a second opinion.
I was barely able to wait in the A&E department as in addition to the symptoms explained above, I was also suffering from an abscess on my lower spine and after 6 hours of being in the A&E department, I called my wife to take me home."
"As part of our investigation into the concerns you raised following your visit to A & E on 13 October 2011, we have reviewed your medical notes and discussed your care with Dr Oliver Spencer, Consultant in Emergency Medicine who contributed information to our response.
You were concerned that no blood samples were taken and your symptoms were not sufficiently investigated by the doctor in A & E. Dr Spencer confirms that the decision to refer you to the on-call surgical team was the correct decision given your symptoms. However, on reviewing A & E notes and in particular your observations, he explained that your temperature, respiratory rate and heart rate were all raised. Dr Spencer advised that all these findings suggested a possible serious infection and you should have been admitted to hospital for further investigation and received intravenous fluids and antibiotics.
On reviewing your medical notes, it appears that the doctor who reviewed you did not appreciate how unwell you were at the time of attendance to A & E. I am deeply sorry for this error and was particularly disappointed to read that you were admitted to King's College Hospital the next day.
As a result of your complaint, Dr Spencer has been asked to ensure all junior doctors receive enhanced training to ensure they are mindful of the criteria and signs of serious infection, and confident in the early and robust management of infection particularly with regard to the timely administration of fluids and antibiotics."
"You are right when you say that no blood samples were taken and your symptoms were not sufficiently investigated by the doctor in the accident and emergency department. The decision to refer you to the on-call surgical team was the correct decision given your symptoms however reviewing the Emergency Department notes and in particular your observations: your temperature, respiratory rate and heart rate were all raised. All these findings should have suggested a possible serious infection. In this situation you should have been admitted to the hospital for further investigation and to have been given intravenous fluids and intravenous antibiotics."
"The decision to refer to the on-call surgical team was the correct decision given this man's presentation. However, reviewing the Emergency Department notes and in particular the observations: This gentleman's temperature was raised, his heart rate was persistently raised and respiratory rate was raised. All these findings are consistent with infection and possible sepsis. A urinalysis was performed. I was unable to find any blood results pertaining to this attendance in the Emergency Department. There is no documentation of any intravenous fluids or intravenous antibiotics being administered. Reviewing the medical notes I do not believe that the doctor who reviewed him has appreciated how unwell he was at the time when he was seen in the Emergency Department. Blood tests including lactate should have been carried out, and he should have received intravenous fluid resuscitation and intravenous antibiotics whilst waiting for the surgeons to review him."
" The aorta is of normal calibre and there is no evidence of abdominal aortic aneurysm. Free gas is seen within the pelvis that appears to be localised within the perineum. There is gas surrounding the rectum and tracking up along the side of the pelvic walls. There is fatty stranding and inflammatory change seen in the pelvis. No discrete collection is identified. No significant free fluid seen in the abdomen or pelvis. There is no evidence of intestinal obstruction. No convincing sign of intestinal perforation. The rectum and sigmoid colon are largely collapsed but does appear to be slightly thick walled. Diverticuli (sic) are present in their (sic) rectum and sigmoid colon. The caecum and descending colon appear thick walled. The appendix has a normal appearance. A few small 9mm non-specific nodes are seen within the right iliac fossa ."
"Conclusion: The origin of the free gas in the perineal region and gas tracking in the anterior abdominal wall in the pelvis is uncertain, but there is no convincing bowel perforation. Given the distribution of free gas, perineal infection (? Soft tissue abscess/necrotising fasciitis) must be considered. Images reviewed with surgical team."
"He was sent from the Emergency Department at KCH to the CT scanner, which demonstrated free gas within the pelvis that appeared to be localised within the perineum. There was gas surrounding the rectum and tracking along the side of the pelvic walls with some fatty surrounding and inflammatory change also seen within the pelvis. No discrete collection was identified and there was no significant free fluid in the abdomen or pelvis and there was no evidence of intestinal obstruction or perforation. Given the distribution of the free gas, [perianal] infection secondary to soft tissue abscess or necrotising fasciitis was considered. [C] went almost immediately to theatre where he underwent incision and drainage of his left tissue rectal cavity with evacuation of a [retropubic] collection of pus. There was a laparostomy and significant debridement of his perianal region and around the bladder. De-functioning colostomy was performed and his abdomen was left open with a Vac dressing to the wound."
"No connection between [the] retropubic and perineal/perianal region."
The expert dimension concerning the aetiology
The anatomy and relevant medical terminology
"The term necrotizing fasciitis (NF) describes a group of relatively uncommon, but life-threatening infections of the skin, soft tissues, and muscles, which tend to progress rapidly through the fascia planes, causing gradual destruction of the fascia at a rate reaching 2-3 cm/h. Developing in the lower or upper extremities, the perineum and genital area (Fournier's gangrene) and in the abdominal wall, its swift clinical course is correlated with polymicrobial infection and synergy, which usually co-exists . The majority of cases present anaerobic bacteria that proliferate in a hypoxic environment and produce gas, which accumulates in the soft tissue spaces, giving the characteristic image of gas gangrene on plain X-rays and computed tomography (CT) scans .
Early diagnosis of NF is mandatory. Any delay could prove fatal, given its association with more extensive surgery, higher rates of amputation, and higher mortality rates. Furthermore, if left untreated, the infection could lead to systemic inflammatory response syndrome (SIRS)."
The development of Professor Winslet's opinion
"[D1's] case on causation is that [C] did not have a perianal/ischiorectal abscess but was suffering from primary pelvic sepsis (probably caused by a perforated diverticulum). This was a progressive synergistic infection which inevitably required surgery."
"7.1.2 At the time of presentation at A&E on 13.10.2011 [C] was generally unwell with no localising symptoms to the anus, perianal or ischiorectal region. He had back pain, hip pan and urinary symptoms and rectal examination revealed mild tenderness only rather than exquisite tenderness one develops with perianal sepsis. The indications for CT are abdominal pain radiating to his back in the presence of suprapubic RIF and LIF tenderness. The CT on 15.10.2011 demonstrated perirectal sepsis and diverticula within the rectum and sigmoid. At the EUA[1] there was no pus in the perineum but necrotic material and laparotomy revealed retro pubic sepsis.
7.1.3 Perineal sepsis tracking proximally produces local symptoms of pain in the perineum. It does not present with general unwellness back pain hip pain and urinary symptoms. It does not associate with the presence of suprapubic RIF and LIF tenderness. In light of these presentation and clinical findings as well as the CT which showed perirectal gas no discrete collection and diverticula in the rectum and sigmoid I believe [C] developed initial occult pelvic rather than perineal or ischiorectal sepsis which would explain the lack of cutaneous manifestations of sepsis, the lack of exquisite pain on rectal examination the radiological and operative findings. The reason I believe that the infection is likely to be pelvic in origin, spreading towards the perineum, is that the patient's symptomatology in A&E on 13th October, pain in the anus, abdomen, hips and back, is not compatible with perianal sepsis. [C] also has difficulty passing urine which dates back to 12th October. I would refer to the [C's] witness statement.
7.1.4 On the balance of probability, [C] would not have avoided necrotising fasciitis. However, for the reasons given above I do not believe [C] had an ischiorectal/perineal abscess.
7.1.5 If a court accepts this view it would have a major effect on causation as a sepsis would have been occult until it was well established."
(i) in relation to the scan of 15 October 2011, there was (a) minimal evidence of sigmoid diverticulosis, (b) no evidence of sigmoid diverticulitis, (c) no evidence of free intraperitoneal gas, (d) evidence of extra-peritoneal gas in the soft tissues of the pelvis and the majority of the gas seen on the scan appears to have been extra-peritoneal and (e) the imaging features, on the balance of probabilities, were more suggestive of necrotising fasciitis than of a bowel perforation;
(ii) in relation to all of these CT images (two subsequent CT scans being available for inspection), there was no evidence of a perforated sigmoid diverticulum.
"3.1.2 A history of anal pain was given to the surgical SHO. At rectal examination there was tenderness at the lateral border of the prostate between 10 and 11 o'clock with no other palpable masses. A possible evolving ischiorectal abscess or prostatitis was considered.
3.1.3 The importance of this entry is that it confirms a history of anal pain but the clinical findings are not compatible with an ischiorectal abscess where the tenderness would be lateral, i.e. between 2 and 6 on a clock face if it was on the left hand side, and 6 and 10 on the clock face if it was on the right hand side. The tenderness between 10 and 11 would be in the region of the prostate which runs from 10 til 2 and would be compatible with the sepsis identified in the retropubic space at the time of subsequent laparotomy.
3.1.4 Furthermore, the tenderness elicited from an ischiorectal abscess would be in the anal canal rather than the level of the prostate gland which is above the levator ani muscle indicating that the sepsis was supra levator. This finding in the absence of any external manifestations of sepsis in the buttock (the note clearly states 'externally NIL') would indicate that the sepsis began proximally and extended distally."
"3.15.1 It is accepted that on presentation to the emergency department on 13 October [C] complained of 'pain in anus for last two days', but he was also complaining 'back and hips painful' such that he was 'unable to get off trolley'.
3.15.2 Such pain as reported and documented is compatible with referred pain from nerve root irritation or compression more proximally within the lumbosacral plexus from the spreading pelvic infection rather than focal pathology at the precise site of the reported pain."
"The history of anal pain in the context of these findings has been explained within my previous report as being attributable to referred pain from an infective/inflammatory process higher within the pelvis generating irritation of nerve roots ."
"Is it agreed that the Claimant's reported pain in the rectum/anus could be attributed to referred pain from an infective/inflammatory process higher within the pelvis generating irritation of nerve roots or proctalgia fugax?
KP & DB Agree: There are multiple potential causes of perianal/rectal pain and this suggestion is a reasonable possibility."
"If this was a perianal/ischiorectal abscess, would you expect pus to have been seen in the ischio-rectal fossa on (a) the CT scan performed on 15 October and (b) at operation on 15 October?
RS: No. Necrotising fasciitis would create the big necrotic cavity, which would replace the pyogenic membrane.
MW: Will say in an uncomplicated perianal or ischiorectal abscess, he would expect to see pus on CT and at operation. In the presence of severe synergistic sepsis, pus would not be commonplace. Therefore, the Experts agree."
Breach of duty - the case against D2
What should have happened if the blood results had been obtained?
What did happen and what should have happened concerning C's departure from the Mayday Hospital?
"There was a failure on the part of the A&E staff and/or the surgical team to ensure that the Claimant was contacted following his departure from the second Defendant hospital that night or the following day. The surgical team appear to have been formally in charge and when they realised that the Claimant was missing should have attempted to telephone the Claimant to summon him back to hospital. If the surgical and/or A&E team were unable to contact the Claimant they should have handed over the responsibility of both locating and retrieving the Claimant to the senior nursing officer. The senior nursing officer would then have had to implement the second Defendant's policy for contacting patients urgently."
"If it was mandatory to summon C back to hospital (a patient who had capacity and absconded whilst waiting for blood tests with a reasonable differential diagnosis of ? evolving ischiorectal abscess/?prostatitis) then this obligation would seem to apply to all adult patients who leave without being seen who need blood tests or might have an infection. There is nothing in the material provided by the experts which could justify the imposition of so wide an obligation on a busy A&E department.
In reality this is just another mechanism by which C has sought to fix D2 with responsibility (i.e. to blame D2) for the consequences of his own decision to leave. The submissions on this topic above apply with equal force: C must take responsibility for his own action in leaving."
The effect of surgery on the morning of 14 October
"On balance, I believe [C] would have developed severe sepsis potentially bordering on septic shock and required a period of organ support in the critical care unit. However, earlier surgery on 14th would have occurred ahead of the marked activation of the coagulation cascades and on that basis I believe that limb ischemia and tissue loss would have been substantially reduced if not avoided altogether."
The case against D1
Conclusion on liability
Concluding observations
APPENDIX 1
Consultant Surgeons (breach of duty)
C: Professor Robert Sells
Professor Sells is a retired consultant in general surgery and transplantation. He was based in the Royal Liverpool University Hospital between 1971 and 2005 when he retired.
D: Professor Robin Phillips
Professor Phillips has been a Consultant Surgeon at St Mark's Hospital for Intestinal Diseases, London, for many years and has had other roles at St Mark's and elsewhere. His speciality is colorectal surgery.
Consultant Surgeons (causation)
C: Professor Sells
(see above)
D: Professor Marc Winslet
Professor Winslet was first appointed as Professor of Surgery and an Honorary Consultant Surgeon at the Royal Free Hospital in 1996 and he has remained largely associated with the Royal Free since then, as well as UCL. His main interests include colorectal surgery.
GPs
C: Dr Laurence Knott
Dr Knott retired as a GP in 2012 after over 30 years in general practice in Enfield. He is currently a senior assessor for the General Medical Council and is a Clinical Complaints Adviser for the Medical Defence Union.
D: Dr Jeremy Budd
Dr Budd retired as a full time general practitioner in 2015 after 30 years as a GP. Since 2005 he has been a member of the Council and Cases Committee of the Medical Defence Union.
Consultants in Emergency Medicine
C: Mr Peter Richmond
Mr Richmond was the full-time Consultant in Emergency Medicine in Poole from 2009 to 2014, having been Consultant in A & E in Wales (Cardiff Royal Infirmary and the University Hospital of Wales) since 1988.
D: Dr Gregor Campbell-Hewson
Dr Campbell-Hewson has been Consultant in Emergency Medicine at the Royal Hospital for Sick Children, Edinburgh, and the Edinburgh Royal Infirmary since 2012 (having previously served in the same capacity between 2004 and 2009) and was Consultant in A & E Medicine at Addenbrooke's Hospital, Cambridge, between 1998 and 2004 and 2009 and 2012.
Consultant Radiologists
C: Professor Steve Halligan
Professor Halligan was appointed Professor of Gastrointestinal Radiology at UCL in 2005 and remains in that position.
D: Dr Hartley Euinton
Dr Euinton has been Consultant Radiologist at Chesterfield Royal Hospital since 2004 and remains in that position
Consultant Microbiologists
C: Dr James Gray
Dr Gray has been Consultant Medical Microbiologist at the Birmingham Children's Hospital and the Birmingham Women's NHS Trust since 1995.
D: Professor Keith Cartwright
Professor Cartwright has been a Consultant Microbiologist since 1978 working primarily in public health with a particular interest in community-acquired infections. He is a member of the Medical Defence Union Cases Committee.
Consultants in Anaesthesia and Intensive Care
C: Dr Kenneth Power
Dr Power has been Consultant in Anaesthesia and Intensive Care in Poole since 1991 and Clinical Director for Anaesthesia and Critical Care since 2013.
D: Dr Dominic Bell
Dr Bell has been Consultant in Anaesthesia and Intensive Care at Leeds Royal Infirmary since 1992.
APPENDIX 2
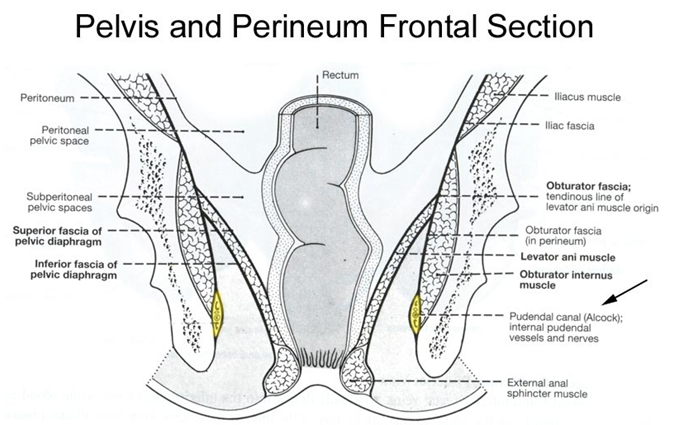 </P>
</P>
