Freely Available British and Irish Public Legal Information
[Home] [Databases] [World Law] [Multidatabase Search] [Help] [Feedback]
England and Wales High Court (King's Bench Division) Decisions
You are here: BAILII >> Databases >> England and Wales High Court (King's Bench Division) Decisions >> Gahir v Ola [2024] EWHC 390 (KB) (23 February 2024)
URL: http://www.bailii.org/ew/cases/EWHC/KB/2024/390.html
Cite as: [2024] EWHC 390 (KB)
[New search] [Printable PDF version] [Help]
KING'S BENCH DIVISION
Strand, London, WC2A 2LL |
||
B e f o r e :
(sitting as a Judge of the High Court)
____________________
| MR GURMUKH GAHIR (by his Litigation Friend Ms Gagun Gahir) |
Claimant |
|
| - and - |
||
| DR AYODELE OLUSGUN OLA |
Defendant |
____________________
Martin Porter KC (instructed by Gordons Partnership) for the Defendant
Hearing dates: 7, 8, 12-15, 19 June 2023
Judgment circulated in draft: 13 February 2024
Judgment handed down: 23 February 2024
____________________
Crown Copyright ©
- In November 2018 the Claimant had the misfortune to contract a rare viral disease namely Herpes Simplex Encephalitis (HSE). In some of the literature this is also referred to by the initials HSV (Herpes Simplex Virus) or HSVE (Herpes Simplex Viral Encephalitis). I will use HSE.
- The Claimant was then 43 when he contracted HSE, having been born on 30 September 1975. On Tuesday 27 November 2018 he saw his GP, the Defendant Dr Ola. What occurred at this consultation will be examined in detail in this judgment.
- On Friday 30 November 2018 the Claimant was admitted to hospital as an emergency. He was assessed. Administration of an anti-viral drug called acyclovir was commenced.
- The Claimant was very seriously ill. As Mr Horne KC put it in his written opening note, the Claimant has suffered a significant brain injury. He is and will be unable to live independently. He lacks capacity to manage his property and affairs and lacks litigation capacity. He brings this claim, for damages for personal injuries and other losses arising out of the alleged negligence of the Defendant, by his sister and litigation friend Ms Gagun Gahir.
- By order sealed on 11 March 2022 it was directed that:
- I am grateful to Mr Michael Horne KC, who appeared for the Claimant, and to Mr Martin Porter KC, who appeared for the Defendant, for their extremely helpful written submissions.
- The essence of the Claimant's case is:
- The essence of the Defendant's case is:
- This, as will become clear, is a dramatic over-simplification of the difficult issues which I must seek to determine in this case.
- I received written and oral evidence from four members of the Claimant's family, all of whom share the family name "Gahir". Without intending any disrespect, I shall accordingly refer to them by their first or given names.
- I received oral and written evidence from the Defendant.
- On behalf of the Claimant, I received written and oral evidence from the following expert witnesses:
- On behalf of the Defendant, I received written and oral evidence from the following expert witnesses:
- The report of Professor Almond, Consultant Physician was agreed.
- In making findings of fact, I have had regard to the entirety of the evidence, which includes materials relied upon which appear in the bundles, and which was provided during the trial. I remind myself that the Claimant bears the burden of proving all relevant matters on the balance of probabilities.
- Gee accompanied the Claimant to the consultation with the Defendant on Tuesday 27 November 2018 and was present with him during that consultation. She gives details in paragraph 3 of her witness statement of her science background. She has a BSc in Applied Biology and a Master's degree in neuroscience. She described pursuing a career in the pharmaceutical industry. In November 2018 she was an NHS Liaison Manager for a large pharmaceutical company.
- She was forceful when giving her oral evidence and had clearly come to court with an unshakeable belief that a wrong had befallen her brother. I am in no doubt that she genuinely believed what she was saying to be both truthful and accurate. I must nevertheless determine, as with all truthful witnesses, whether her evidence is accurate and reliable.
- Gagun, as noted, is the Claimant's Litigation Friend. I found her to be more measured in her oral evidence. She struck me as a careful truthful witness. Her evidence in general gave me confidence.
- Gurdip, the Claimant's mother, struck me as a truthful witness. As will become clear, when dealing with the timing of events around the time of the consultation on Tuesday 27 November 2018, she was more comfortable with the concept of days of the week rather than dates of the month. In my experience this is by no means unusual.
- Rupinder, the Claimant's wife, was again a truthful witness although her evidence was of limited scope in relation to the core issues in this case.
- The issue is whether on Tuesday 27 November 2018 the Claimant has proved that the Defendant was guilty of such failure as no General Practitioner of ordinary skill would be guilty if acting with ordinary care.
- The presentation of the Claimant at the consultation on Tuesday is clearly important, as is what the Defendant was told by Gee, who had taken the Claimant to the consultation and remained with him during the consultation. However, also important is what the Defendant knew or ought to have known about the Claimant from his previous observations of him and from medical records, the contents of which he knew or ought to have known.
- There is agreement that the relevant triad of presenting features which would have mandated urgent referral to hospital are:
- A recent history of fever and headaches was clearly given at the consultation. The contentious issue is the presence of the third component.
- Whilst it is intended that the facts stated in this part of the judgment are uncontentious, I am nevertheless satisfied that they have been proved on the preponderance of the evidence.
- The Claimant was known to his family as Sonny. He was employed as an IT consultant. In 2018 the family home was being renovated. The Claimant was living at Gee's home, separately from his wife and children. He had been with Gee since the summer of 2018.
- Gee knew something of the Claimant's medical history. She was aware that he had been told he had symptoms of irritable bowel syndrome (IBS) and coeliac disease. She also understood that he suffered migraines which she thought were associated with working with computer screens. She believed the Claimant was otherwise in good health and was someone "who would make light of any illness".
- The Claimant's wife, Rupinder, also referred in her witness statement to the Claimant suffering from migraines "for a number of years" which she said could be "quite severe". She too thought these were linked to working with computer screens.
- The Claimant made a trip to Paris over the weekend of Saturday and Sunday 24th and 25th November, returning home on Sunday evening.
- I will deal with the evidence of the consultation on Tuesday 27 November 2018 with the Defendant at which Gee was present at the end of this section. I start with the evidence of Gurdip and of the other evidence of Gee.
- In her witness statement, Gee says that the Claimant returned to her home from Paris, on Sunday 25 November 2018. He said he did not feel well and went to bed without having eaten anything. She was not aware at that stage that the Claimant had been to Paris.
- On Monday 26 November 2018 Gee went to work, returning at around 3.00pm or 4.00pm. She found "all the lights on in the house, which was unusual." She continues in her witness statement:
- Gee tried to arrange an appointment with a GP but could not get through on the telephone. She says she telephoned her mother, Gurdip, on Monday and it was Gurdip who arranged an appointment with a GP at 10.30am on Tuesday 27 November 2018. Gurdip suggested that Gee give paracetamol to the Claimant, which she did on Monday. She says that the Claimant took a packet to his room when he retired for the night.
- During the cross-examination of Gurdip, it was put to her that it was on Tuesday 27th November 2018 that she had first become aware that the Claimant was unwell. In support of that proposition, she was taken to paragraph 2 of her witness statement:
- Gurdip said that this was a mistake and that she had learned that the Claimant was unwell on Monday evening when Gee had telephoned her. Gurdip said that she had made the appointment for the Claimant to see a GP on Tuesday. I am satisfied that the reference in the witness statement to [Tuesday] 27th November is a mistake, and that Gee did telephone her mother on Monday evening and tell her that the Claimant was unwell.
- I am also satisfied that Gurdip went to Gee's house on Tuesday. This is consistent with the latter part of paragraph 2, and with paragraphs 3 and 4 of her witness statement. She went to see the Claimant on Tuesday and noted that he "was obviously unwell and was not himself". The witness statement continues:
- As I noted above, it became clear that Gurdip was more comfortable in dealing with days of the week rather than numerical dates of the month. I am satisfied that it was on Monday that Gee telephoned, on Tuesday evening that she went to see the Claimant and on Wednesday that Gurdip stayed with the Claimant.
- In her witness statement Gurdip says she arrived at about 9.00am on Wednesday and found the Claimant asleep under a duvet and sheet. He "appeared feverish and perspiring". Her impression during the day was that he was burning up with a high temperature, so she put a wet flannel on his forehead to soothe him.
- Gurdip says that the Claimant "periodically looked at his work phone in the morning and dealt with one or two work related tasks" and that although she tried to discourage the Claimant from taking calls he received one "from someone who had been locked out of their computer". Gurdip says she took the receiver and suggested the caller have a conversation with the Claimant on another occasion because he was feeling unwell. She said that she and the Claimant exchanged "small talk" over lunch. Although the Claimant answered questions from Gurdip and asked her if her office computer was working normally, she said that the Claimant was speaking normally but slowly.
- She was cross-examined about the work calls. She said that there were two phone calls in the morning which he answered but that he could not manage. She said that whatever questions were asked, he "muffled" and there was no proper response to the calls. She said she told the Claimant to put the phone down.
- In answer to questions from Mr Porter, Gurdip said there were three telephone calls, two from work and one in the afternoon from the surveyor concerning the building work at the house. She was firm in her recollection that the Claimant could not manage these calls. She said she took the telephone away from him when he answered it and told the caller that he should speak to another family member because the Claimant was not well.
- I accept the evidence of Gurdip as being truthful and accurate.
- Her written evidence may be summarized:
- Mr Porter's questions were in two parts. He firstly asked about some WhatsApp message exchanges between Rupinder and the Claimant before and after the consultation with the Defendant. Next, he asked about the Claimant's past medical history, in part recorded in some clinical notes of consultations following the Claimant's admission to hospital at which Rupinder was present.
- The purpose of the questions relating to the contents of the text messages was to show that the Claimant was not confused when he was seen by the Defendant.
- On Monday 26 November 2018 at 6.20pm the Claimant sent a message to Rupinder concerning the start of pipework and a lighting issue at the family home.
- On Tuesday 27 November 2018 at 8.20am Rupinder told the Claimant to "try and make a doctors app[ointment] if u can". The Claimant replied at 8.21: "Still sick can't see screens properly". Later, at 5.47pm Rupinder asked about the consultation with the Defendant. The Claimant replied at 5.54pm: "Ok confirm migraine and gave me some tabs, will see how it goes. Just wanna stop this nauseous feeling it's horrible". Mr Porter observed that the Claimant was able to report what had happened at the surgery, to which observation Rupinder agreed.
- Mr Porter referred Rupinder to various clinical notes, some made soon after the Claimant was admitted to hospital, but others made later in 2020. It was clear she had little or no recollection of the early meetings with clinicians, saying that "those days seem to be quite a blur". I accept that evidence. She agreed that the Claimant smoked and drank alcohol before his admission to hospital but she was unable to help with quantities because, as she said, she was not always with him.
- Rupinder agreed that the Claimant took a turn for the worse in summer 2020. She agreed that she and the Claimant spoke by telephone to Dr Price (Consultant Psychiatrist) in June 2020. The note of that telephone consultation is at pages 2007-8. It records that the Claimant had stopped taking sertraline, and that the Claimant's behaviour gradually changed. It was noted that the Claimant was spending "most of his time in his room". Rupinder explained that this was the position at the time, and that she and the Claimant were occupying separate bedrooms. In re-examination she said she believed that there was an association between the Claimant ceasing to take sertraline and the deterioration in his condition. She said that, following the recommendation of Dr Price, the Claimant started taking sertraline again.
- Returning to questions asked by Mr Porter, Rupinder agreed that in August 2020 she called 111 because the Claimant had now started hearing voices for the first time. Rupinder agreed with clinical notes made at the time which recorded a deterioration in the Claimant's condition over the last six months.
- I accept the evidence of Rupinder as being truthful and accurate. I do not consider that the WhatsApp messages to which she was referred show that the Claimant was not confused. The messages from the Claimant were short, many smart phones use predictive text, and in short, I do not consider the messages to be probative one way or the other.
- The same goes for messages between the Claimant and a third party, Rachel. Even though some parts were in French, I note the evidence of Professor Michael to the effect that alterations in mental state is very fluctuant in viral encephalitis, particularly in the early phases. He said of the Claimant that there were periods where he was able to do activities and periods when he wasn't. This seems to me to accord with the evidence of the Claimant's family members and explains, if explanation is required, why he was able to deal with the WhatsApp messages.
- The parts of her written evidence which I consider to be relevant may be summarized briefly:
- In cross-examination she was asked about her knowledge of the Claimant's past medical history. She said she was aware that over a number of years the Claimant has suffered from "some stress and anxieties" and that he had been off work for a significant period of time but could not remember if his time off work was related to chronic fatigue.
- She agreed that stress generally led to some fluctuation of mood, but she did not consider that her brother was of generally low mood in his constitution.
- On Thursday 29 November 2018 she thought the Claimant was not acting normally. In response to the proposition that it was later on Thursday evening, when she Face Timed the Claimant, that he had deteriorated to the extent that he had become confused. She said:
- In re-examination she said that before November 2018 she last remembered seeing the Claimant in September when he was in really good spirits.
- By way of introduction, the Defendant had been in practice as a partner at the New Medical Centre in Romford (the surgery) since 1996, having qualified as a doctor in 1985. He had seen the Claimant on several occasions since 2015, although the Claimant was also seen by other clinicians at the surgery. In oral evidence, the Defendant said that the Claimant had been his patient for 10 or 11 years at the time of the relevant consultation.
- The evidence of what occurred at the consultation comes from Gee and the Defendant. It will also be necessary to consider the contents of a telephone call made by Gee to the NHS 111 service on Friday 30 November 2018 which led to the Claimant's admission to hospital. The Defendant says that properly interpreted it demonstrates that symptoms of confusion or delirium were not present at the time of the consultation, but developed later.
- Gee's written evidence may be summarized. The Claimant said he was too unwell to drive himself to the surgery so Gee drove him. He also asked Gee to accompany him into the consultation, which had never happened before.
- It was cold when they set out, but the Claimant wore a t-shirt and light jacket. On the journey he wound down the car window, complaining that he felt "too hot".
- Gee dropped the Claimant off outside the surgery and went to park the car. Gee says that the Claimant, having exited the car, "appeared confused as to what to do next". She would normally have expected him to walk into the surgery. Gee thought he looked "lost". She told the Claimant to stand where he was until she had parked the car and returned. She took him into the surgery "holding his hand". She thought the Claimant appeared to be disorientated.
- As they went into the consultation room Gee says that the Claimant "was having to follow my instructions and was struggling to keep his balance."
- In the consultation room, Gee noticed that when the Claimant was speaking to the Defendant, "he was pausing for long periods of time and talking very slowly and quietly as though he was drained of energy." His response was "delayed, slow and slurred."
- Gee says she provided the Defendant with the following information concerning the Claimant:
- Gee says that she told the Defendant that the Claimant had appeared unclear what the consultation was for.
- As the consultation continued, Gee says that she occasionally completed sentences for the Claimant and occasionally responded to questions put to him. She felt that was unusual "and it must have appeared so to Dr Ola as he would not have ever seen me accompany Sonny to any appointment previously". Periodically she had to prompt the Claimant to respond to the Defendant.
- At paragraphs 35 and 36 of her statement, Gee describes the Claimant's behaviour and demeanour during the consultation:
- At paragraph 40 of her witness statement Gee says:
- Gee recalls the Defendant saying that the Claimant did not have a temperature. Gee told the Defendant that she thought it had been raised the day before. She says that the Defendant indicated that the Claimant had a history of migraines and that this was probably the cause of the current symptoms. Paramax was prescribed and the Claimant was advised to rest in a dark room with plenty of rest and fluids.
- Gee describes the end of the consultation in paragraphs 43 and 44 of her witness statement:
- Gee was asked some additional questions. She was asked how she would have responded if the Defendant had asked her if the Claimant was confused. She said she would have mentioned what had happened earlier that day and the day before. She elaborated upon that answer in this way:
- In cross-examination she was asked about her knowledge of medical conditions affecting the Claimant other than those she had already mentioned, namely IBS, coeliac disease, and migraines. Mr Porter was concerned that Gee had been selective in her witness statement about the Claimant's medical history. He asked her about the Claimant's history of work stress and chronic fatigue. Gee observed that this was correct and that "most of us have work stress". She said the Claimant was vocal about his health. She knew the Claimant was off work, (Mr Porter suggested in "2014, 2015") but she was not sure about chronic fatigue. At this point Mr Porter took Gee to notes of a neuropsychological assessment of the Claimant made in January 2019 at which both the Claimant and Gee were present. Gee agreed that much of the detail of the Claimant's past medical and family history were provided by her. However, she pointed out that:
- I accept that explanation. I accept in her witness statement the focus of her attention was the general state of health of the Claimant in the recent past before the consultation with the Defendant.
- Gee's recollection of the events in the consultation with the Defendant was the subject of sustained challenge by Mr Porter, with particular emphasis upon whether Gee had told Dr Ola that the Claimant was "confused, uncertain and fearful". Gee rejected the proposition that she had not told Dr Ola about this. However, in her first few answers, she did not expressly say that she had told the Defendant about these symptoms. Mr Porter took her to the part of the Letter of Claim dealing with the consultation with the Defendant. It is true that there is no express reference to "confusion" but there is reference to matters such as slow speech and the Claimant observing that the ground was moving. Gee relied upon this in her answers thus:
- Mr Porter was understandably anxious to seek to establish that any evidence of confusion on the part of the Claimant did not manifest itself until after the consultation with the Defendant. It is common ground that on Friday 30 November 2018 the condition of the Claimant deteriorated. Attempts to arrange a further consultation with a GP were unsuccessful. Gee says she was advised to telephone 111 or 999 if it was an emergency. She called 111. Mr Porter placed reliance upon a recording of the telephone conversations between Gee and various people to whom she spoke during the call. A transcript was prepared which was attached to Mr Horne's written note of opening. I listened to the recording, and I accept that the transcript is sufficiently accurate for the purposes of determining the issues raised in this case.
- The record of the 111 call shows that:
- I set out below what appear to me to be the relevant parts of the conversation with Naz which formed the subject matter of the questions from Mr Porter. I do not consider that the conversation with Dr Haque adds anything significant. The line numbers have been added:
- Mr Porter first asked about the exchange which resulted in Gee saying "Yeah, last night" (lines 6 to 8). In answer to the proposition that Gee was agreeing that there was "new confusion" which began on Wednesday 28 November 2018 Gee said:
- Mr Porter next referred Gee to lines 12 to 16. Her answer was much the same as before; that she was focussed "on the day" in relation to "new confusion". She continued:
- Gee explained that when she said "yesterday" (in line 15) she meant that this was when she noticed the new confusion, on Thursday. She disagreed with the proposition that the Claimant had not been confused on Tuesday when he saw the Defendant.
- The consistent theme running through her answers to questions from Mr Porter on this issue is that the Claimant's condition, including signs of confusion, worsened through Monday, Tuesday (when he saw the Defendant), through Wednesday and Thursday and finally Friday, when he was admitted to hospital. She was asked about a handwritten note made by the paramedics who attended in the ambulance which reads [Bundle 4, p1242]:
- During re-examination an issue arose whether the handwritten note in the preceding paragraph did or did not have a comma after the word "hallucinations". I am satisfied that it did, and that my typed transcription in the preceding paragraph is correct.
- Following Gagun's oral evidence it became clear to Mr Porter that that Gee should have been asked about some WhatsApp message exchanges between her and the Claimant. She was recalled and her attention was directed to Bundle 3 pages 886-7. At page 887 there is a screen shot of a message sent by Gee to the Claimant on Tuesday 27 November 2018 shortly before or after (it does not matter which) the consultation with the Defendant. She explained that it was information about phosphorus tissue salts used to alleviate fatigue. Mr Porter suggested they were also used in cases of depression. Gee said she was not looking at depression. She explained that she thought they would be good for replenishing electrolytes in the context of phosphorus being generally used for exhaustion, burnout and fatigue.
- She was also asked about a WhatsApp message at 12.11pm on Wednesday 28 November 2018 which reads: "I've booked an appt for you with Sarita on Friday 2.30. I'll take you there x." Gee explained that Sarita was a doctor she had met whom she thought might be able to help the Claimant "manage his IBS in a more holistic way". Mr Porter observed that on Wednesday Gee was planning to take the Claimant to see Sarita on Friday and suggested that "these texts are sent before your brother is confused". Gee rejected that proposition.
- I accept Gee's explanation concerning the reference to "new" confusion during the 111 call with the call handler Naz. She was referring to a deterioration in the condition of the Claimant rather than the onset of confusion which I accept began before.
- The Defendant's written account of the consultation is at paragraphs 13 to 23 of his first witness statement.
- The last time the Defendant had seen the Claimant before 27 November 2018 was on 31 January 2018.
- The Defendant says he remembers the consultation "because of the subsequent unfortunate events". In summary:
- The text of the Defendant's clinical note was helpfully set out in the opening note of Mr Porter, which I reproduce below:
- In his second witness statement, the Defendant dealt with the description of the Claimant given by Gee concerning his alleged confused state. He said that if the Claimant had presented as confused, uncertain or fearful, or with fidgeting or strange hand movements, or if these symptoms had been described by Gee, then he would have recorded them in his notes. He agrees that such symptoms would have indicated possible delirium or an occult infection. However, he says in paragraph 4 of his second statement that:
- At the start of the cross-examination of the Defendant, he was asked if he agreed that the triad of headache, history of fever and symptoms or signs of confusion would be a concern to all competent GPs. Understandably the Defendant agreed, subject to the caveat, which I think is fair, that it depends on what is meant by confusion. The Defendant later agreed that the terms confusion, cognitive impairment and delirium were interchangeable, observing that delirium is associated with confusion. In my judgment, based upon the evidence as a whole and in the context of this case , I have taken "confusion" to mean, as was submitted by Mr Horne, change in cognition, personality, behaviour or consciousness.
- The Defendant initially said that, reflecting upon the consultation, he did not see in the Claimant a confused man. This is a point he also made in his first witness statement. He said to Mr Horne that he had known the Claimant for "quite some time".
- The Defendant was taken through the Claimant's medical history as recorded in the clinical notes held by the surgery. Bowel issues were first noted in 2007, but it was in about 2015 that the Claimant began a series of fairly frequent visits to clinical professionals during which coeliac disease was diagnosed. The Claimant went on a gluten free diet and seemed to improve.
- The Defendant drew attention to old records beginning with a new patient registration on 4 August 2006 when a history of depression following a severe motor vehicle traffic accident in 2003 was noted. There is nothing to suggest that this was other than short lived and such depression is, in my judgment, entirely understandable.
- Between May 2015 and January 2016 there is no note in the records of low mood or anxiety. On 12 August 2015 the Defendant recorded complaints of gastro-intestinal symptoms of bloating, abdominal pains and fatigue. He noted "? psychosomatic, ? MUS [Medically Unexplained Symptoms]". He wrote a private referral letter to Dr Castle, Consultant Psychiatrist. The Defendant referred in that letter to " a whole host of medically unexplained symptoms including headaches". Later on he wrote: "he does admit to some emotional stress". In fact, the Claimant did not see Dr Castle. His medical insurance would not cover the cost. No NHS referral was made.
- The Defendant sought to give the impression that at each consultation with the Claimant where a complaint of headache was made, the Defendant conducted a careful examination and exploration of the complaint. However, it became increasingly clear during the course of cross-examination that this was far from the case. Looking at the note of consultation on 12 August 2015 there is no reference to headache. The reference to headache appeared in the letter to Dr Castle. The note of consultation on 12 January 2016 reads: "says he has got headaches and can't see the screen, and can't go to work and needs a cert[ificate]". Curiously, the Med 3 "sick note" was dated 5 February 2016 and covered the period 6 to 19 January 2016, giving the diagnosis "Abdominal symptoms". The Defendant was unable to explain how that Med 3 came to be issued or why that diagnosis was recorded, although he speculated that a colleague may have issued it.
- On 23 May 2016 the Defendant recorded "fatigue and tiredness, struggling with nausea, headaches and felling unwell also reports low mood discussed possibility of CFS [Chronic Fatigue Syndrome]". The Defendant agreed that this could have been the first occasion that CFS was mentioned. He said he could not remember "the specifics" of the day. A referral to a neurologist was made for 13 September 2016 but the Claimant cancelled it.
- The next consultation with the Defendant was on 21 July 2017. No reference to mood was noted. The problem noted was of a flare up of gastro-intestinal symptoms.
- The Claimant saw a Nurse Practitioner on 1 November 2017. The complaint was of "headache most of the time". The note recorded "Frontal headache", which the Defendant agreed was a coding from a drop-down menu on the computer. The Defendant saw the Claimant on 7 November 2017 for "review". The Defendant wrote "Migraine" and agreed with Mr Horne that this was the first time that he considered that the Claimant was suffering from migraine. There was than a series of medical appointments related to migraine which resulted in a prescription of amitriptyline on 31 January 2018. That was the last time the Claimant saw the Defendant before 27 November 2018.
- When questioned in more detail about each consultation, the Defendant was unable to give any details additional to those recorded in the clinical notes. In one sense that is unsurprising, but in the context of this case it is very important because, contrary to the impression which I find the Defendant was seeking to create about knowing the past history of the Claimant and using that as a reason for not always making a full enquiry about headaches, I am satisfied that for the most part, the Defendant made no, or no adequate enquiry. I am satisfied that the Defendant was prone to make assumptions without making specific enquiry. Indeed, at one point in his evidence he said: "there are many assumptions made when you know somebody. You just build a picture of them over time". The difficulty in this case is the "picture" was not documented and the Defendant has no recollection of anything beyond what is contained in the notes.
- At one point, Mr Horne suggested to the Defendant that he was making up his answers as he went along. That arose when Mr Horne was asking about the Claimant's absence from work for a period of 7 months between 4 June 2015 and 19 January 2016. The referral letter to the neurologist contained this: "His fatigue symptoms were so disabling he was off work for about seven months". I am satisfied from the medical records that Mr Horne was correct to put to the Defendant that the reason for that period of absence was abdominal symptoms. However the Defendant said the cause of absence was "possibly a combination of" fatigue and abdominal symptoms. Mr Horne pointed out that chronic fatigue did not feature in any of the Med 3 certificates. The Defendant said that seven months was a long time and "it's likely that if tiredness and fatigue came out in the history it may not be recorded here, although on occasions I did record it, but it's the duration of the illness which he had, in the absence of any serious disease, that prompted all these referrals and they mention that the fatigue was disabling". The Defendant refuted the suggestion that he was "making that up as he was going along" by saying: " no, because I know this patient so well and I'm just really reflecting my knowledge of him". I was and remain entirely unconvinced by that response. I do not find that the Defendant was "making it up". I think he was genuinely trying to find, in his own mind, reasons for his belief that he knew more about the Claimant's history than in fact, as I find, he did. However, it does in my judgment cast some doubt about two important matters:
- It is now appropriate to consider that consultation. At one point, when answering questions about the Claimant's presentation at the index consultation, and the contribution made by Gee, the Defendant said:
- Later on during the cross-examination he said that the Claimant answered the questions as briefly as he could. He thought that it was Gee who mentioned that the Claimant had headaches and that the Claimant "validated it by saying because I asked him as well by saying he had headaches". He agreed that the same went for the symptoms of nausea and fever ("burning up"), by which I find that it was Gee who reported the symptoms and the Claimant who validated this report. In short, the Defendant agreed that he could not necessarily remember who said what.
- It was suggested to the Defendant that in reality it was Gee who was having to clarify "just about every element" of the Claimant's history, to which the Defendant replied: "I think so, I think that's reasonable to say, yes." He also agreed that the consultation was not about a concern that the Claimant was unable to work, but it was about a concern about the Claimant's symptoms.
- The Defendant was pressed about what he had been told about the nature of the Claimant's headache or headaches and what enquiries he had made.
- The Defendant recorded in his clinical note "headaches" in the plural. He was asked about that. He said that the impression he had was that the Claimant had a series of headaches with gaps between them, but he could not remember who gave him that impression.
- He was asked about the gap of 10 months since the last time the Claimant had been seen, in January 2018. The Defendant said that he had not asked the Claimant about events during that period or whether the Claimant had suffered headaches. He agreed that if the question had been asked and the Claimant had said that there had not been any headaches during that period, that would not have deflected his diagnostic thinking in this case. The Defendant thought that in presentation it was "very much like" what he had seen in the past, meaning, I find, migraine. The Defendant did not seek to ascertain the location of the headache.
- He was then asked if the nature of the headache was "pounding". The Defendant said he could not recall. He was taken to paragraph 22 of his second witness statement:
- When he was taken to this passage in cross-examination, on day 3 of the trial, he was reminded that on day 2 of the trial he had said:
- His response to this was:
- He elaborated on this. He said he had two "patients", one of them being a worried sister Gee. He went on:
- The Defendant was reminded that Gee had said she did mention that the headache was pounding and that it was not a series of headaches. He was asked if the reality was that he did not ask many questions about the headache, but instead looked for evidence to confirm the "assumption" that this was a migraine. The Defendant said that the history of nausea, vomiting and sensitivity to smells was highly suggestive of migraines. He agreed that he was also given a history of the Claimant not leaving his room and not eating.
- Questions then turned to the history of fever. The Defendant agreed that he had been told that the Claimant had taken paracetamol and that this could bring down a temperature. He agreed that fever was not a symptom of migraine. He said he did not dismiss the history given by Gee that the Claimant had been "burning up", but was reassured by the fact that when he took the Claimant's temperature it was normal. Later on he agreed that the history was of "fever and headaches for a few days", indicating agreement with the proposition that both had started at the same time.
- The Defendant also agreed that Gee had "emphasised" that the Claimant was feeling more emotionally flat than previously. He agreed that this would be a significant part of the history. He was asked why he had not noted it. He said it was an error on his part in the sense that it was towards the end of the consultation, and he was running late.
- The Defendant agreed that there were concerns about the Claimant's behaviour but that "they were behaviours which he had had in the past and it looked like an exacerbation of them. That's the impression I had". However, he agreed that this was an assumption which he made. He also said that "the symptoms of not coming down, not interacting with family, not eating, is suggestive of an emotional disturbance... not of migraine in itself."
- He was questioned further about the Claimant's behaviour and agreed with the proposition that he had reached a view that the behavioural issues were due to a psychiatric cause, and it was this that led hm to providing a leaflet about CBT.
- Importantly, in my judgment, the Defendant also agreed that there appeared to be a temporal co-incidence between the onset of headache, the onset of fever and the onset of a mood disorder.
- Pressed on the issue of behavioural change, he stressed that there was limited time available in an NHS GP consultation, and that this consultation had already exceeded the usual 10 minutes allowed. He said that he would have "loved to" have gone into more detail about the low affect that the Defendant noticed and which Gee had reported. However, he said he made the assumption, based upon his knowledge of the Claimant from previous consultations, that the Claimant was "feeling down".
- I have sought to summarize the evidence of the Defendant by referring to what appeared to me to be the significant parts.
- It is obvious that the clinical note taken is very short and cannot possibly amount to a record of everything that was said or discussed in the consultation.
- I am satisfied that the Defendant was aware that the Claimant was suffering from headaches or a headache and that a history of fever had been given by Gee which was, or ought to have been, accepted at face value. The Defendant was aware that Gee had used the expression "burning up". The Defendant was also aware, or ought to have been aware, that the onset of headache and fever occurred at about the same time. The Defendant knew that fever was not a symptom of migraine.
- Gee's evidence gave me confidence. Making all allowances for my impression, noted at the start of this judgment, that Gee "had a story to tell" I am satisfied that her evidence was accurate. Her description of the Claimant's presentation in the presence of the Defendant in my judgment accords with the probabilities in this case.
- The evidence of the Defendant did not give me confidence. I find that during the consultation he felt overwhelmed by the situation that was unfolding before him. In answer to a question from me, the Defendant said he had not met Gee before. I am entirely satisfied that, even if he had, he would have no cause to remember her. However, I cannot ignore her scientific background. She was not a mere relative with no knowledge of clinical matters. She was convinced and rightly so, as it turned out that there was something seriously wrong with her brother. I am quite satisfied that she conveyed this in forceful terms to the Defendant. I observed at the outset of this judgment that she was "forceful when giving her oral evidence". I am sure that she was equally forceful when speaking at the index consultation.
- I can easily understand why the Defendant, now knowing of Gee's scientific background, would convince himself that he knew the Claimant better than in fact he did. I am satisfied that the Defendant was prone to assumptions, and I find that those assumptions were not justified. He did not appreciate the significance of what Gee was telling him. I do not find the Defendant to have been a GP who made full notes of consultations. This, coupled with my finding of a lack of appreciation of the seriousness of what Gee was telling him, explains why things which Gee told him are not recorded. Also, as the Defendant himself said, the consultation was, in his opinion, "chaotic". Whilst that may have made it difficult for him to record everything, it was his duty, as a professional clinician, to remain in control of the situation.
- In his first witness statement at paragraph 21, the Defendant says that he did not observe the Claimant fidgeting and making strange hand movements and that, had he been told of this or observed it he would have recorded it in his notes and been concerned about the Claimant. That same is true of the Claimant's response to questions being "delayed, slow and slurred". the paragraph concludes thus:
- I accept the evidence of Gee that the Claimant did behave as described. I discount the possibility that she is mistaken about when this behaviour manifested itself and I absolutely reject any possibility (which has not been suggested) that she has made this up. Her description of the Claimant's behaviour outside the surgery when she returned to the Claimant, having parked the car, is convincing. The Claimant's behaviour during the index consultation seems to me to be consistent with what Gee described outside the surgery.
- I am satisfied that the Claimant's behaviour during the index consultation, as described by Gee, must or should have been observed by the Defendant. I am unable to accept his assertion that he would have noted them. Having been taken through his other clinical notes I was not impressed by his note taking and, as I have found, I consider that he was overwhelmed by this consultation.
- In paragraph 22 of his statement, the Defendant says he does not recall a complaint of "pounding" headache, but this was dealt with in cross-examination. I am satisfied, for what it is worth, that the word "pounding" was used. I am also satisfied that reference was made in the consultation to a perception by the Claimant that the ground was moving and the room spinning.
- Dealing with paragraph 23 of the Defendant's statement, I am entirely satisfied that the description given by Gee of the Claimant's behaviour at the conclusion of the consultation is accurate. Once more the Defendant says he would have noted such behaviour in his notes had it occurred, but I am far from satisfied that this is the case.
- It follows that I am satisfied to the requisite standard that the evidence of what occurred at the consultation on 27 November 2018 is in all material respects as described by Gee.
- Dr Budd and Dr Barraclough were called "back-to-back" following the lay evidence.
- Both are distinguished clinicians well qualified to give expert evidence on what is to be expected of all reasonably competent GPs.
- Both agree that if I find, as I have, that Gee's evidence concerning what happened at the consultation is accepted, then breach of duty is established.
- That being so, it is unnecessary to discuss the alternative case of the Claimant, namely that even if I did not accept the evidence of Gee, the Defendant ought nevertheless to have referred the Claimant to hospital on Tuesday 27 November 2018.
- But for the breach of duty which I have found proven, it is likely, and I so find, that the Claimant would have been admitted to hospital on Tuesday 27 November 2018.
- Upon admission to hospital on Friday 30 November 2018, administration of acyclovir commenced very rapidly. I am satisfied, for reasons given below, that had the Claimant been admitted on Tuesday, commencement of acyclovir treatment would also have been rapid. The relevant delay in commencement of treatment is agreed as being 55 hours.
- What would have been the outcome if commencement of acyclovir had been commenced 55 hours earlier? Intuitively, one would think that the earlier the administration, the better the likely outcome. However, some of the evidence which was presented to me suggests that it may not be as straightforward as that.
- Acyclovir is not a "cure" for HSE. Acyclovir is shown to be useful in preventing further damage or at least slowing down the rate of damage. It is instructive, and indeed necessary, to explore this in a little more detail.
- Many of us are familiar with the expression "viral infection" and some at least with the concept of "viral load" as a means of expressing the amount of virus in an infected person's body. We often speak of the term "virus" in the context of describing the type of viral infection. In this case, it is the Herpes Simplex virus. I learned in the course of this trial that an individual viral particle is called a virion.
- What follows is an over-simplification of a complex process. HSE can begin with the introduction into a single brain cell of a single virion. That virion reproduces by a process of replication. The products of the replication process invade other cells. Having done so, the "new" virions themselves replicate. Cells invaded by virions are irreparably damaged, which is why acyclovir cannot repair such damage. Acyclovir does not "kill" virions. What it does is prevent the virions replicating. The manner and rate of replication is dealt with later in this judgment.
- There is agreement that acyclovir administration should commence as soon as possible. In general, most patients who receive the drug early do better than patients who receive it later. However, some patients who receive it early do not do so well, and some who receive it late do very well.
- Is it possible to say into which cohort the Claimant falls? That is what I must seek to determine.
- In determining the issue of causation in this case, it is necessary to consider the expert evidence as a whole, and not simply on a discipline-by-discipline basis. However, summarizing the evidence of experts of like disciplines is the easiest starting point. Before that, it is necessary to consider the progression of the Claimant's condition following his admission to hospital so as to put the expert opinions into context.
- In that respect, I have found the summary in the agreed report of Professor D S Almond, Consultant Physician, to be of use.
- The Claimant arrived at the Queen's Hospital Romford at 16.46 on Friday 30 November 2018. The Ambulance paramedics had recorded a Glasgow Coma Score (GCS) of 14/15 on account of confusion.
- At 16.49 intravenous acyclovir and chloramphenicol were prescribed. Administration began at 17.35.
- A CT head scan showed a hypodense area to a temporal lobe. An MRI scan was advised. When performed on 1 December 2018 the MRI scan showed changes suggestive of viral encephalitis. A sample of cerebro-spinal fluid (CFS) was obtained via lumbar puncture. The polymerase chain reaction (PCR) test results were not available until 7 December 2018. That test showed positive for HSE.
- On 4 December 2018 the Claimant's condition deteriorated to the point where he was admitted to the Intensive Care Unit. The admission clerk noted the GCS to be 6/15 at 19.25. That score represented a deterioration from a score of 9-10/15 noted by Dr Mattoscio (neurologist) earlier on 4 December 2018, (at 16.00, at page 1304) and later (10/15 at page 1309). In oral evidence both Dr Wreghitt and Dr Baker disregarded the 6/15 score as being unreliable. A deterioration in renal function was noted and believed to be related to the administration of acyclovir. The dosage was reduced.
- On 11 December 2018 the Claimant suffered his first seizure. In summer 2020 he developed psychotic symptoms.
- It was not possible to hear the oral evidence of Professor Michael and Dr Turner, Consultant Neurologists, back-to-back. The Radiologists Dr Das (Claimant) and Professor Jackson (Defendant) were interposed between them. However, the other experts in their respective disciplines were called back-to-back.
- The Claimant relied upon the evidence of Professor Michael. His self-penned "Biosketch" makes for hugely impressive reading. I accept without reservation his description of himself as "a world leading expert in the field of HSV encephalitis with an extensive clinical, policy, and academic expertise in up-to-date management of HSV encephalitis and its sequelae". In oral evidence he said he spent 90% of this time on academic work and 10% on clinical work. He has been involved in dozens of cases of HSE with patients either directly under his care or in a consultative role.
- Professor Michael's position was, crudely stated, that in cases of HSE there is a correlation between viral load, the administration of acyclovir, the immune response and outcome.
- The Defendant relied upon the evidence of Dr Turner. Since 2013 he has been an independent neurologist. Before that he was a consultant in neurology at the Portsmouth Hospital and the Wessex Neurological Centre in Southampton from 1983 to 2013. He said that for 30 years he dealt with all of the acute neurology cases in the region. In cross-examination he said he had seen "less than ten" cases of HSE in his 30 years in practice.
- Dr Turner's position was, crudely stated, that in cases of HSE there is no correlation between the viral load, the administration of acyclovir, the immune response and outcome. In support of this position, he relied upon a paper published in 1997 in the American publication "Neurology". The lead author is B.Wildemann (the Wildemann paper). In that study, CSF samples were taken from eight patients with HSE. I deal later in more detail about his evidence in relation to the Wildemann paper. It is fair to say that Dr Turner does accept that there is a non-linear relationship between viral load and the immune response.
- Before examining the respective positions of the neurologists, including in relation to the literature, it is helpful to start with their evidence recorded in their joint statement. The key question, in my judgment, is number 15 which had several parts. I summarise the responses which I consider to be relevant.
- The question with relevant answers is set out below:
- Professor Michael was firmly of the belief that there was a direct correlation between the viral load and the ultimate outcome for the patient. Cross-examined directly on that point, with reference to literature that measured the burden of virus in CSF Professor Michael explained that the viral load discerned from CSF was a "poor proxy of what's happening in the brain". He said:
- Professor Michael was asked to comment upon the effect of the viral load upon the immune response, whereby (in grossly simplistic terms) the body's immune system begins to attack cells in the body. The proposition put to him was that the indirect mechanism of the immune response was not related to the viral load. Professor Michael disagreed. He said: "It's both. The immune response is proportionate to the viral load". He went on to explain that acyclovir halts viral replication in the cell where the replication activity is happening. At this stage I should say that at various times the experts in this case have referred to the "immune response", the "auto-immune response" and the "inflammatory response". I am sure that each term has a technically different meaning, but for the purposes of the body's response as it affects the brain secondary to infection by the HSE virus, I have taken them to mean broadly the same thing.
- Moving to the relevance of the development of psychosis in mid-2020, Professor Michael was of the opinion that, having regard to the neuroradiology reports, they were consistent with the Claimant having suffered quite a significant brain injury. He described what was shown on the imaging and said that these "very clearly were insults from HSV encephalitis and nothing else". Thus, to the extent it was being suggested that the psychosis in 2020 was unrelated to the HSE, he rejected that proposition.
- Professor Michael was firm in his view that "a delay of three days in starting the effective antiviral drug acyclovir would have a material impact on the outcome for a patient with HSV encephalitis; that includes factors which are cognitive, neuropsychiatric also".
- His attention was next drawn to a paper by Sir Peter Kennedy et al (2013) published in 2013 in the Journal of NeuroVirology which Professor Michael had referred to in his report. The quote in the report from the paper was:
- Mr Porter postulated that this provided some support for the suggestion that there is a level of uncertainty in predicting what the outcome will be in a particular case, depending on how quickly the administration of acyclovir is commenced. Professor Michael explained that the authors said clearly that a delay in commencement of administration of acyclovir of over 48 hours was associated with a "materially worse outcome". He said that the authors were making the point that unlike bacterial meningitis, where one can calculate in hours how well or poorly someone might do upon commencement of IV antibiotics, for viral encephalitis it is more insidious and it is hard to make a distinction in the one-day window, but certainly it is well supported that delays of two days or more are associated with a worse outcome.
- Professor Michael was unimpressed with attempts to categorise the quality of outcomes by reference to linear scales, particularly in relation to what he described as "historical literature" from the 1980s and 1990s. This is because the treatment for HSE has moved on "markedly" since then. Professor Michael thought this was also the position in relation to a retrospective study of patients from 1991 to 1998 by Raschilas et al (2002) entitled: "Outcome of and Prognostic Factors for Herpes Simplex Encephalitis in Adult Patients: Results of a Multicenter Study". That paper made reference to SAPS II (Simplified Acute Physiology Score II).
- Once more, Professor Michael was not impressed. He explained that SAPS II is not used to categorize outcome. It is a physiological score, used for cases of sepsis. In the joint statement, Question 13 touched upon a different scale, the Extended Glasgow Outcome Scale which categorises outcome by reference to eight classifications. Both Professor Michael and Dr Turner had reservations about this scale, but both agreed that the Claimant was at the time of the joint statement at Grade 3 (Lower Severe Disability) or Grade 4 (Upper Severe Disability).
- Professor Michael was asked to comment upon the fact that the Claimant's GCS, and SAPS II declined after administration of acyclovir had commenced. He gave a comprehensive answer. He said that this occurred in most cases involving severe infections. For example, once antibiotics are started to treat bacterial pneumonia, a patient will take some time to improve. He said this was particularly true for viral encephalitis and that it was very much within the normal history of someone with HSE to deteriorate despite administration of acyclovir. He emphasized that the earlier antiviral treatment starts, the faster the virus is cleared and, importantly, the less the inflammatory response.
- There then commenced an extremely important investigation of the probable outcome had acyclovir administration been commenced earlier. Professor Michael thought that on the balance of probabilities the Claimant would fall within that band of 40% to 60% of people, depending on which study was looked at, who would have made a very good outcome. He deferred to the neuroradiologists on the issue of whether a CT scan performed on Tuesday 27 November 2018 would have been normal or not. Subject to that he thought all the other prognostic factors would very much have put the Claimant in the good prognosis group. He repeated that the single biggest modifiable factor is the time from the onset of symptoms to commencement of treatment with the antiviral drug, which he said "we know works".
- The radiology evidence is dealt with more thoroughly below, but it is convenient to note at this stage that that one cannot say what a CT scan undertaken on 27 November 2018 would have shown.
- Professor Michael elaborated on his opinion on outcome. He said that many patients who have had HSE continue with symptoms such as headache and fatigue. Professor Michael thought the Claimant's outcome would have been "materially better than it currently is" because of a three-day delay in starting acyclovir administration. He thought this was a matter borne out in both his clinical experience and in the literature.
- In re-examination Professor Michael explained that "materially better" meant a more than negligible, substantial better functional outcome. He also explained that more than half of HSE patients will have some degree of deterioration during their admission. This could be a fall in the GCS score, increasing psychotic behaviour or seizures. He said: "the likelihood of the severity of that deterioration is best predicted by any delays in starting IV acyclovir". He justified this on the basis of his clinical experience and in the literature which he had outlined in his report.
- Somewhat unsatisfactorily, during re-examination, Professor Michael referred to a paper not previously in evidence of which he is the lead author. It was published in 2020 in Cell Reports ("the Cell paper"). It described a study where the brains of cloned mice were injected with the Herpes Simplex Virus and then treated with acyclovir.
- To describe the paper as a "dense read" is rather to understate the extreme technical nature of the paper. Moreover, the suggestion seems to have been that there was a comparative study of different groups of mice who were injected with different concentrations of the virus. However, I am far from clear that this is the case, as was Dr Baker. In the end I think it best to draw no conclusions from this paper, which his why I shall not summarize the evidence of Professor Michael or of Dr Baker about that paper.
- In oral evidence Dr Turner told me about his experience, as outlined above. He said that had acyclovir administration been commenced on Tuesday ("three days earlier"), the Claimant would have been "largely in the same clinical condition as he is now". He went on to elaborate. On the balance of probabilities, he thought:
- He summarized the effect on the Claimant of that opinion by saying that it would make a difference to his quality of life but not an enormous, large or significant difference to the way the Claimant's brain functioned.
- Mr Horne asked Dr Turner about the various outcome scales referred to in the literature and in the Joint Statement. I have mentioned the Extended Glasgow Outcome Scale when dealing with answers to Question 13 in the Joint Statement earlier. At Question 14 in the Joint Statement, the Neurologists were asked what level the Claimant would have been if acyclovir administration had begun on 27 November 2018. Professor Michael thought Grade 6 (Upper Moderate Disability) or Grade 7 (Lower Good Recovery) "and would be independent". Dr Turner thought that the Claimant would "still be in the condition that he is, not fully able to look after himself but can be left alone for more than 8 hours. On the Extended Glasgow Outcome Scale that would remain at 4" (Upper Severe Disability), which is the worse of the two "severe disability" Grades which both experts thought represented the Claimant's condition at the time of the preparation of the Joint Statement.
- Somewhat confusingly, there are two other scales namely the (ordinary) Glasgow Outcome Scale, using 5 levels of outcome, and the Modified Rankin Scale, using 6 levels of outcome. In relation to the Modified Rankin Scale, Dr Turner repeated his reservations about the appropriateness of using that scale, observing that it was for stroke victims.
- On the 5-point Glasgow Outcome Scale, Dr Turner agreed that the equivalent to Grade 3 or 4 on the Extended Scale was 3 (Severe disability; patient dependent for daily support) but making the fair point that "these are very broad categories" and that so far as Dr Turner was concerned, the Claimant was "not dependent for daily support", although he acknowledged that he lived with his family and was dependent on them. He agreed that the Claimant needs support on a daily basis for activities in respect of which he would otherwise have been independent.
- Dr Turner was asked about a paper to which Professor Michael had relied upon in his report. The lead author is Sylviane Defres. Professor Michael is the third named of many co-authors, of whom Dr Das is also one. Outcomes of HSE patients were assessed at discharge and at 12 months post-discharge. The 5-point Glasgow Outcome Scale was used. In his report, Professor Michael said, interpreting a bar chart in the paper, that at the 12-month stage, 41% of patients had a score of 5/5 and 30% had a score of 4/5. Grade 5 is "Good recovery; resumption of normal life with minor neurological and psychological deficits. Grade 4 is "Moderate disability; patients independent in daily life." The patient cohort was enrolled between December 2012 and December 2015. The conclusion of Professor Michael was that the 71% of patients within Grade 4 or 5 were independent at 12 months post discharge. At paragraph 35 of the Joint Statement (dealing with Question 14) he said that this score reflected either "'no need for assistance in everyday life, employment is possible but may require special equipment' or 'light damage with minor neurological and psychological deficits'".
- Dr Turner's view was that the Claimant's current condition was such that he was within GOS Grade 3: "Severe disability; patient dependent from daily support". It was Dr Turner's view that the same outcome would have prevailed had acyclovir administration been commenced on Tuesday 27 November 2018. This was explored by Mr Horne. He suggested to Dr Turner that the study showed that with modern treatment the high majority of patients treated in UK hospitals between 2012 and 2015 remain independent.
- Dr Turner's objection to the study was that the numbers were low, although he agreed there were more patients than he had seen in his personal experience, and they were more recent than he had seen in his experience. Dr Turner accepted that he had no experience of a patient being treated in 2018. It is clear to me that his experience was limited to ten patients during his front-line NHS practice ending in 2013. It is right to observe that the authors of the Defres paper themselves recognised that although their study was one of the largest prospective studies of unselected patients with encephalitis, "the size was limited" - see line 343 of the report, to which Dr Turner's attention was drawn in re-examination.
- The suggestion made by Mr Horne was that Dr Turner held an overly pessimistic view about the likely outcome of treatment of HSE in the recent era in the UK hospitals. He did not accept that proposition, although he agreed that the Claimant's outcome was "a minority outcome". This was despite, he acknowledged, that on Tuesday 27 November 2018 the Claimant's presentation was not unusual and was at the milder end of the spectrum. Dr Turner was referred to the Joint Statement and to Professor Michael's response to Question 14, dealing with the Defres paper. Professor Michael explained that the time of administration of acyclovir was available for 49 patients with HSE. Acyclovir was given early (within 48 hours of admission) in 35 cases. Professor Michael utilised the Modified Rankin Score to measure outcome. For 30 of those patients, it was between 0-3/6. A score of 0 is "No symptoms". A score of 3 is "Moderate disability. Requires some help, but able to walk unassisted". A poor outcome (4-6/6) was observed in 5 (14%) of the 35 patients. The remaining 14 patients (of the cohort of 49) received acyclovir later than 48 hours after admission. Of those 14 patients, 4 (29%) had a favourable outcome and 10 had a poor outcome.
- Having put those matters to Dr Turner, Mr Horne suggested that it defied logic to say that the Claimant would have had "the same unusual outcome if treated on [Tuesday 27 November 2018] in any event". Dr Turner's response can be summarized thus:
- Dealing with the inflammatory reaction, Mr Horne suggested that it would have been proportionately lower if HSE had been treated three days earlier. Dr Turner disagreed. The response would have been lower but "not necessarily proportionately lower". Dr Turner agreed that there was a relationship between viral load and the immune response, but he said it was not linear. Dr Turner thought that the Claimant's auto-inflammatory response was "extremely strong". He did not think it was highly unusual, but it was unusual. Dr Turner agreed that there was nothing "explicit" in the published literature that would help indicate whether the timing of the deterioration four or five days after commencement of acyclovir was of itself unusual. Mr Horne had earlier dealt with the rate of increase in viral load. Dr Turner agreed it was "exponential" although Dr Baker, in his evidence, disagreed with that word. Dr Turner had also earlier agreed that the viral load had been allowed to "exponentially grow" because of the delay in administration of acyclovir, that this led to a "significantly increased number of brain cells affected, and "a significantly increased level of inflammatory response because of the relationship with viral load".
- In re-examination Dr Turner was asked to give reasons for his opinion that the Claimant would have suffered a psychotic episode even if treatment had commenced on Tuesday 27 November 2018. Dr Turner said that HSE caused brain cellular damage. The immune response to that damage caused damage to the Claimant's neurobehavioural pathways "very severely" and that led him to have a lack of control over his sense of reality. Importantly, Dr Turner thought that would have happened "because of the very severe damage to his brain" if treatment had commenced earlier. He also thought that intensive care on 4 December 2018 would have occurred in any event because it is "not uncommon that there is an early deterioration after the onset of treatment".
- He was also taken to the Defres paper and to the part of the Joint Statement dealing with Professor Michael's response to Question 14. Dr Turner was asked to say where the Claimant was in the Modified Rankin Score. He thought score 3. On that basis, the Claimant's outcome should be classed as "favourable" and thus equivalent to the minority of 4 out of 14 patients (29%) who received acyclovir late but who had a favourable outcome.
- There was little relevant difference between the opinions of Dr Das and Professor Jackson. In my judgment, both experts were eminently well qualified to give evidence about relevant matters in this case.
- The first CT scan of the Claimant's brain was undertaken on 30 November 2018. The report by the radiologist (Dr Chawda) was in these terms:
- Mr Porter correctly submitted that any opinion of the reporting radiologist is inadmissible opinion evidence. The contents of the report are admissible only to the extent it comprises factual evidence (32PD 27.12). However, at their joint meeting the experts were asked whether they agreed with that report. They said that they did.
- The focus of inquiry was whether it was possible to say what would have been seen had a CT scan been undertaken on Tuesday 27 November 2018. The relevant question asked in advance of the joint meeting was question number 3: "If a brain CT scan had been undertaken on 27/11/18 on the balance of probabilities what would it have shown?"
- Dr Das opined that it "would have almost certainly been normal with no detectable abnormality". Professor Jackson opined that "there is a possibility that a CT scan on 27/11/18 may have shown some temporal lobe abnormality".
- The basis for both opinions was the respective interpretations of the radiologists of the CT scan undertaken on 30 November 2018. Dr Das thought there were "subtle" changes to the right temporal lobe shown on the scan. Professor Jackson thought the scan showed "marked" changes to the right temporal lobe. Images were reproduced at pages 326 (report of Dr Das) and 432 (report of Professor Jackson) of the bundles. Because the images look from the base of the spine upwards, the right side of the brain is the left side of the image and vice versa. Dr Das had superimposed yellow arrows over the images to highlight an area on the right side of the brain which is slightly darker than the corresponding area on the left side of the brain. He categorised that difference as "subtle".
- Looking at images of the same areas, Professor Jackson categorised the difference as marked. It may be that the difference between them is the interpretation of the terms "subtle" and "marked". Professor Jackson explained in oral evidence, in answer to a question from me, that for him "if something is subtle, you have to be able to consider that it might be normal and you are over-reporting it, and I would not consider that to be the case when I was reporting this film". Referring to images of the scan at page 432 of the bundles, (part of his report) he showed me the location of the middle cerebral artery which he said was displaced forwards. That, said Professor Jackson, "is clear evidence of swelling".
- I accept that interpretive evidence. However, whether the change should be categorised as a subtle change, or a marked change does not seem to me to matter much, if the purpose of the inquiry to assist in determining whether it is possible to say what a CT scan undertaken on 27 November 2018 would have shown. That is because I interpret the answers to question 3 in the joint report to mean that, on the balance of probabilities, no temporal lobe abnormality would have been detected on a CT scan undertaken on 27 November 2018. It is possible that some abnormality may have been apparent, but that is not enough to make a finding on the balance of probabilities that such abnormality would have been there to be seen on a CT scan.
- This was confirmed in oral evidence during questions asked of Professor Jackson by Mr Porter. He asked whether one can sensibly infer what a hypothetical CT scan on Tuesday 27 November 2018 would have shown. Professor Jackson gave a long but helpful answer:
- Dr Das said that his understanding of various studies was that in most patients, a CT scan taken within 48 hours of the onset of symptoms of HSE would show no changes. Professor Jackson's view is the contrary. However, given my finding on the evidence of both experts that they cannot predict what would have been seen on a scan taken on 27 November 2018, this again does not seem to me much to matter.
- In my judgment, and for the avoidance of doubt, the changes shown on the CT scan undertaken on 30 November 2018 do not enable me to make any finding about the speed of progression of the Claimant's HSE. The scan undertaken on 4 December 2018 showed what Dr Das described as "florid changes" and I did not understand Professor Jackson to disagree with that description. I accept that the progression of HSE can be rapid, but as Dr Das said in answer to a question from Mr Porter, it is not possible reliably to date the onset of symptoms of HSE from the CT scans in this case, which evidence I accept.
- Although Dr Baker was asked by Mr Horne about the Cell paper produced by Professor Michael, I do not recite that evidence because I have decided it is unsafe to place any reliance upon that paper, as explained above.
- Dr Tim Wreghitt gave expert evidence on behalf of the Claimant. He is a Consultant Clinical Scientist. He explained that he trained first as a scientist. He was awarded a Doctorate (PhD) in Microbiology and finally became a Member of the Royal College of Pathologists (MRCPath) by examination in virology. He became a Fellow in 1994. In 2008 he was awarded the OBE for services to public health virology. With almost 44 years relevant experience he has seen between 30 and 40 patients with HSE.
- Dr Robert Baker gave expert evidence on behalf of the Defendant. He qualified in medicine. He became a Member of the Royal College of Physicians (MRCP) in 1992. In 2000 he was awarded a Doctorate (PhD) in Microbiology. In 2005 he became a Fellow of the Royal College of Pathologists. He explains in his report that he is not a full time virologist, but treatment of patients with suspected or proven herpes meningitis and encephalitis HSE is a common and frequent clinical aspect of his work.
- There was an irreconcilable divergence of opinion between the virology experts. For the Claimant, Dr Wreghitt maintained his position expressed in the Joint statement in answer to question 5. That question was:
- Dr Wreghitt's opinion to part a) was that the Claimant would have been left with less severe neurological damage, but it was not possible to specify which aspects of his neurological function would have been improved. To part b) he answered: "No".
- The material part of Dr Baker's opinion to part a) was that " the likely benefits to earlier treatment would have been marginal, subject to the opinion of the neurologist". To part b) he answered: "No but marginal, subject to the opinions of neurologists".
- Dr Baker maintained that view during intense cross-examination by Mr Horne. Dr Baker's final position was elicited at the end of cross examination by Mr Horne:
- Despite that irreconcilable difference of opinion, there were areas of agreement. In the joint statement, the manner in which acyclovir prevents the herpes simplex virus replicating was explained in far fuller and agreed detail than the simplified version I have given. In the joint statement it was emphasised that acyclovir will not remove virions from cells that are already infected. This means that such cells remain susceptible to lysogenic, auto-immune damage despite the presence of the drug.
- Dr Baker went on to make additional comments which were not endorsed by Dr Wreghitt at the time that the Joint Statement was signed. However, in oral evidence, despite some hesitation and reservations, he did broadly agree with the additional comments, adding his own views on some of the issues. Dr Baker's additional comments are shown in quotation marks:
- Dr Baker concluded his above observations in the joint statement by saying: "All of these observations indicate that herpes virus continues to reproduce after the initiation of acyclovir therapy and that suppression of virus is unpredictable and not permanent." Dr Wreghitt said that he was not ready to sign up to that at the time the joint statement was prepared. He did not think that suppression of the virus was unpredictable, and made the point that suppression was permanent once it had happened, but ultimately he was prepared to agree.
- With reference to the GCS scores, the experts agreed that it was 14/15 upon admission and that it dipped to 9/15 on 4 December 2018. A GCS of below 10 upon commencement of administration of acyclovir is associated with a poor outcome. Both experts discounted the GCS score of 6/16 recorded by the ICU admission clerk on 4 December 2018.
- Question 4 of the Joint Statement was concerned with whether the treatment of the Claimant with acyclovir would be defined as "late". It is agreed that the Claimant probably had HSE on Sunday 25 November 2018. The experts agreed on four relevant clinical indicators:
- On the above basis, the experts agreed that indicator (3) would "indicate late disease, and even that depends on the opinions of other experts as to the claimant's condition" on Tuesday 27 November 2018. Dr Baker referred to the SAPS II. Questioned by Mr Porter whether by reference to that scale the Claimant was doing "well" Dr Wreghitt said he could not object to that proposition.
- The sticking point is the final observation by Dr Baker where he:
- There was discussion about the rate of replication of the virus, and in particular, whether it was exponential or some other growth rate. Dr Wreghitt was not entirely comfortable with "exponential", describing the growth rate as more akin to a chain reaction.
- The response of Dr Wreghitt to the Wildemann paper was similar to that of Professor Michael, namely that an eight-patient study was a very small sample. He also was concerned at the use of CSF samples that may have been frozen and thawed, perhaps more than once, an issue dealt with by Professor Michael in his evidence. Dr Wreghitt was concerned about whether the CSF viral load would reflect the viral load in the tissue in the temporal lobes. I took that to mean that there may be a high viral load in the brain even though the viral load in the CSF sample may be low, a point made also by Professor Michael. Dr Wreghitt believed that the higher the viral load, the more damage is caused. He said that, in animal studies, "that's been proved to be the case".
- The issue of the viral load and extent of the auto-immune response was also discussed. In answer to questions from Mr Porter, Dr Wreghitt said that the immune response to HSE was quite complicated. He said that the white cell response results in inflammation and "a lot of damage". In re-examination this issue was revisited by Mr Horne. Dr Wreghitt explained the mechanism of damage in this way. A single virion infects a neuron. The process of replication begins and "now you have hundreds of thousands of viruses". He said that the white cell mediated response "kicks in" creating damage which gradually cascades through. He said there was definitely a relationship between viral load and the immune response: "if you look at any time point, there's less virus present, less damage present, less immune response". He said the relationship was not linear. Thus, said Dr Wreghitt, in this case, if one went back three days, there will be less virus "for sure", less neuronal damage "for sure" and "probably less cellular damage through the white cell mediated response".
- Dr Baker also had views about the relationship (if any) between viral load and immune response. He said that viral replication was not exponential. Viral replication is constrained by a number of factors. In some cells, the virus cannot get in. In other cells, the product of viral replication cannot get out to infect other cells. Relying upon the Wildemann paper, he said that there was not a direct relationship between viral load and the amount of damage to the brain the auto-immune response. He acknowledged that there were only eight patients, but nevertheless believed that if there was a direct relationship, it would have been seen in these patients.
- Mr Horne asked Dr Baker if he accepted in general terms that the lesser the amount of virus, the lesser the damage caused by the immune response. Dr Baker did not agree, on the basis that the immunological response was idiosyncratic, so that the amount of virus in the body does not necessarily reflect the patient's ultimate outcome. I thought that was an unhelpful response. The question was put "in general terms" and I readily accept there will always be patients whose immune response does not follow the norm, in other words there will always be outliers, but the general view amongst the other experts was that there was a relationship between the viral load, the immune response and outcome. I thought this inability to assist in answering in general terms a question that had been postulated in general terms undermined the reliability of his opinions.
- Professor Michael had referred in his first report to a paper by Sili et al entitled "Herpes simplex virus encephalitis: Clinical manifestations, diagnosis and outcome in 106 adult patients". It was published in Journal of Clinical Virology in 2014. Mr Horne explored why Dr Baker had not referred in his report to this paper which, said Mr Horne, demonstrated a neurologically worse outcome from a delay in treatment from the onset of the first presenting symptom. Dr Baker could not remember. He was then asked to imagine that the Wildemann paper was discounted as being unreliable. In those circumstances, would Dr Baker agree that it is logical that the amount of central nervous system viral load is directly related to the severity of tissue damage? Dr Baker did not agree. He pointed instead to an alternative explanation of the cause of tissue damage which he said may not or will not necessarily be related to the viral load. This alternative explanation is that cells which are infected with the virus will express cell surface proteins on the surface which will trigger auto immune damage. The number of virions required for this to happen is unknown "but it may be a small number".
- Mr Horne then asked a series of questions based upon the proposition that the immune response was white cell mediated and that the trigger for this was the presence of the virus. The virus results in a protein being present on the surface of a cell and it is the presence of the protein which attracts the immune cascade. Dr Baker agreed with that sentence. He also agreed that there is damage to cells caused by the pathogen (virus) "essentially leaving a protein which will also attract inflammatory cascade" as Mr Horne put it. Given those answers Mr Horne suggested that "it is all related to the pathogen". Dr Baker agreed that this was the case "initially". Then came the important proposition that the more pathogen there is at any one point, the greater the immune cascade would be. Dr Baker said that one could not say that "with any certainty whatsoever". Asked if it was the likely position, Dr Baker said the likely position would be determined by how much virus there was in any individual cell which was being attacked. He also said that damage can continue after the virus has gone. I have to say I found Dr Baker to be guarded in his response to these propositions from Mr Horne, which seemed to lead on from the issue identified by Dr Baker about the significance of the presence of protein on the cell surface.
- Returning to the Wildemann paper, Mr Horne pointed out that there were only eight patients and that samples of CSF had been taken at different stages of the disease from different patients. He suggested that in those circumstances the paper was unreliable in terms of showing that there was no relationship between viral load and outcome. Dr Baker's response was that this was the only study that looked at humans and it did not show a relationship between viral load and outcome. In response to an earlier proposition that a sample of eight patients was so small that it renders any conclusions invalid:
- Dr Baker's final position was that there is a sub-set of patients for whom acyclovir makes "very little difference" because of their particular individual immunological makeup. In his opinion, the Claimant had an immunological reaction to HSE which manifested itself on day 5, such that the likely benefits of earlier treatment would have been marginal. He qualified that opinion by saying that it was:
- It is axiomatic that in every case, regard must be had to the entirety of the evidence before findings of fact can be made. That said, in some cases it is possible to confine findings derived from expert evidence by considering the evidence of experts of like disciplines. In this case, given the disciplinary overlap of topics dealt with by the experts, it would be impossible to form any view without considering all of the expert evidence together, although the contribution to this judgment by the GP experts is necessarily limited given my findings of fact concerning what happened at the consultation with the Defendant.
- As between the Neurology experts, there can be little doubt that Professor Michael is probably the leading neurological expert in the country in the field of Herpes Simplex Viral Encephalitis. His practical experience was more extensive and recent than that of Dr Turner. His published research portfolio is clearly the result of prolific academic work. Professor Michael referenced many relevant papers. Dr Turner referenced no published papers. That would not necessarily matter if the expert has extensive practical experience, but in my judgment practical experience of ten patients with HSE does not trump the opinions of Professor Michael supported as they are by practical experience of many more patients and supported by peer reviewed academic papers, many of which were co-authored by Professor Michael.
- I am nevertheless grateful to Dr Turner for sharing his genuinely held beliefs which were useful as a "sense-check" when considering the opinions of Professor Michael in areas where their opinions differed.
- There was minor debate about the use of the word "exponential" to describe the rate of viral replication and the spread of the virus in the brain. Dr Wreghitt vacillated a little. Dr Turner agreed with the use of the word. Dr Baker was having none of it.
- My assessment of the evidence concerning rate of viral replication is that even if the growth rate is not truly exponential, because the amount of material which is released from an individual virion is not constant, which I think is what troubled Dr Wreghitt, it is certainly very rapid. It may be that hundreds of new virions are produced, or it may be measured in the tens. Also, it appears, as Dr Baker said, that the virus cannot get into some cells and in other cells the product of viral replication cannot get out. Be that as it may, and as indicated above, it is clear to me that even if "exponential" is not precisely the correct term, the rate of replication increases over time as more material is released from individual virions to invade other cells which in turn results in those new virions releasing more material and so increasing the viral load in the brain.
- Dr Baker is himself an outlier amongst the experts on the issue of the relationship between viral load and the immune response. He would not agree with the proposition "in general terms" that the lesser the virus, the lesser the damage caused by the immune response. Instead, he relied upon his own theory, unsupported by any literature to which my attention was drawn, that proteins in the surface of cells which had been expressed from virions would trigger an immune response unrelated to the viral load. It is the absence of a relationship between viral load and the immune response which sets him apart from the other experts.
- To the extent that Dr Baker relied upon the Wildemann paper to support his opinions, I accept the evidence of Professor Michael concerning the limitations to that paper. It is relatively old (1996) and does not reflect more recent advances in the treatment of HSE. There were only eight patients. The timing of CSF sample collection was not uniform, and I take on board the concerns about the quality of the CSF as a result of the freeze/thaw cycle.
- Professor Michael, Dr Turner and Dr Wreghitt all broadly accepted the proposition of a relationship between viral load and immune response. In this sense, I use immune and inflammatory as meaning broadly the same. There were, it is true, differences in opinion about how precisely to express the relationship. I accept that the presence of protein on the cell surface plays a part in the immune response, but it seems to me that the preponderance of the evidence supports the proposition that there is a clear and direct (or near direct) relationship between viral load, immune response and ultimate outcome.
- In my judgment, the 1996 Wildemann paper does not undermine the expert opinion evidence of the degree of relationship between viral load and the immune response.
- The consequence of this is that, in my judgment, had acyclovir administration been commenced on Tuesday, the viral load would have been less. The acyclovir would have been targeting the replication process of fewer virions and the rate of increase of the virions would have been slowed. By Friday, the viral load was greater than it would have been on Tuesday. The acyclovir had to target the replication process of more virions and, whilst the rate of increase was still slowed, such process started from a higher base level than if it had begun on Tuesday.
- What of the deterioration in the Claimant's condition on 4 December 2018? Dr Turner thought that the Claimant's auto-inflammatory response was "extremely strong". He was of the opinion that the Claimant deteriorated "in very violent form" but, as recited in the summary of his evidence, he agreed there was nothing "explicit" in the literature which would help to indicate whether the timing of the deterioration was of itself unusual. That being so, it seems to me that experience is the best indicator. In that respect, it is Professor Michael who has undoubtedly the most real-life experience of how patients with HSE progress. He was not at all surprised by the fact of deterioration. I also accept his evidence, based upon his clinical experience, that the "likelihood of severity of that deterioration is best predicted by any delays in starting IV acyclovir". Thus I find that the Claimant would probably have deteriorated even if acyclovir had been started on Tuesday, but that the severity of such deterioration would have been less than in fact it was.
- I deal next whether the Claimant would have suffered a psychotic episode. Dr Turner thought that this would have occurred in any event. Professor Michael described in convincing detail what could be seen from the imaging. His view was that they showed insults from HSE "and nothing else". I reject any proposition that the Claimant was in some way pre-disposed to psychosis. In my judgment the medical history does not bear that out.
- The remaining issue is the critical one; what would have been the Claimant's outcome if acyclovir had started on Tuesday? I reject Dr Baker's view that any improvement in outcome would have been marginal. No other relevant expert expresses that view which, in any event, was expressed to be subject to the opinions of the neurologists.
- Reference to the various "outcome" scales provides some guide, but no expert was entirely comfortable with the use of what they described as linear scales with, in some cases, very broad descriptions which were not tailor made for viral encephalitis cases.
- Despite those reservations, the experts made some use of the various scales. In my judgment, the opinions of the Neurologists are of most use.
- In their Joint Statement, they agreed on the Claimant's condition at the time the Joint Statement was made. By reference to the Extended Glasgow Outcome Scale the Claimant was Grade 3 or Grade 4, that is lower to upper severe disability. Professor Michael used the numerical Grades. Dr Turner used the descriptors: "low to upper severe disability".
- By reference to the same scale, Professor Michael thought that with earlier treatment, the Claimant would have been Grade 6 to Grade 7, that is upper moderate disability to lower good recovery. Dr Turner's view did not alter from the view he expressed in the Joint Statement:
- Even allowing for the broadness of the descriptors, the position of Dr Turner seems to me to be untenable. Literally interpreted, it is a predicted worse outcome than has actually been achieved, since it makes no reference to "low to upper severe disability" (emphasis added). In fairness to Dr Turner, it will be recalled that in oral evidence he described the difference in outcome as being that the Claimant's memory would have been better. But that is all.
- Once more, I have to prefer the greater experience of Professor Michael. In my judgment, the Claimant would have been at Grade 6 or Grade 7 and would be independent for routine daily living. I accept that at present, although he is living with his family, he needs some assistance. He would continue to have headaches. He would be able to work in some capacity in IT but necessarily at a lesser level of capability than before and may have required adjustments to be made. Precisely what adjustment I cannot say on the evidence presented to me. This is consistent with the opinion of Dr Wreghitt, who thought that the Claimant would have been left with less severe neurological damage, although he could not specify which aspects of his neurological function would have been improved. I prefer this opinion to the opinion of Dr Baker whose refusal to accept, subject to the opinion of the neurologists, that any improvement would have been more than marginal undermined the value of his evidence.
- As to mental capacity, the Claimant would not have been able to manage family financial affairs. This is in accordance with the Joint Statement of the neurologists.
- Beyond this I do not consider it possible to go on the evidence presented before me.
- I offer my profound apologies to the parties for the length of time it has taken for me to complete this Judgment.
His Honour Judge Robinson:
Introduction
"A preliminary issue shall be tried between the Claimant and the Defendant as to whether or not the Defendant is liable to the Claimant by reason of the matters alleged in the Particulars of Claim, if so, whether or not any of the injuries described were so caused."
(1) On Tuesday 27 November 2018 the Defendant ought to have appreciated that the Claimant was suffering from a serious neurological illness which mandated urgent admission to hospital. Failure so to appreciate and act amounts to breach of duty of care by reference to the Bolam test.
(2) Had the Claimant been admitted to hospital on Tuesday it is probable that administration of acyclovir would have been commenced speedily.
(3) Because the Claimant was not admitted to hospital until Friday 30 November 2018, commencement of administration of acyclovir was delayed by about 55 hours.
(4) Commencement of acyclovir treatment on Tuesday would have resulted in a better outcome.
(1) There was no breach of duty on the part of the Defendant.
(2) It cannot be established that earlier commencement of administration of acyclovir would have made a difference.
The Lay Evidence
(1) Garbux, known as Gee. She is the elder sister of the Claimant.
(2) Gagun, sister and the Claimant's Litigation Friend.
(3) Gurdip, the Claimant's mother.
(4) Rupinder, the Claimant's wife.
The Expert Evidence
(1) Dr Jeremy Budd, General Practitioner (two reports).
(2) Professor Benedict Michael, Consultant Neurologist (two reports).
(3) Dr Kumar Das, Consultant Neuroradiologist.
(4) Dr Tim Wreghitt OBE, Consultant Clinical Scientist.
(1) Dr Kevin Barraclough, General Practitioner (two reports).
(2) Dr Alan Turner, Consultant Neurologist (two reports).
(3) Professor Alan Jackson, Professor of Radiology.
(4) Dr Robert Baker, Consultant Medical Microbiologist.
Overview and Assessment of the Claimant's Lay Witnesses
BREACH OF DUTY
(1) Fever.
(2) Headache(s).
(3) Cognitive impairment and/or confusion and/or personality or behavioural changes, sometimes referred to as delirium.
Claimant's Background
The Lay Evidence on behalf of the Claimant
Gee and Gurdip
"8. I walked into the guest room and found Sonny using his laptop. I could see he was unwell. He was hot to the touch and appeared feverish. My impression was that he was suffering from severe flu. He was perspiring and complained of a severe headache and told me that he had been unwell all day. He told me that he did not feel like eating and had been sick earlier.
10. Sonny mentioned that the light was irritating him yet paradoxically all the lights were on in the house. He also complained of a smell that I could not detect. No one had been cooking and there was nothing to account for what he was complaining of. He said to me 'I am scared' but he did not tell me what he was afraid of. That he should express fear of anything was completely out of character but I thought at the time his fear was of being left alone when unwell.
11. I had not seen Sonny this unwell before and I was concerned about the fever. He looked sick, pale and was perspiring. I also noted a different tone to his voice. I would describe it a bit like a flat monotone.
12. Apart from light and a smell that I could not detect, he also complained about hearing a noise that I could not hear. He described it as a high-pitched tone. It was his fever, combined with his overall condition, that concerned me enough to consider that an appointment should be made with his GP. Had he felt well enough, this is something he would have arranged for himself."
"2. I learned that Sonny was unwell on 27th November 2018 and I went to see him at my daughter Gurbux's [Gee's] home where he was staying at the time."
"4. As [Gee] was going to be at work the following day the 28th November, I made arrangements to stay with Sonny that day so I could look after him."
Rupinder
(1) She and the Claimant were living apart while the family home was undergoing extensive building works.
(2) The Claimant had suffered migraines for a number of years. These could be quite severe; he feels less inclined to talk; likes people to "keep the noise down" and asks to be left alone.
(3) She was kept informed of the Claimant's condition and went to see him on Thursday 29 November 2018. She says she "recognised that there was something different about this occasion". She noticed that he had a "vacant look and stared into space".
(4) She also noticed that he kept moving his fingers in an unusual way. When speaking with him she only got a limited response. She formed the view that he appeared disorientated.
Gagun
(1) She spoke by telephone with Gee on Monday 26 November 2018. Gee said the Claimant had returned from a yoga retreat on Sunday and was acting strangely and had been really upset. Gagun says this "was a concern as it was unlike Sonny."
(2) She was aware of the Claimant's history of recurring migraines "in the past".
(3) She arranged to be with the Claimant on Thursday 29 November 2018. The Claimant complained of smells that were making him feel sick, but Gagun could not smell anything. She confirmed in cross-examination that this was the first time she had seen the Claimant since his return on Sunday.
(4) The Claimant told Gagun that he "felt as if he had WhatsApp messages coming through his nose from his head". Gagun thought this was strange.
(5) She learned on Friday 30 November 2018 that the Claimant had been admitted to hospital.
"That's not quite correct. There were a couple of conversations that I'd had with my brother during the day that didn't quite make sense to me and were sort of red flags. So in answer to your question, there were a few odd things that struck me as out of character for my brother that day."
Events on Tuesday 27 November 2018
(1) He said he was unwell on Sunday.
(2) When Gee returned home on Monday, all the house lights were on. The Claimant mentioned this fact but said they were irritating him. Gee found this "inexplicable".
(3) The Claimant was in the guest room and appeared to have "severe flu". He was perspiring and was complaining of a "severe headache." He said he had been unwell all day.
(4) The Claimant "had been complaining of a smell and a sound" neither of which Gee could detect. She also thought he was "acting out of character in being simultaneously confused, uncertain and frightened."
(5) She thought the Claimant was "obviously unwell". His "temples were pounding and it appeared clear he had a fever."
(6) In answer to a question from the Defendant, Gee said she had not taken the Claimant's temperature, but that she felt he must have a temperature because he was "burning up" and that all of the windows in the house were open.
(7) Gee had never soothed the Claimant by pressing a wet flannel to the nape of his neck. She had given water and paracetamol to help reduce his temperature.
(8) The Claimant had not eaten all day, which was "not usual".
"35. Sonny was continuously fidgeting and making strange hand movements and touching his fingers together. I had never seen him do this before.
36. Both before the consultation and afterwards Sonny complained to me of dizziness, difficulty keeping his balance and his demeanour with me and Dr Ola was almost childlike. I told Dr Ola that I was worried about Sonny because I had never seen him in such a state before. I recall Doctor Ola endeavoured to allay my fears."
"Although I provided Dr Ola with information and the answer to some of his questions, it was Sonny himself who told Dr Ola that he had a pounding headache and he felt as though the ground was moving and the room was spinning. He told Dr Ola that he felt sick and that light irritated him."
"43. As Sonny stood up to leave, he paused holding the same position for a while, not moving as if unsure what to do next.
44. I had to prompt him to leave and when I did, he was slow to react. Sonny looked at me and Dr Ola and said 'the floor is moving' accompanied by hand gestures to describe what he was feeling. I remember looking at Dr Ola quizzically, he just looked at me and nodded. As we left, I asked my brother if he was OK, and he just repeated the floor was moving. "
"Specifically when I arrived home, my brother usually, when he has a headache, is irritable and he wants to be left alone and he usually sits in a fairly dark room. He doesn't like bright lights. But on this occasion the lights were on and that did not sit right with me and then he said 'Sis I'm scared'. Now he never says anything like that. This is a grown man. He's quite sure of himself, that rang alarm bells "
(1) These matters related to 2014 and 2015, a long time before 2018.
(2) Certain matters had only come to her attention after she had started speaking to the Claimant's circle of friends.
(3) In 2017 and 2018 the Claimant had started Yoga which "really put him in a good place." The Claimant was more energetic, positive and was moving on with things.
(4) So far as she was concerned, in the period before the consultation with the Defendant, she knew the Claimant "to always be in good health and someone who did make light of any illness".
In short, she rejected the proposition that her witness statement was "misleading and incomplete".
"Confusion could be the fact that he was disorientated, which I had mentioned, that the ground was moving, that he was scared. I had mentioned that he was scared. I'd also mentioned the smells and the noise that I couldn't detect. So all of this amounted to a full picture."
(1) Gee first spoke with call handler called Naz.
(2) Naz then spoke with a clinician. Gee had no input into that conversation.
(3) Gee then spoke with the Clinician, Dr Haque.
There was a later call to the ambulance service concerning the delay in arrival which I do not find to be instructive.
| 1 Naz | What's happening? |
| 2 Gee | Right so he had a fever on Monday, so all week he's had a fever. Tuesday we went to the GP to see Dr Ola. |
| 3 Naz | Just tell me what's happening today, if he needs help, that's why I need to know as soon as possible. |
| 4 GG | Right okay so today this is his fifth day he hasn't slept all night, he's been really delirious, he's having conversations that make no sense. |
| 5 Naz | So, he is unable to answer questions? |
| 6 Gee | Yeah. So he keeps looking at his right hand, I think he's probably having a either a, you know, a nervous breakdown, or |
| 7 Naz | Has this ever happened to him before? |
| 8 Gee | Never. First time I've seen him this way, so I'm really concerned now. |
| 9 Naz | So he's got a new confusion at the moment, yeah? |
| 10 Gee | Yeah. Last night |
| 11 Naz | Alright so what I'm going to do is run through an assessment with you |
| [Naz attempts to contact a clinician and reverts to Gee] | |
| 12 Naz | Gee, can I quickly ask you, I'm still trying to get through to a clinician at the moment but can I just ask you, when did this new confusion start? |
| 13 Gee | Erm, probably Wednesday, Thursday, yesterday more so, coz Wednesday I was at work. |
| 14 Naz | When did you notice he was, sort of, confused? Do you remember what |
| 15 Gee | Yesterday. |
| 16 Naz | Yesterday, you saw it you noticed, okay, stay on the line for me, I'm trying to get through to a clinician okay? |
"The new confusion firstly 'new confusion' is the word that she [Naz] used. If you can appreciate I hadn't slept for 24 hours, I was very stressed, new confusion was a word that was thrown at me. In my mind, I had already thought what does new confusion mean? So that was a word that was thrown at me. I was speaking about symptoms that were presenting on that morning and through the night. That's what new confusion means."
" she's asked me when did it start? I'm thinking well Wednesday I wasn't at home, so Thursday is when I recognized all of these new symptoms that I'm conveying to you now."
"On Tuesday was worse and stated hallucinations, floor was moving. He has become increasingly confused."
In answer to the proposition from Mr Porter that the Claimant's "confusion is worsening as the week goes on" she replied: "Exactly".
Defendant's Lay Evidence
(1) The Claimant presented with a few days' history of acute onset headaches, nausea, occasional vomiting and sensitivity to smells.
(2) He reported a fever and said he had not been able to go to work because he had been feeling unwell.
(3) Gee did most of the talking. The Claimant seemed rather withdrawn but "did answer all the questions I put to him".
(4) Gee emphasized that he had headaches, had been feeling nauseous with occasional vomiting, symptoms of fever and had not been himself lately.
(5) The Defendant took the Claimant's temperature, blood pressure, and blood oxygen saturation level, all of which were normal.
(6) The Defendant said he would have taken the Claimant's pulse reading but did not record it. He infers this is because "it will not have been concerning".
(7) Examination of the throat was normal.
(8) The Defendant's impression was that the Claimant "was suffering from the classic signs and symptoms of migraine, and he had presented in a similar way before, that is with a frontal headache, feeling sick, and possibly vomiting".
(9) The Claimant presented as being low in mood and was not really engaging much in conversation. The Defendant discussed a referral for Cognitive Behavioral Therapy (CBT). The Claimant agreed.
(10) The Defendant told Gee that if the symptoms got worse they should get back in touch with the surgery or go to the A&E department.
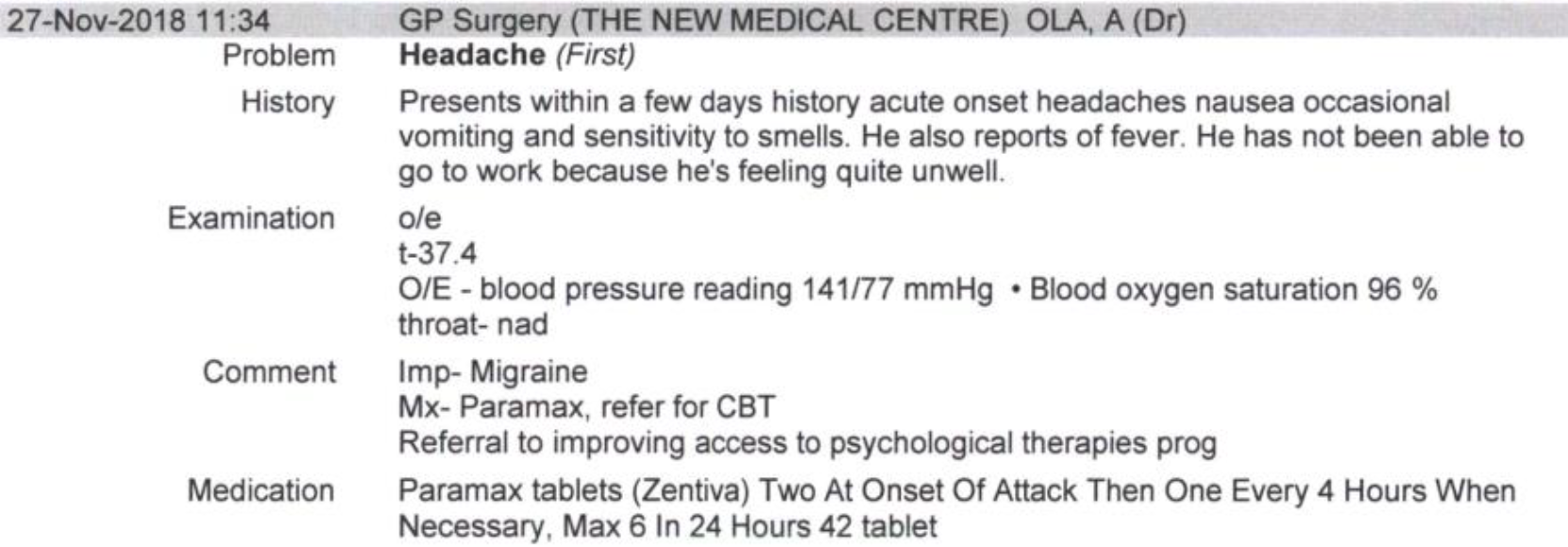
"I am certain that there were no obvious symptoms or signs of delirium or confusion during my consultation, nor were these reported to me by the claimant or his sister. There was no objective evidence of any fever."
(1) The extent of the Defendant's recollection of events outside the contents of the clinical notes;
(2) The quality of such clinical notes as the Defendant did make.
This is of course important when considering what actually happened during the consultation on 27 November 2018.
"When they came in and he sat down, there was this impression that he didn't want to be there. And he only spoke when I asked him a question, and he answered very curtly, very brief, brief, and his sister had to flesh it out, and then I'll go back to him, he would answer the question "yes" or "no", and he would answer and then the sister had to flesh it out."
I remember asking him about the nausea, for example - sorry, the vomiting, and he said, no, he hadn't vomited, and his sister said, "Actually you did, you did vomit yesterday", and he said, "Okay, yes, I did vomit yesterday". So that was the general atmosphere. He wasn't chatty, by any stretch of the imagination. His sister did - helped him out to answer in more detail based on her own observation."
"I do not recall him saying that he had a pounding headache, or that the ground was moving and the room spinning. Had he done so I would have recorded this in my notes".
"I remember... the headaches being described either by his sister... or by himself... as a pounding headache."
"What I meant was it wasn't mentioned to me in the consultation that he has a pounding headache. What I recollect is that headaches and I think, if I may just mention as well, this was a very, if I could use the word, chaotic consultation."
"I had numerous symptoms all coming, and trying to validate what sister says... And there was a sort of an underlay of him... not coming out of his room: why isn't he coming out of his room? Why is he not eating?... He's not mixing with the family. So all this was going on and... that's what I meant by the word "chaotic". In other words, there were a lot of things that were being discussed at the consultation but I do not recollect specific pounding headaches being mentioned in that context."
Findings arising from the Consultation
"Indeed, I suspect I would have called an ambulance as these could have been signs of delirium or an occult infection like a urinary tract infection."
The GP Experts
CAUSATION
Effect of Administration of Acyclovir
The Claimant's Progress Following Admission to Hospital
The Expert Evidence
Neurologists
15. On the balance of probabilities, with treatment with acyclovir starting on 27//11/18:
(a) Would the Claimant have made a complete recovery or would he have had some ongoing problems?
The neurologists agreed that "people who have had HSE never make a complete recovery".
(b) If he would have had ongoing problems:
(i) Please outline in the general terms the sort of problems he was likely to have had, and their likely functional impact on his life.
Professor Michael thought he would have continued to suffer headaches and have had cognitive problems for example being unable to manage the financial affairs of his family. Dr. Turner agreed with that and added that his memory would have been impaired, his sense of smell would have been poor or absent and he would have continued to have psychiatric problems and would have developed psychosis. On that latter issue, Professor Michael thought the development of psychosis was on the balance of probabilities a consequence of significant brain injury from HSE as opposed to a prior history of anxiety.
(ii) Would the Claimant's current condition be better than it is currently?
Professor Michael thought his condition would have been better than it is currently. Doctor Turner thought the Claimant would still have developed the disabling cognitive and psychiatric symptoms.
They both agreed that there is good evidence that there is a worse outcome after a 48 hour delay of acyclovir treatment.
(c) Would he have been independent, or would he have had some care requirements?
(d) If he would have had some care requirements, in general terms please set these out.
Professor Michael thought he would have been independent for routine daily living. Dr. Turner thought he would have needed reminding to take his medication and to maintain good daily human contact.
They agreed that the Claimant would need help with the more complex tasks for daily living such as managing family finances.
(e) Would he have been able to return to work whether in his pre- injury work as an IT consultant or in some [other] capacity?
Professor Michael thought he would have been able to return to work as an IT consultant in some capacity, perhaps with some adjustments made.
Dr. Turner thought work as an IT consultant would have been too complex for him to return to it.
(f) Would he have been able to continue to undertake routine domestic tasks at home?
There was agreement that he would have been able to undertake routine daily tasks at home. Dr. Turner observed that he does so now but needs reminding.
(g) Would he have retained the capacity to manage his own affairs?
There was agreement that it depends on the affairs in question. He would have been able to get on a bus and do the shopping but not manage family financial affairs.
" measuring a tiny amount of fluid from the lumbar spine is not an accurate representation of the amount of virus in the brain. Moreover, many of the studies which are referred to, because of the relative rarity of the disease, reflect samples that have been stored for some time in freezers, and frozen and thawed for various clinically indicated and research indicated tests. We know that freeze/thaw cycles and storage conditions, even the samples the CSF is stored in, reflect the ability to recover virus".
"Nevertheless, a recent review by two of the leading experts on the condition concludes that 'it is currently not possible at present to say that one can accurately predict the degree of ensuing disability from the number of days [sic] delay, especially when comparing, say, 3 days with 4 days'".
(1) His memory would have been better.
(2) His anosmia (loss of sense of smell) would not have been better.
(3) His tendency to headaches would not have been better.
(4) His ability to organize his life would not have been better.
(5) His movements would not have been better.
(1) The Claimant deteriorated "in a very violent form". It was "severe and became more severe".
(2) The Claimant's admission to the intensive care unit four days later was "not particularly unusual" but after discharge from the ICU he continued to deteriorate.
(3) The continued deterioration was due to the "violence of the inflammatory reaction which was taking place".
Radiologists
"No acute intracranial haemorrhage is seen. There is apparent low density change in the medial aspect of the right temporal lobe. This could be artifactual but a lesion here cannot entirely be excluded. There is no significant effacement of the lateral ventricles or midline shift. I would suggest an MRI scan for exclusion of any temporal lobe abnormality."
"I think that's an extraordinarily difficult question. I've said in my report that I think it is possible that there would have been changes two days previously. I think it is possible in that there are what I consider to be marked changes with the temporal lobe swelling by the time he got his CT scan done. And we do not have a literature on how quickly these changes develop. We know that they do develop quickly from watching them clinically, but we don't scan patients on a daily basis for herpes encephalopathy, so we don't have that data set to look at. So I think it's a difficult question and I think you can answer it in either way and provide some justification as Dr Das did. He thinks it was very early in the symptoms and that it was likely to be normal. I think by the time we saw it, it was pretty marked and therefore it was quite possible it would have been abnormal. But I've no scientific basis for that, that's just a feeling from clinical practice."
Virology
"On the balance of probabilities, how (if at all) would the Claimant's current condition differ if he had received acyclovir on 27/11/18 (rather than on 30/11/18)? In particular would it be:
a) better than it currently is?
b) the same as it currently is?"
Q. What we suggest is that [the Claimant] would probably have been within the 70 per cent of patients who have a good outcome. By that we mean an outcome retaining his independence if treated on the 27th rather than treated three days later on the 30th. It's apparent you reject that, but are you really saying those three days made no difference?
A. I am.
Q. Made no difference?
A. I said in my conclusion the likely benefits of earlier treatment would have been marginal, subject to the opinion of neurologists. Now neurologists are all agreed that there would have been some improvement, I put an argument why that would not necessarily be the case, but I use the word "marginal".
(1) "CSF obtained within the first 72 hours of symptoms may be negative by molecular detection, but become positive during the subsequent days despite administration of iv acyclovir." Dr Wreghitt in oral evidence explained that it may take some time for the virions to spread from cell to cell to move through brain tissue before appearing in the CSF.
(2) "Herpes virus remains detectable in CSF until at least seven days after the initiation of iv acyclovir." Dr Wreghitt thought it might be six days but also that it may be up to 10 days, consistent with "at least seven" days. As he put it, it depends on how much virus there is in the system and how much acyclovir is administered. The more virus there is at the start of treatment the longer it will take for the acyclovir to eliminate the vast majority of the virus.
(3) "Ten per cent of patients with herpes encephalitis will relapse if acyclovir is discontinued at 10 days." Dr Wreghitt agreed that some patients do relapse, but said that such patients may have started out with a higher viral load, or maybe not, but even if acyclovir treatment is continued, one would still have what he described as "residual virus". He made the point that viral DNA found in CSF by PCR testing would not necessarily be viable virus, but may be "virus floating around after the bomb has gone off in the cell".
(4) "It is recognised good practice to perform repeat CSF collection after about 10 days of iv acyclovir, because of (3), and if positive, treatment should be extended to 21 days." Dr Wreghitt agreed, but made the point that the more acyclovir you give and the earlier you give it, the more effective it will be.
(5) "Recurrent herpes meningitis and encephalitis are recognised syndromes." Dr Wreghitt agreed without reservation.
(1) A GCS of more than 10 indicates "early".
(2) Whether the patient has lost consciousness.
(3) Whether more than 5 days have elapsed before acyclovir treatment is commenced.
(4) Whether more than two days have elapsed between hospital admission and administration of acyclovir.
" avers that [it] is therefore difficult to argue that acyclovir delivered any earlier would have made much difference."
Dr Wreghitt said that he absolutely could not accept that proposition. In his opinion, if the Claimant had been treated with acyclovir three days earlier he could not believe he would not be "significantly neurologically better off" than he ended up being.
"Well that would be fine if everybody else in this court were not saying that there is a clear deterministic relationship between the presence of herpes simplex virus in terms of its copy numbers and the eventual - and the only study which has looked at this has not found it to be the case. Yes, it's small numbers, but it doesn't say what everybody else says should be the case."
" subject to the opinion of neurologists. Now neurologists are all agreed that there would have been some improvement. I put an argument why that would not necessarily be the case, but I use the word 'marginal'."
Conclusions and Findings
" the Claimant would now still be in the condition that he is not fully able to look after himself but can be left alone for more than 8 hours. On the Extended Glasgow Outcome Scale that would remain at 4" (upper sever disability).
Post Judgment Note
