Freely Available British and Irish Public Legal Information
[Home] [Databases] [World Law] [Multidatabase Search] [Help] [Feedback]
England and Wales High Court (King's Bench Division) Decisions
You are here: BAILII >> Databases >> England and Wales High Court (King's Bench Division) Decisions >> PXE v University Hospitals Birmingham NHS Foundation Trust [2024] EWHC 2023 (KB) (31 July 2024)
URL: http://www.bailii.org/ew/cases/EWHC/KB/2024/2023.html
Cite as: [2024] EWHC 2023 (KB)
[New search] [Printable PDF version] [Help]
KING'S BENCH DIVISION
Strand, London, WC2A 2LL |
||
B e f o r e :
sitting as a Judge of the High Court
____________________
| PXE (by his Mother and litigation friend DSD) |
Claimant |
|
- and |
||
| University Hospitals Birmingham NHS Foundation Trust |
Defendant |
____________________
Mr Richard Booth KC (instructed by Bevan Brittan LLP) for the Defendant
Hearing dates: 19-22 March 2024
____________________
Crown Copyright ©
- The Claimant, who is now 15 years old, was born at 00.54 on 4th October 2008. In these proceedings the Claimant sues by his mother and litigation friend, claiming damages for personal injuries prior to and around the time of his birth and alleged to have been caused by the negligent failure on the part of the Defendant's staff to (1) classify his mother's pregnancy as high risk, in light of her recorded history of "cystitis: kidney scarring" (2) to perform growth scans from 28 weeks and (3) to deliver him earlier so as to avoid injury.
- In the events that happened the Claimant suffered foetal growth restriction, which was not recognised and addressed prior to his delivery. The Claimant suffered periventricular leukomalacia ("PVL") and now has permanent brain damage. In a draft defence served as a letter of response to the letter of claim sent on 9 April 2020 it was accepted, in paragraph 30, that the Claimant probably sustained PVL damage because of chronic foetal hypoxia ischaemia, which occurred in the perinatal period. This position is repeated in the defence filed in these proceedings.
- There is an anonymity order in place and purely for ease of reference I shall refer to the Claimant and his mother as "the Claimant" and "the Claimant's Mother" respectively. No disrespect is meant to either of them by so doing and at this juncture I acknowledge, having observed the Claimant's Mother during the course of the trial before me, the very obvious effect on her of the events that were investigated in considerable detail at the trial before me. Whilst she was quiet and dignified during the trial, listening intently to the evidence, there were moments of obvious and spontaneous distress.
- The Defendant is an NHS trust which is vicariously liable for any negligence on the part of the obstetric and midwifery team who were responsible for treating the Claimant's mother at Solihull Hospital and in the community. At the time of the Claimant's birth both Solihull Hospital (which was described as a maternity unit) and Heartlands Hospital (where there was an obstetrics team) formed part of the Heart of England NHS Trust (the third hospital in the trust was the Good Hope Hospital). It employed, amongst others, midwives Karen Hickman and Vivienne Carbery and Ms Susan Hutchon and Mr Christopher Griffin, both of whom were consultant obstetricians. It was Mr Griffin who delivered the Claimant by emergency caesarean section on 4th October 2008.
- This is my judgment following the trial on the issue of liability only. The Claimant was represented by Ms Gumbel KC and the Defendant by Mr Booth KC. I am grateful to them both for their clearly structured and helpful skeleton arguments and bullet point and oral closing submissions together with their focussed approach throughout the trial, which enabled the court to cover a large amount of evidence in a relatively short period of time. There is a significant amount of documentary evidence in this case in addition to the oral evidence (both of fact and of opinion) that the court heard over the course of three sitting days. Expert opinion evidence has been provided in the following disciplines: midwifery, nephrology, obstetrics, foetal medicine and neonatal medicine. All but the neonatology experts attended the trial to give oral evidence. The fact that a particular piece of evidence or document or submission has not been referred to in this judgment does not mean that it has not been taken into account.
- It is sensible to set out at this juncture the allegations of breach of duty that were pursued at trial and which can be found in paragraphs 5.4(a) to (c) of the Particulars of Claim, namely that the Claimant's Mother was not properly risk assessed by midwifery staff at the time of booking and the failure to notify the maternal history of renal disease and refer to a consultant led obstetric care resulted in inadequate antenatal monitoring by:
- Factual causation is pleaded as follows in the second paragraph numbered 5.4 (it is put on the basis that the Claimant's injuries were caused or materially contributed to by the negligence of the Defendant):
- In her written opening Miss Gumbel KC identified the key issues for the court to decide and which arise from the allegations of breach of duty and causation as follows:
- The Claimant was the first baby that his mother gave birth to. The Claimant's mother, who was born in April 1973, was booked at home on 17 April 2008 in relation to her pregnancy with the Claimant. That booking (and all subsequent midwifery appointments other than in a hospital setting) was undertaken by community midwife Hickman. Some two weeks earlier on 3 April 2008, the Claimant's mother had attended the Early Pregnancy Assessment Centre having experienced lower abdominal cramps and bleeding. The referral letter from her GP dated 1 April 2008, which was written against this clinical background, expressed concern that "this is a threatened miscarriage" and asked for a review as to the viability of the pregnancy. A one-page printout of the Claimant's mother's medical history (seemingly printed off at 12:45 on 1 April 2008) was enclosed with the referral letter. It indicated, in relation to the headings "significant medical history" and "chronic disease register" that there was "no data recorded".
- A scan undertaken on 3 April 2008 indicated that the pregnancy was viable.
- At the booking-in appointment on 17 April 2008, in the section of the mother's handheld records that was dedicated to medical history, midwife Hickman ticked the box to indicate that there was a history of kidney or urinary problems. She recorded the details as "recurrent cystitis scarring on kidneys."
- The Claimant's mother was booked in for an ultrasound dating scan on 16 May 2008 and an antenatal care appointment with a midwife (midwife Carbery). The ultrasound scan assessed the gestation of the baby at 13 weeks and the estimated date of delivery was assessed at 20 November 2008. The Claimant's mother's BMI was recorded at 20. Midwife Carbery recorded in the "antenatal clinic-held summary" notes (under the heading "summary of relevant history"):
- The notes completed by midwife Carbery at the antenatal appointment on 16 May 2008 indicate in three places that the pregnancy was "low" risk and the management plan for the Claimant's mother was "midwife led care".
- On 20 May 2008 Ms Hutchon reviewed the classification of the pregnancy as "low risk" and initialled and dated the assessment of the antenatal risk as low to indicate her agreement with this assessment.
- On 12 June 2008 the Claimant's mother was reviewed by Midwife Hickman for an antenatal appointment who noted "all well". BP was recorded as 124/75. Urine was noted to be NAD (no abnormalities detected). There is a tick next to the foetal movements box to indicate they were discussed.
- On 17 July 2008 the Claimant's mother was reviewed by Midwife Hickman for an antenatal appointment who noted "for regular MSU in light of history. All well. MAT B1 given." BP was recorded as 112/72 and urine was not tested at this appointment. The boxes are ticked to indicate fetal movements were felt and discussed.
- On 28 August 2008 the Claimant's mother was reviewed by Midwife Hickman for an antenatal appointment who noted "Bloods for BTS, FBC & RBS taken". Fundal height measurement was noted as 27cms at 28 weeks. Urine was not tested and BP was recorded as 129/74. Presentation was noted to be "ceph".
- On 25 September 2008 the Claimant's mother was reviewed by Midwife Hickman for an antenatal appointment who noted "all well". BP was recorded as 108/87. Urine NAD. The boxes are ticked to indicate fetal movements were felt and discussed. Presentation was noted to be "ceph". Fundal height measurement was noted to be 30cms.
- At 20:20 on 3 October 2008 the Claimant's mother attended Solihull Hospital and reported that fetal movements were reduced for 4 days and that she had felt: "no movements last night which is unusual, none today. No pain or visual disturbance, feels well". The Claimant's mother's blood pressure was measured as 158/98. At 20:50 a CTG recording of the Claimant's heart was recorded as pathological, there was no variability, decelerations x 1 unprovoked, no accelerations. At 21:00 the Claimant's mother was seen by Dr Raj. He noted that the Claimant's mother's cervix was closed. He noted: "For C section, gown, Consent, NNU informed." The consent form noted the procedure as caesarean section, the benefits as "delivery" and the risks as: "Infection, Haemorrhage, Thrombosis".
- Prior to transfer to Heartlands Hospital, the Solihull Hospital records indicate:
- The notes then indicate:
- The Claimant's mother was transferred to Birmingham Heartlands hospital and the Claimant was delivered by Mr Griffin at 00:54 on 4 October 2008. His condition is described in the neonatal admission summary notes, which indicate that he had the following problems:
- Prematurity
- Respiratory distress syndrome
- Neonatal hypoglycaemia
- Thrombocytopaenia
- Intrauterine growth retardation
- Staph Epidermidis sepsis/septicaemia
- Jaundice
- The Claimant remained in hospital until 6 November 2008, when he was discharged home.
- On 10 March 2009 the Claimant's parents held a meeting with Mr Griffin. Following that meeting he wrote a letter to the Claimant's parents of the same date. In it he stated:
- A letter of claim with draft particulars of claim attached setting out the letter from Mr Griffin was sent on 9 April 2020. On 1 March 2021 the Defendant responded and denied liability. The claim form was sealed on 12 January 2022 and it was served, together with the particulars of claim, on 26 January 2022. A defence denying liability was served on 19 April 2022. Directions were given on 20 July 2022, expert evidence exchanged on 4 August 2023 and the trial on liability took place between 19 and 22 March 2024.
- The burden of proving negligence lies on the Claimant to the civil standard (i.e. the balance of probabilities). The applicable legal framework is not contentious. The starting point is the well-known case of Bolam v Friern Hospital Management Committee [1957] 1 WLR 582 where it was held that:
- This test applies to both the midwives and the Doctors employed by the Defendant.
- In terms of application of this case to the level of seniority of a doctor or midwife the Court of Appeal clarified in the case of: FB v Princess Alexander Hospital NHS Trust [2017] EWCA Civ 334,
- The Bolam test was expanded by the test in the case of Bolitho v City and Hackney HA [1998] AC 232 at page 241:
- In her closing submissions Ms Gumbel KC submitted that the particular difficulty for the Claimant in the present case is to show what would have happened if Ms Hutchon (the Defendant's consultant) had taken into account the kidney scarring (it being alleged that she did not properly take this into account or investigate its significance). What she would have done if she had acted competently in taking into account the kidney scarring is a matter of hypothesis. In this respect the analysis of the Court of Appeal in the case of Keefe v Isle of Man Steam Packet Co Ltd. [2010] EWCA Civ 683 at paragraph 19 is relevant:.
- Mr Booth KC also drew my attention to the cases of Maynard v West Midlands RHA [1985] 1 All ER 635 and Hooper v Young [1998] Lloyd's Rep Med 61 when considering the applicable principles.
- He submitted (and I do not take it that this is in any way contentious) that when one looks at the authorities the test to be applied, mutatis mutandis, as to whether there was any negligence by the Defendant's treating midwives or doctors is by the standard of the ordinary skilled midwife or obstetrician respectively at the relevant time before 1st October 2008, exercising and professing to have the special skill of a midwife or obstetrician respectively. Only if the midwives or doctors employed by the Defendant failed to measure up to that standard can they be said to have been negligent. The measure can also be expressed by asking whether the actions of the midwives or doctors were such as a reasonably competent midwife or obstetrician (respectively) exercising appropriate skill and care could have taken. Briefly, was the relevant action within the bracket of acceptable treatment? In this regard a wrong decision by such a clinical practitioner is neither here nor there.
- Furthermore, genuine differences of opinion and technique between midwives/doctors exist and the fact that the Defendant's midwives/doctors took one as opposed to any other of such opinions or techniques does not prove negligence. I add (and this was not part of Mr Booth KC's submissions but is clearly the case in light of the Bolitho gloss as it is sometimes referred to) that expert evidence relied upon by a defendant to establish a genuine difference of opinion and technique must have a logical basis and reach a defensible conclusion when considering the question of comparative risks and benefits. If it does the court will be satisfied that such evidence represents a standard of practice recognised as proper by a competent reasonable body of opinion and the Claimant will be unable to establish breach of duty. The role of the court when undertaking this evaluation of expert evidence is most definitely not to prefer one tenable clinical view as opposed to another and use this as a basis for a finding of negligence.
- On behalf of the Claimant I heard from the Claimant's mother, maternal grandmother and Mr Griffin. On behalf of the Defendant I heard from Mrs Hickman (who retired in 2019), Ms Carbery and Ms Hutchon (who stopped working in antenatal clinics in 2014 and retired in 2018). My clear impression of each of these witnesses was that they were doing their best to assist the court, albeit about events that happened almost 16 years ago (or in the case of the Claimant's mother's pre-pregnancy medical history considerably longer than 16 years ago).
- The Claimant's mother was clearly an intelligent and articulate woman. Prior to the birth of the Claimant she was employed as a nanny for two privately working plastic surgeons and she remains employed by them, albeit in a different capacity. Under cross examination the Claimant's mother said that whilst she still does not know whether she has chronic kidney disease ("CKD") "I know definitely that one of my kidneys was scarred, so I don't know how you would class that." She thought that she was told this when she was around 16 or 17 (at which time she also had a scan) and also said that when she was a lot younger she was "referred to Corbett Hospital where I had a number of scans." At this juncture I note that unfortunately the medical records relating to the Claimant's mother's childhood have either been lost or destroyed. Either way these were not available to the court.
- The Claimant's Mother was taken to her medical records which indicated that in 1994 when she spent a few days in hospital over her 21st birthday for treatment for food poisoning she underwent an intravenous pyelogram ("IVP") of her kidneys, which was reported as normal (save that the lower pole of the right kidney was obscured by abdominal gas) and following discharge from hospital she underwent an ultrasound scan of her right kidney. At the time the Claimant's mother gave evidence the results of these scans were not available to the court but there was a letter dated 5th May 1994 addressed to her GP explaining that an ultrasound scan had been arranged. That letter is annotated with a manuscript note that stated "IVP & Scan kidneys. NAD". The Claimant's mother had no recollection of the IVP or subsequent ultrasound scan being undertaken or of being told the outcome of these investigations (although she fairly accepted that she would have been reassured by these results).
- Likewise, the Claimant's mother had no recollection of a later abdominal ultrasound scan carried out in 1996.
- At a later stage in the trial the Claimant's solicitors were able to provide the reports prepared after the IVP and ultrasound scans were undertaken in 1994 and the further abdominal ultrasound scan was carried out in 1996. These documents confirmed that no abnormalities were detected in the Claimant's mother's kidneys in 1994 or 1996. However, these documents were not included in the Claimant's mother's GP notes that were disclosed for the purposes of the trial.
- In cross examination the Claimant's maternal grandmother agreed that her daughter had never told her that she has CKD. She recalled taking her daughter to have a scan at the Corbett Hospital when she was about 5 or 6 and the evidence in her witness statement (which was not challenged) was that her daughter's history of childhood cystitis began when she was 5 years old and she had an infection that involved blood in her urine. This was followed by "repeated episodes of cystitis during her childhood and teenage years and upwards."
- Mr Griffin gave evidence via a video link from Australia. In his witness statement he stated that he remembered the events surrounding the Claimant's mother's pregnancy and that the letter that he wrote to the Claimant's parents accurately reflected his opinions at the time. He said this in his witness statement:
- Under cross examination Mr Griffin accepted that in 2008 there were only about 50 to 100 consultant obstetricians in the UK with significant experience and skill in performing ultrasound scans. He was one of them. He also accepted that in 2008 he had a lower threshold for performing foetal growth ultrasound scans than a number, but not all, of his consultant colleagues.
- Following the Claimant's birth, and notwithstanding his concerns (as set out in his letter and witness statement), Mr Griffin did not himself fill out an incident report, although in fairness to him he also said in evidence that at the time incident forms were usually filled in by more junior members of staff and he believed that cases such as the present one were automatically reviewed by a clinical risk group (although he could neither affirm or deny whether that actually happened in the present case).
- In evidence Mrs Hickman accepted that she had no individual recollection of the Claimant's mother and her evidence amounted to an attempt to reconstruct her thinking at the time when she completed the relevant medical notes. Mrs Hickman cannot be criticised for this given the passage of time.
- Under cross examination Mrs Hickman said that when she wrote down "recurrent cystitis: kidney scarring" she would have written down "exactly what the mother told me". This would have prompted enquiries about whether the mother was under the care of a consultant or had had any recent issues and if the answer was no "my thought would be that it was not necessary to highlight it for an urgent review and I put her down for a routine appointment". She herself did not write "low risk" or assign any level of risk (although I note that the routine appointment was in a midwife led clinic). Mrs Hickman described a three-stage process, with her dealing with the booking in, then a review by a midwife and finally a review by a consultant. We know that in the present case the midwife review was undertaken by midwife Carbery and the reviewing consultant was Ms Hutchon.
- Midwife Carbery gave evidence that at the appointment on 16 May 2008 (which was the one and only time that she saw the Claimant's mother) she would have had access to a letter into the hospital assigning the lady to clinic (this has not been disclosed but logically must have had some input from midwife Hickman) together with the mother's hand held notes. At her appointment with the Claimant's mother midwife Carbery went through the mother's medical history again (together with taking blood pressure and sending off a midstream urine sample). Midwife Carbery accepted that at this clinic it was her judgment about whether to designate the pregnancy as low risk or not and that, knowing the Claimant's mother had reported a history of cystitis and kidney scarring:
- Midwife Carbery was not sure for definite whether she would have known in 2008 that there was a risk that any pre-existing kidney disease could get worse in pregnancy and presented a risk of IUGR or pre-eclampsia. She gave evidence that she probably made a clinical judgment that the Claimant's mother was at low risk of chronic kidney failure, relying on the fact that the Claimant's mother wasn't under a renal consultant, "hadn't really had any symptoms except once or twice in her adult life" and that there was no sort of regular medication or GP reviews. Her evidence about what she would have been told by the Claimant's mother about the number of adult infections with cystitis ("once or twice") was unconvincing and based on an assumption that "if I had had any information that highlighted an issue, I would have made a consultant referral" and therefore would have explored how many episodes of cystitis the mother had had as an adult. I note that midwife Carbery had no recollection of her appointment with the Claimant's mother, had made no notes of the follow up questions to the mother or her answers and did not even give an indication of the threshold for adult cystitis infections that would by themselves merit a referral to a consultant led clinic.
- I also note that in her oral evidence the Claimant's mother said under cross examination that if she was asked to estimate how many times she had seen her GP about cystitis in the last 20 years she would probably think "one, two times". Midwife Carbery was in court to hear the Claimant's mother give this evidence. It is in my view likely that the aspect of Midwife Carbery's evidence that the Claimant's mother "hadn't really had any symptoms except once or twice in her adult life" was a case of midwife Carbery repeating (most probably inadvertently, because she did say that she thought she had read it somewhere) evidence that she had heard the Claimant's mother give earlier the same day in court. That evidence was itself inaccurate when one looks at the Claimant's mother's medical records (although for the sake of completeness I will state at this juncture that nothing material to the present case turns on the number of incidents in adulthood that the Claimant's mother suffered from cystitis).
- Midwife Carbery's evidence also suggested (without any recollection or documentary evidence to suggest she did) that she might have discussed the Claimant's mother's case with Ms Hutchon. There is no evidence to support this assertion and it is just as likely that she did not.
- That said, I do accept that it is more likely than not that midwife Carbery would have asked the Claimant's mother whether she was under a renal consultant, was under GP reviews or was taking medication. That was consistent with the evidence of Mrs Hickman about the enquiries she would have made (and indeed is consistent with the evidence given by Ms Hutchon about the approach she adopted when assessing the risk of the pregnancy).
- Ms Hutchon (who is now retired and has not been in clinical practice for a while) also gave evidence to the court. She was a reflective witness who was at pains to try and put herself in the position she was in in 2008 (with the knowledge she had as at that date, acknowledging as she did that "I don't think that what I knew in 2008 is what I know now").
- Ms Hutchon's evidence was that she undertook an independent assessment of the Claimant's mother's pregnancy and any risks associated with it. I do note that she also gave evidence that "midwives are generally experienced enough to recognise when expectant mothers require Consultant led care", however there was nothing in her evidence to suggest that the assessment that she undertook was a "rubber stamping" exercise. Ms Hutchon said that her assessment that the pregnancy was low risk was based on the information recorded by midwife Carbery (including "cystitis: kidney scarring") but that she would also have had access to "other notes available at the time" which included the admission for threatened miscarriage. She also said that if she had not been happy with the amount of information she had she would have looked at surrogate information "so that would be things that would be available on the Trust intranet, previous admissions. I think the miscarriage notes would have been there, the GP's letters all GP's letters to other specialists, any old MSU results."
- In response to questions put by Mr Booth KC in re-examination Ms Hutchon stated that she believed that she would have had sight of the microbiology results of the Claimant's mother's MSU taken on 16 May 2008 (by midwife Carbery) and reported on 19 May 2008 when assessing the care pathway for the Claimant's mother's pregnancy on 20 May 2008.
- When asked whether she thought at the time that a history of cystitis and kidney scarring was of any relevance to the pregnancy Miss Hutchon said yes, it meant "increasing a risk of urinary tract infections during the [pregnancy]" but that at the time she didn't think that there was an increased risk of having a baby with IUGR or a risk of pre-eclampsia. She also acknowledged that seeing a note that the Claimant's mother had "cystitis: kidney scarring" was worrying enough to cause her to want to explore the matter further (by looking at what she described as the surrogate information as set out above).
- Ms Hutchon also gave evidence that one of the possibilities from a history of cystitis and renal scarring was that the mother had reflux nephropathy but went on to say that it is very common for women to have recurrent cystitis from their late teens and that:
- Later on in her evidence Ms Hutchon said this:
- Ms Hutchon also acknowledged, in response to a question from the court, that at the time of the Claimant's mother's pregnancy she was not aware of the connection between reflux nephropathy and IUGR in the absence of functional kidney abnormality.
- In both her witness statement and in live evidence Ms Hutchon dealt with what would have happened if the Claimant's mother had been assessed as high risk at the clinic on 16 May 2008. In her witness statement she said she would most likely have seen the mother in clinic late May/early June and she said this:
- In her oral evidence Ms Hutchon suggested for the first time that if the Claimant's mother had been referred to her and she had had any concerns about the history of kidney scarring, she would have been more likely to try to arrange a kidney scan than a fetal growth scan. She suggested that this might have been done at the same time as the 20-week scan if the sonographer was happy to assess the kidney.
- Ms Hutchon also gave evidence that "the division between high risk and low risk is really about a prescription for your antenatal care. It's not it's not a predictor of what will happen so by agreeing to "low" in the antenatal notes, you're really agreeing to what was the standard ante-natal care package, and that is repeated tests throughout the pregnancy to detect growth restriction, and in particular to detect pre-eclampsia" and that if she had felt that the Claimant's mother needed ultrasound scans "It's inconceivable I wouldn't have booked antenatal scans, growth scans, if I felt that they were indicated."
- She accepted that growth scans would have been more accurate in picking up that the Claimant was suffering from IUGR and that if the mother had been scanned at 28 weeks the IUGR would have been picked up and the management of the pregnancy would have been different, although she expressed some doubt about whether a growth scan would have been first done at 28 weeks or at a later juncture in the pregnancy, and was unclear in her recollection whether in 2008 growth scans would have been done at 28 and 34 weeks or 32 and 34 weeks, commenting that "it wasn't universally available for us to do 28 and 32 week scans." She suggested that it would have been easier for Mr Griffin to do 28 and 32 week scans because he was in a position to do the scans himself, noting that her requests for scans could be declined by the sonographers if they felt that the request did not accord with current guidance.
- Ms Hutchon was taken in her evidence and in re-examination to the literature that was available in 2008. She thought that she might have had a copy of the Handbook of Obstetric Medicine, 3rd edition (2006) by Nelson-Piercy at home. She was aware of the work being undertaken in the West Midlands by Professor Jason Gardosi and his team in relation to foetal growth screening by fundal height measurement, and had in fact attended one of Professor Gardosi's lectures.
- The claimant relied on a number of pieces of medical literature including a paper presented in 2009 by Professor Gardosi and others in the journal "Best Practice and Research Clinical Obstetrics and Gynaecology". The authors commenced the paper with the following statement:
- The paper went on to consider when to measure and who to measure. The answer to the former question was, in the view of the authors, that fundal height measurement should commence at 26 to 28 weeks and no more frequently than fortnightly (to avoid the increment in foetal growth being smaller than the measurement error). The answer to the question of who to measure included those pregnancies considered high risk, and the paper states that table two incorporated therein listed the more common clinical conditions "currently considered to be an indication for serial ultrasound." That table consists of part A and Part B. Part B identifies indications for increased risk of fetal growth restriction which would justify serial ultrasound biometry. Those risks include "renal conditions" (stated to be less than 1% of cases). The paper noted that it was estimated that about 20 to 25% "of our maternity population have one or more indications for 3rd trimester surveillance by ultrasound".
- The authors went on to comment that:
- In her oral evidence Ms Hutchon intimated that as this paper was published in 2009, it is likely that it informed later revisions of the Trust guidelines. She also said that she recognised the lack of availability of scanning resources referred to in the paper and that at about the time of the paper community midwifery scanning was introduced. I do however note that the paper referred to the fact that antenatal restriction of fetal growth restriction had been adopted by health service commissioners as a key quality indicator in the West Midlands prior to the paper being published. One would expect Trust guidelines to be kept in synch with key quality indicators, although what is not clear is when in 2009 the paper was published and how "recently" the key quality indicator had been adopted as at the date of publication of the paper.
- Evidence was provided by Ms Angela Helleur for the Claimant and Ms Jennifer Fraser for the Defendant.
- Ms Helleur was recently appointed as the Site Chief Executive at the Princess Royal University Hospital on South Sites, Kings College Hospital NHS Foundation Trust where she is responsible for the delivery of all services including maternity for the acute hospitals. Past appointments include chief nurse and executive director of midwifery for the South East London integrated care board, chief nurse and executive director of midwifery for the Lewisham and Greenwich NHS trust and deputy director for the medical directorate of NHS London. She is an experienced midwife educated to Masters level and until her most recent appointment maintained a clinical practice in addition to her management responsibilities. She has over 20 years' experience as an expert witness.
- In her written report dated June 2023 Ms Helleur expressed the following opinion:
- This was a view that Ms Helleur maintained at the joint meeting of the midwifery experts. The note of the meeting records Ms Helleur's view that:
- Under cross examination by Mr Booth KC Ms Helleur was asked:
- Later she said this:
- It was put to her that:
- Ms Fraser, the defendant's midwifery expert, qualified as a midwife in 1975 and retired from clinical practice at the end of 2012, coming off the Nursing and Midwifery Council Register in 2014. She was the lead midwife for clinical governance in obstetrics, paediatrics, sexual health and gynaecology until June 2011 at the Norfolk and Norwich hospital. She is educated to Masters degree level and when practising acted as a supervisor for midwives as well as also frequently lecturing and publishing articles.
- In her written expert's report Ms Fraser said this:
- The expert also opined that when midwife Carbery saw the Claimant's Mother on 16 May 2008 "she says that she did not record [the claimant's mother] taking any medication, receiving any other treatment or being under the review of a doctor for her cystitis and scarring or she would, as per usual practice, have recorded this. It was after these two midwifery appointments that Ms Hutchon perused the records on 20 May 2008. A consultant opinion may have been helpful but it was not mandatory. But in any event a consultant overview did take place."
- In the joint statement prepared following the meeting of the midwifery experts Ms Fraser opined that there was no evidence of chronic disease on 17 April or 20 May 2008 (the latter date should be 16 May 2008, which is the date that the mother saw midwife Carbery as opposed to the date that the notes were reviewed by Ms Hutchon) and that it was reasonable to classify the Claimant's Mother's pregnancy as low risk.
- When asked under cross examination why she thought it would have been helpful for the Claimant's Mother to be seen by a consultant if it was clear cut that she could simply be assessed as low risk her answer was as follows:
- This was an unconvincing response. If one took the statement that "any face to face discussion could be helpful", against an assertion that the pregnancy in question was low risk, there would logically be an appointment between expectant mother and consultant in every case. No obstetrics system could cope with that and nor would it be a sensible use of resources or a proper balance of risk against benefit.
- The Claimant called evidence from Dr Peter DuPont. He was appointed consultant nephrologist and UCL honorary associate professor at the Royal Free Hospital, London in 2006. He has more than 30 years' experience in all aspects of renal medicine including general nephrology, chronic kidney disease, hypertension, dialysis and renal transplantation. He has been engaged in medico legal practice since 2008 with the bulk of his work being undertaken for claimants. He thought when asked about this that this had something to do with fee structures.
- In his oral evidence to the court Dr DuPont explained that reflux nephropathy is a disease that develops congenitally. Within the body there is a collecting system known as the renal pelvis, which collects urine. There are two tubes one on each side that drain down from the collecting system of the kidney to the bladder and then the bladder empties to the outside in the usual fashion. There is a valve mechanism situated on each kidney where the urinary tube joins the bladder. The purpose of the valves is to prevent reflux back up to one or both kidneys when the bladder is squeezed. It is thought that reflux nephropathy is caused by a fault in one or both valves. If a young child has a lower urinary tract infection (such as cystitis) and a faulty valve, instead of preventing reflux the valve allows infected urine back up towards the kidney. The developing kidney in a young child is then susceptible to scarring. This is known as a reflux nephropathy. It is not a disease that develops de novo in adults. It is thought that for most patients the reflux stops at about the age of five years, but by that stage the damage is done. Once a scar is established on a kidney it is there for life and it is not reversible. Patients who develop reflux nephropathy in childhood can present in adulthood with hypertension or impaired kidney function.
- The significance of reflux nephropathy in an expectant mother is that pregnancy is "a stress test for the kidneys, your glomerular filtration rate goes up by about 50% during pregnancy, so something that wasn't a problem prior to pregnancy may be revealed by pregnancy. So quite a number of women with either known or not known history of reflux nephropathy may run into difficulties in pregnancy and they're picked up for the first time in pregnancy."
- Dr DuPont was of the view that the evidence from the maternal grandmother was consistent with what he had described. He said that urinary tract infections in children are relatively uncommon (as opposed to in adult life when they are extremely common).
- When asked whether if a woman has had urinary tract infections in childhood and had scarring in the kidney there was any relationship with the number of infections that she had in adulthood or that changed matters in any way he said this:
- His evidence was that scarring of the kidneys has a relatively short list of causes and in a woman of the Claimant's Mother's age with her history of childhood infection the likeliest cause of kidney scarring would be reflux nephropathy in childhood.
- One of the central planks of the Defendant's case on causation is that there is no evidence that the Claimant's mother does have a scarred kidney and as such suffer from chronic kidney disease; as such the Defendant argues (amongst other matters) that the Claimant's case is that his mother ought to have been placed on the high risk care pathway and then undergone fetal growth scans because of a risk of a condition that she might not have.
- In this context under cross examination Dr DuPont accepted that even as at the date of the trial (almost 16 years after the index events) there is no objective evidence on the scans undertaken to date that the Claimant's mother is suffering from chronic kidney disease; he accepted that the IVP and renal ultrasound done in 1994 were reported as normal but maintained that unless and until a DMSA imaging is undertaken one cannot rule out that the Claimant's mother has a scarred kidney. Such a test could not have been undertaken during pregnancy due to the radiation risk and has not (for reasons that have not been clearly elucidated to the court) been undertaken in the intervening period since the Claimant's birth, notwithstanding the fact that in his initial expert report provided in 2021 Dr Dupont recommended that a DMSA scan be undertaken.
- Dr Dupont also accepted under cross examination that the normal IVP and normal ultrasound scans that have been undertaken "make it unlikely on the balance of probabilities" that the Claimant's mother does have clinically significant kidney scarring but that "even if you felt that the risk was less than 50 per cent that she did have kidney scarring, going into pregnancy I'm not sure that would be enough to hang your hat on and say this is a low risk pregnancy, which is sort of the question that was posed." He went on to say:
- He also said that it is likely that the Claimant's mother's case would have been obstetric-led care and deferred to the obstetricians to define what that would have looked like.
- In the course of his cross examination Dr DuPont accepted that in his expert report he had veered into areas that were not within his own expertise (midwifery and to some extent obstetrics, although he justified his opinion that Dr Hutchon did not have enough evidence to categorise the Claimant's Mother's pregnancy as "low risk" on the basis that "for me it seems self evident"). Dr DuPont also accepted that he had outlined sections of a medical paper that he sought to rely on, a review article on reflux nephropathy and hypertension from the Journal of Human Hypertension (1998) in red (and in one place underlined some of the paper in red) and had not provided the entire paper.
- Dr Peter Andrews was the Defendant's expert nephrologist. He is a consultant nephrologist, former clinical director of the South West Thames Renal and Transplantation Unit who has produced more than 300 reports over a 20 year period, about 60% for claimants and 40% for defendants.
- In his written report Dr Andrews very much concentrated on addressing the issue of whether the Claimant's Mother has chronic kidney disease. He said the following:
- He went on to say in his written report that:
- Under cross examination he said this:
- Dr Andrews accepted that the history of kidney scarring and cystitis as a child was consistent with the possibility of reflux nephropathy and went on to say that it was something that should have been considered by the obstetrician in the context of the presentation of the patient. The following extract from his cross examination is of particular relevance:
- The claimant relied on a report from Mr Mark Denbow, who is an obstetric and fetal medicine expert. The Defendant relied upon obstetric evidence from Mr Derek Tuffnell and fetal medicine evidence from Dr Colette Sparey.
- Mr Denbow is a consultant in fetal medicine at University Hospital of Wales and a consultant in fetal medicine and obstetrics at St. Michael's Hospital, Bristol. This is a large teaching hospital. He accepted that his expertise in fetal medicine meant that his knowledge base in relation to fetal maternal medicine was significantly greater than that of a consultant obstetrician.
- Mr Denbow readily accepted that Mr Tuffnell represented a responsible body of obstetric opinion, commenting that "I've known Derek for many, many years and he has an established reputation as a leading voice in obstetrics" and that the same was true for Dr Colette Sparey in her field of fetal and maternal medicine.
- In his written report Mr Denbow explained that fetal growth restriction "reflects placental insufficiency, where the placenta is functioning sub-optimally in its role to supply oxygen and nutrients, the fetus fails to maintain adequate growth in utero, and is unable to reach its biological growth potential." Placental dysfunction can be subdivided broadly into three phases; preclinical, clinical and deterioration. Pre-eclampsia ("PET") and otherwise idiopathic fetal growth restriction "are part of the same disease spectrum and both relate to a problem of placentation and consequent placental ischaemia. PET can be thought of as a two-stage disorder. The first stage is abnormal perfusion of the placenta. The second is the maternal syndrome."
- Mr Denbow also opined in his written report that "the annotation in the notes (the significance of which appears not to have been noted by the midwifery team) 'cystitis: kidney scarring' is highly suggestive of reflux nephropathy." He then referred to the Handbook of obstetric medicine, 5th edition by Professor Catherine Nelson-Piercy and in particular the chapter on renal disease (which I deal with in greater detail in the section below dealing with the contemporaneous medical literature) which he maintained was authority for the proposition that women with reflux nephropathy and normal renal function and without hypertension pre-pregnancy had a 33% increased risk of hypertension and 15% increased risk of PET in pregnancy and that "there is a particular association between reflux nephropathy in the mother and FGR".
- Mr Denbow's expert opinion is that:
- His evidence was that it would not have been unreasonable to scan for fetal growth at 28 and 36 weeks, and if this had happened the 28-week scan would most likely have shown evidence of FGR and an ultrasound at 32 weeks would certainly have evidenced FGR. This was a view shared by Dr Sparey in paragraph 40(d) and (m) of her written report dated July 2023 and at the meeting of experts Mr Denbow and Dr Sparey agreed that on the balance of probabilities if a scan had been undertaken at 28 weeks the fetus would have been small for gestational age and the Claimant's Mother would have been advised to have further growth scans (at fortnightly or 2-3 week intervals) and weekly Dopplers. Dr Sparey was of the view that since the Claimant's Mother reported reduced fetal movements for four days prior to the day of birth it is highly likely that the decision to deliver the Claimant would have been made during these few days due to changes in fetal dopplers and/or an abnormal CTG or BPP and the baby would have been delivered a day or so before 3rd October 2008. Mr Denbow was of the view that the precise time at which the threshold to deliver would have been reached is unknown, however it is likely that there would have been evidence of significant fetal compromise (worsening fetal Dopplers or CTG changes) in the few days prior to 3rd October 2008, most likely corresponding to the four day history of reduced fetal movements.
- Mr Denbow was very clear in his oral evidence in chief that the key point in the Claimant's mother's pregnancy notes was the reference to cystitis and kidney scarring. He said this:
- Under cross examination it was put to Mr Denbow that he would not be critical of a consultant obstetrician in a district general hospital in 2008 not being aware of any association between reflux nephropathy and IUGR. His initial response was to say "I think I would be critical" but he then qualified this by saying that there was plenty of evidence which indicated that in 2008 it was known that renal conditions in general (as opposed to reflux nephropathy specifically) were associated with growth issues in pregnancy (something that Ms Hutchon indicated in her evidence she was aware of) and that:
- Mr Denbow also said under cross examination that in May 2008 there would have been a range of obstetric opinion about whether the Claimant's Mother was categorised as high risk or low risk. He commented that the joint meeting that he has held with Mr Tuffnell and Dr Sparey brought home to him that there were regional variations but went on to say that given the work that was being done in the West Midlands in 2008 by Professor Gardosi and his team he would have expected any regional variation in the West Midlands to have indicated that in that area growth scans would have been performed in 2008 if it was thought that the Claimant was at risk of intrauterine growth restriction.
- Under cross examination Mr Denbow stated that he was of the view that Ms Hutchon should have seen the Claimant's Mother at a face to face consultation. This evidence was slightly different to evidence given by Mr Denbow in chief, when he said that Ms Hutchon's dismissal of the Claimant's Mother's medical history was a concern and that he felt there were three options available to Ms Hutchon. The first was to assume that this was a case of reflux nephropathy and given the particular association between reflux nephropathy and fetal growth restriction manage the patient accordingly. The second was to contact the GP for further information (although that might not have been much use in the present case) and the third was to have a discussion with the local nephrology team.
- It was put to Mr Denbow that there was a fourth option; to arrange for a scan of the Claimant's Mother's kidneys at the same time as the 20-week pregnancy scan. Mr Denbow's response was as follows:
- Mr Denbow accepted under cross examination that if a consultant obstetrician had adopted his second option, contacted the patient's GP and received a response that an IVP and renal ultrasound scan in 1994 were reported as normal that would be reassuring to a treating obstetrician. When later in the cross examination it was put to Mr Denbow that the Claimant's Mother did not have renal disease there was the following exchange:
- Dr Sparey gave expert fetal medicine evidence on behalf of the Defendant. In her written report dated July 2023 she was clear that whilst growth scans from 28 weeks would have identified IUGR, in practice this would not have happened because "I do not believe that there was ever any indication to carry out an ultrasound assessment of fetal growth prior to the acute presentation with a four day history of reduced fetal movements on 03.10.08 and thus, whilst I do believe that fetal growth restriction would have been detected had scans been carried out, there was no opportunity to make the diagnosis prior to this date. This being the case, the outcome was sadly inevitable."
- In this context Dr Sparey agreed with Mr Tuffnell's opinion that the Claimant's Mother's history would not have mandated growth scans and was of the view that there was no indication to carry out an ultrasound assessment prior to the Claimant's Mother presenting with reduced fetal movements. She also expressed the opinion that had the Claimant's Mother been referred to an obstetrician for review in the first trimester she would have been discharged back to the community midwife for ongoing antenatal care "as she would correctly have been classified as having a low risk pregnancy due to the lack of any medical condition or other risk factors at this time."
- Mr Tuffnell is now retired from clinical practice but until 2019 he was a consultant in obstetrics and gynaecology at Bradford Hospitals. Post clinical retirement he continued his national role with the maternal mortality and perinatal mortality research interests until about 2021 and he has experience, amongst other matters, of being a member of the NICE intrapartum care guideline development group and the chair of the RCOG short answer questions examination committee. He has done medico-legal work for about 30 years, with more reports provided for defendants than claimants and in the last five years about 80-90% of his reports have been prepared on the instruction of a defendant.
- In his report dated July 2023 Mr Tuffnell opined as follows:
- The decision by Dr Hutchon on reviewing the Claimant's Mother's medical notes to continue to monitor her pregnancy on the basis that it was low risk was an acceptable approach
- If instead of this approach the midwife had referred the Claimant's Mother to a consultant at booking he considered that the "actual management would have been to plan for the care to be provided by the midwives with referral back if there were any concerns during normal care."
- There was no national guidance for growth scans in 2008. The Claimant's Mother did not have any signs of renal impairment. She had no proteinuria. Renal function, if it had been checked, would have been normal. She had no hypertension or urinary problems with infection. On that basis Mr Tuffnell would not have arranged growth scans for her based on her history even if she had been referred to him at 16 weeks.
- In his evidence in chief Mr Tuffnell indicated that Bradford Hospitals (which consisted of Bradford Royal Infirmary and St Luke's) was a large district general hospital and around the time of the present case there was only one nephrologist working in the trust. There were no joint clinics between obstetrics and nephrology and no direct referral route to a nephrologist. The only cases he remembered where a nephrologist was involved were those involving pregnant women who were on dialysis or at stage 4 renal failure just before they were going to go on dialysis. The nephrologist would not have been involved in cases where there was even mild actual impairment of renal function.
- Mr Tuffnell was asked in examination in chief about his views on the four possible treatment options for the Claimant's Mother that were discussed by Mr Denbow in his evidence (i.e. assume this was a case of reflux nephropathy and proceed down the route of fetal growth scans from 28 weeks, contact the GP for further information, discuss with the local nephrology team and arrange for the Claimant's Mother's kidney to be scanned when the 20 week fetal abnormality scan was undertaken). He said this:
- Under cross examination Mr Tuffnell, who had been present in court when Dr Hutchon gave evidence, said this:
- Mr Tuffnell was cross examined about the view expressed by Dr Andrews in his evidence to the court, namely that "I think it was incumbent upon the obstetrician to investigate the matter further at that point [i.e. an assertion by the patient that she had kidney scarring] with regards to the overall clinical picture". Mr Tuffnell said this:
- Mr Tuffnell was taken to the 2006 edition of Professor Nelson-Piercy's Handbook of Obstetric Medicine. His evidence was that "there needs to be renal impairment and that's why the table at the top of the page is quite important, because it shows that in women without renal impairment or even with only mild renal impairment it's not suggesting there is an increase of IUGR."
- Mr Tuffnell agreed with Dr Andrews and Mr Denbow that if a patient said she had kidney scarring and there was no evidence to the contrary, one cannot simply disregard this information but was adamant that "even with that history in the absence of any renal impairment, I would not have considered it necessary to arrange the further follow up that's been suggested." When pushed on the issue of whether renal scarring was something that an obstetrician had to take seriously he said this:
- On the question of potential effects on the unborn child of the maternal renal scarring he was very clear that "with the history of kidney scarring but no ongoing concerns, then to provide the type of antenatal care that Dr Hutchon suggested would be reasonable". It was put to him that the fact that there were no ongoing concerns at the start of the pregnancy did not inform whether the kidney scarring was going to produce problems of pre-eclampsia later on in the pregnancy and problems of IUGR later on in the pregnancy and that these were problems that should have been looked for. His response was that:
- This evidence was further expanded in response to a question from the court when Mr Tuffnell said this:
- Mr Tuffnell was of the clear view that by agreeing with the assessment of the Claimant's Mother's pregnancy as "low risk" Dr Hutchon did not dismiss the kidney scarring and that the suggestion that she did dismissed the purpose of ante natal care, which was to look for the complications that the Claimant's mother could have been at higher risk for. In his view "Dr Hutchon had made the judgment that, as she called it, the standard prescription of care would be sufficient in this circumstance and if there were any concerns, as in all pregnancies, there would be referral back."
- The Claimant relied on evidence from Professor John Wyatt and the Defendant from Dr Janet Rennie. At a meeting held on 19 February 2024 the neonatologists agreed that:
- On the basis of this level of agreement the neonatology experts were not called to give oral evidence at trial.
- I was referred to a number of contemporaneous publications. Amongst them (and relied upon for different reasons by both parties) was the Catherine Nelson Piercy Handbook of Obstetric Medicine chapter on renal disease. The heading "chronic renal disease" which starts at page 186 indicates that the effect of chronic renal disease on pregnancy includes preeclampsia and IUGR. Immediately afterwards it states that under "Factors influencing outcome" that "The outcome of pregnancy and any adverse effect on underlying renal disease are both influenced by:
- Presence and degree of renal impairment (see later)
- Presence and severity of hypertension
- Presence and degree of proteinuria
- Underlying type of chronic renal disease (see later)"
- The text then defines the degrees of renal impairment as mild, moderate and severe and on page 187 there is a section headed "effect of degree of renal impairment on pregnancy outcome". The first bullet point reads as follows:
- Table 10.3 sets out the effective degree of renal impairment on pregnancy outcome. It, together with the following sections on glomerulonephritis and reflux nephropathy are set out below:
- The Defendant suggested that when one looks at Table 10.3 it should be interpreted as saying that a pregnant woman with reflux nephropathy but no known renal impairment (which was the case for the Claimant's mother) was not at increased risk of IUGR. In fact, the factors influencing outcome on page 186 direct the reader to consider the underlying type of chronic kidney disease (hence the use of the words "see later" in parentheses) and as such any specific risk factors associated with that type of kidney disease. There is a section on page 188 that specifically deals with reflux nephropathy.
- Whilst I accept that Table 10.3 illustrates the general principle that the greater the degree of renal impairment the worse the pregnancy outcomes are, it is clearly intended to be read in conjunction with the section addressing the particular factors for this form of kidney disease. Whilst Table 10.3 states that as a general proposition women with mild kidney impairment have a 25% risk of "problems e.g. pre-eclampsia" and there is no entry in relation to IUGR (and I note that there was no indication of whether the reasons for this was a lack of reliable data or because there is no known risk) the section on reflux nephropathy states, after the second bullet point, that "about 25% of women develop pre-eclampsia and this risk is increased in cases of bilateral renal scarring" and in the third bullet point "even those with normal renal function and without hypertension pre-pregnancy are at an increased risk of hypertension (33%) and pre-eclampsia (15%)". As such, a woman with no known renal impairment (as was the case with the Claimant's mother) but a childhood history of reflux nephropathy has a 15% increased risk of preeclampsia. Such a women would not fall within the "mild" category of renal impairment in Table 10.3 unless this category also included women with no renal impairment (which would defeat the whole object of the table), hence illustrating the general nature of Table 10.3.
- The section on reflux nephropathy also states, after the fourth bullet point that "There is a particular association between reflux nephropathy and severe IUGR". Unhelpfully, there is no indication of any particular level of renal scarring that is required for this association to arise (in contrast to the second bullet point that specifically points out that bilateral renal scarring increases the risk of pre-eclampsia) and no indication of whether severe IUGR occurs in cases such as the Claimant's Mother (who provided clinical information to suggest reflux nephropathy but if she was suffering from this disease did not have any renal impairment and was not suffering from any conditions associated with reflux nephropathy (such as increased blood pressure or proteinuria)).
- As such, this textbook (which was in circulation in 2008 and which Ms Hutchon thought she had a copy of at home) may be read as suggesting (without condescending into any details) that there is an association between reflux nephropathy and IUGR but is not helpful on the issue of whether this association applies to a woman with normal renal function.
- This was however not the only textbook or other piece of medical literature in circulation in 2008 that is relevant to the present case. Professor Nelson-Piercy was also one of the joint editors of "Maternal Medicine Medical Problems in Pregnancy" (4th edition, 2007). Chapter 4, which dealt with Renal Disorders (and was authored by D. Williams and L. Lightstone) recommended at page 56, that there be screening for asymptomatic bacteriuria every 4-6 weeks for pregnant women with scarred kidneys due to reflux nephropathy, and noted (at page 58) that women with pre-existing renal disease are more vulnerable to pre-eclampsia but, in the part of the chapter that was provided to the court makes no reference to any link between reflux nephropathy and IUGR. I note that the entire chapter of this textbook was not provided and this includes the sections of the chapter covering the influence of renal function in the outcome of pregnancy. That said, I can safely assume that the Claimant's very experienced legal team would have provided any further parts of this chapter if they felt that they were relevant to the matters before the court.
- I was also provided with extracts from "High Risk Pregnancy Management Options" both 3rd edition (2006) and 4th edition (2011). Chapter 50 of the 3rd edition and Chapter 49 of the 4th edition deal with Renal Disorders. The authors of this chapter noted in the 4th edition (published after the events that this court is concerned with) that the cumulative knowledge in the field of acute and chronic renal conditions from an obstetric perspective was based "almost exclusively on retrospective studies addressing only a small number of cases, underscoring the critical need for large observational studies". This indicates that the evidential base available in or about 2008 would also have been low and this was an area that was not data heavy.
- Looking at the 3rd edition (which encapsulates the knowledge base in 2008 when the Claimant's Mother was pregnant) one can see that it is stated that "reflux nephropathy is characterised by renal scarring, reduced GFR, recurrent UTIs, proteinuria and hypertension. This combination of clinical features makes pregnancy in women with reflux nephropathy particularly high risk." One of the most prevalent pregnancy complications is stated to be superimposed preeclampsia. The authors of this chapter go on to comment that vesicoureteral reflux (VUR) is a familiar disorder and fetal VUR can be detected antenatally by obstetric ultrasound.
- At pages 1113-1114 is a table setting out a summary of management options for pregnant women with reflux nephropathy, with gradings for the quality of evidence and the strength of the recommendation. The "pre-natal" section of this table includes a recommendation to "screen for preeclampsia; fetal surveillance" and "screen fetus for VUR". In his evidence in chief Mr Denbow was asked what was meant by fetal screening in the context of the reference in this table to "screen for preeclampsia; fetal surveillance" and the following exchange took place:
- Mr Tuffnell also dealt with this edition of this textbook in his evidence to the court. He noted that "here the author is describing reflux nephropathy as being associated with reduced GFR, which is reduced renal function, recurrent infections, proteinuria and hypertension. And I think that anyone would consider that someone who had those features would be at high risk and would need further surveillance. But what I don't think this author deals with is somebody who has a history of reflux nephropathy, but without any of those consequences."
- I agree with Mr Tufnell's reading of this particular text; one has to consider the reference in the table setting out the management options for women with reflux nephropathy (found at pages 490-491 of the trial bundle) in the context of the clinical factors identified in the text as relating to reflux nephropathy. I also note that it is the "combination" of clinical factors that is said to make pregnancy in women with reflux nephropathy "particularly high risk". In this context I note that whilst the Claimant's mother reported that she had kidney scarring none of these other clinical factors were present prior to her presentation on 3rd October 2008 and she had regular ante-natal check ups which would have identified the presence of any of the other identified clinical factors. As late as 25th September 2008 none were detected.
- Mr Tuffnell also drew the court's attention to the later edition of "High Risk Pregnancy Management Options" (4th edition) which stated that "reflux nephropathy is common in women of childbearing age and is characterised by renal scarring and reduced GFR". He said this in his evidence in chief "It's interesting that this text, which only requires that relatively milder complication of nephrology doesn't then suggest that fetal surveillance will be needed for reflux nephropathy. So this text is actually accepting even with some mild impairment of renal function you wouldn't necessarily have additional fetal surveillance, whereas the prior text did suggest surveillance because it was including the other effects and implications."
- Mr Tuffnell also drew the court's attention to the RCOG 2012 green-top guidelines which only recommended growth scans for mothers with renal disease where there was renal impairment. Mr Tuffnell agreed with Mr Denbow's assessment that whilst the earlier 2002 guidelines gave guidance on how to manage a baby that had been identified as being small "they don't actually tell you when to do growth scans." In his evidence Mr Denbow acknowledged that the 2002 guidelines did not address when to scan a fetus, but instead were "talking about you've now got a small little fetus, how do you investigate, how do you manage that" rather than how do you work out whether you've got one.
- However, Mr Denbow was able to draw attention to a paper published in January 2008 by David Williams and John Davison titled "chronic kidney disease in pregnancy". This paper poses a number of questions including "how does chronic kidney disease affect pregnancy outcome?" to which the authors wrote the following:
- Table 3 indicates that women with a pre-pregnancy renal function serum creatinine value of less than 125 umol/L are at a 25% risk of experiencing fetal growth restriction. There is of course a cohort of women with creatinine levels of less than 125 umol/L who have normal renal function given normal serum creatine levels are 73 umol/L before pregnancy and range between 54 and 64 umol/L at various stages of pregnancy (see Table 2 in the paper) however the paper addresses "chronic kidney disease" in pregnancy and as with the "High Risk Pregnancy" (3rd edition) textbook, it is unhelpful to look at the table in isolation to the text, which makes it clear that it is one or more of the identified factors that are detrimental to fetal outcome. This is reinforced by the earlier sub-paragraph dealing with how pregnancy affects maternal kidney function which states "most women with chronic kidney disease who become pregnant have mild renal dysfunction and pregnancy does not usually affect renal prognosis (table 3)".
- The Claimant's Mother was not experiencing any of the identified clinical factors identified in the Williams and Davison paper when assessed by Ms Hutchon. I do not read this paper as authority for the proposition that a woman with kidney scarring but no renal dysfunction/no clinical factors identified in the paper is at a 25% risk of FGR.
- I turn now to the issues to be determined and remind myself of the first three questions that Ms Gumbel KC identified in her written opening (and which are set out in paragraphs 8(a), (b) and (c) above). These are helpful because when one analyses them, it becomes apparent that the Claimant's case on breach of duty and factual causation stands or falls with an analysis of whether a reasonably competent obstetrician working in a District General Hospital in 2008 would, or should, have been aware of a link between a mother with reflux nephropathy and no impaired renal function and IUGR.
- Ms Gumbel KC posed the question of whether the history given by the Claimant's Mother and the description of "cystitis: kidney scarring" were sufficiently serious to alert a competent obstetric consultant in 2008 to the risk of the Claimant's Mother having reflux nephropathy or chronic kidney disease.
- The NICE definition of chronic kidney disease is defined as "a reduction in kidney function or structural damage (or both) present for more than 3 months, with associated health implications". The Claimant's Mother was not suffering from hypertension, proteinuria or recurrent UTIs at the time of the conception of the Claimant or when she had her appointments with the two midwives on 17 April and 16 May 2008. Given she had normal serum creatinine levels on 3 October 2008, when she was found to be suffering from severe pre-eclampsia, on the balance of probabilities she would have had normal serum creatinine levels at all earlier stages of her pregnancy and did not have impaired renal function at any stage of her pregnancy. Her medical records indicate that prior to her pregnancy with the Claimant kidney scarring did not feature when she gave her medical history to healthcare professionals; by ways of example on 30 July 2004 Dr Simpson (her then new GP) undertook a new patient check history and there is no reference to kidney scarring, the referral letter that Dr Dickinson wrote to EPAC on 1 April 2008 made no mention of kidney scarring (and the notes attached thereto indicated there were no chronic issues) and when the Claimant's Mother gave her history at her EPAC appointment on 3 April 2008 it is noted that she mentioned "CYTISE (clear now)" but there is no mention of kidney scarring.
- There are further factors after the event of the Claimant's birth which also indicate that the fact that the Claimant's Mother had been told that she had a scarred kidney almost certainly did not cause her concern in 2008, the most notable being that notwithstanding the circumstances surrounding the Claimant's birth, and having received the letter from Mr Griffin dated 10 March 2009 referring to the risk factor arising from her recurrent bladder infections and having been in possession of Dr DuPont's opinion that she should undergo a DMSA renogram for several years now (not only for her own sake but because there is emerging evidence that reflux nephropathy can be familial) she has not sought any further investigation into her reported kidney scarring in the last 16 years.
- In his evidence to the court Dr DuPont acknowledged all of these matters but asserted that the Claimant's mother fell within the definition of chronic kidney disease at the time of her pregnancy with the Claimant because:
- If one drills down into that analysis, the Claimant's claim is that his mother should have been subject to growth scans during her pregnancy due to the risk of IUGR. If the associated health implications had not included that risk the Claimant does not (and in my view cannot) maintain that growth scans were mandated. Whilst Mr Griffin referred in his letter to the Claimant's mother to the risk of pre-eclampsia arising from her residual kidney disease, this is not how the case has been put on behalf of the Claimant, either in the particulars of breach of duty or in the expert evidence from Mr Denbow or in the Claimant's submissions to the court. It follows that the Claimant must establish on the balance of probabilities that a competent obstetric consultant in 2008 would (or should) have been alert to the fact that reflux nephropathy in the absence of renal impairment carried a risk of IUGR.
- That analysis is also intrinsic to the expert evidence from Mr Denbow, whose opinion is that "the significant risk factor of F[etal] G[rowth] R[estriction] of maternal renal disease was overlooked" and that if the previous renal history was not easily accessible, the obstetric team should have made the pragmatic decision to assume the diagnosis of reflux nephropathy and should have offered serial growth scans "due to the known association between reflux nephropathy and FGR".
- Whilst Dr Andrews' starting point in his written report was that the Claimant's Mother did not have chronic kidney disease and was probably mistaken about having a scarred kidney he was forced to accept under cross examination that a treating obstetrician would have to work on the basis of what the Claimant's Mother told them until that account could be displaced. She told them that she had kidney scarring. That account, whilst not supported by objective evidence in the form of a scan that established that this was definitively the case, could not be ruled out during pregnancy. In light of the evidence from Dr DuPont, Dr Andrews, Mr Denbow and Mr Tuffnell on this issue, I accept that, to use a phrase adopted by Mr Denbow, in real time Dr Hutchon was beholden to work on the basis that the Claimant's Mother had a scarred kidney. This was information provided by an intelligent, articulate woman (and I also note that it is not the sort of information that a lay person is likely to conjure out of nowhere; the possibility of kidney scarring is not something that a lay person is likely to be aware of absent having been informed by a medically qualified person that they had it).
- It follows that the arguments proffered at trial about whether the Claimant's Mother did as a matter of fact have a scarred kidney at the time of her pregnancy do not take matters any further forward (subject to one submission made by Mr Booth KC in relation to factual causation which I deal with later). In my clear view the expert evidence strongly supports the finding that Ms Hutchon was obliged to work on the basis that the Claimant's Mother did have a scarred kidney. I note that there is nothing in Ms Hutchon's evidence to suggest that she did anything other than work on this basis when assessing the risks associated with the pregnancy and insofar as it is necessary for me to make a finding to that effect I do so.
- However, a scarred kidney on its own would not meet the definition of chronic kidney disease given the NICE definition unless there were associated health problems. That leads one back to the central question in this case, namely whether a reasonably competent obstetrician should have been aware that there were associated health risks, namely IUGR, as a result of this particular mother (who had no renal impairment) having a scarred kidney due to reflux nephropathy. If the answer to that question is yes, then strictly speaking it matters not whether the Claimant puts his case on the basis that the history given by his mother was sufficiently serious to alert a competent obstetrician in 2008 to the risk that his mother had reflux nephropathy or chronic kidney disease. Either way, the facts were sufficiently serious enough on the Claimant's case to require further investigation and for growth scans to be mandated from 28 weeks.
- For the sake of completeness I note that Ms Hutchon and Mr Tuffnell both accepted in their evidence that if there has been any evidence of renal impairment, they would have taken the view that the Claimant's Mother did suffer from, for want of a better term, clinically significant kidney disease. That would have led Ms Hutchon to adopt a different route to managing the Claimant's Mother's pregnancy; whilst it is not necessary for me to make findings in this regard having considered the evidence of Ms Hutchon and Mr Tuffnell it more likely than not that care would not have been midwife led and would have included growth scans from 28 weeks.
- In her evidence to the court Ms Hutchon, who was at pains to put herself in the position she was in in 2008, accepted that one possibility from the history of recurrent cystitis and kidney scarring was reflux nephropathy. It is also clear from Ms Hutchon's evidence that in the case of the Claimant's Mother she did not consider that reflux nephropathy was a serious possibility because she did not have any evidence of a history of childhood cystitis. That lack of history was as a result of that precise question not being asked of the Claimant's Mother.
- In this context the expert midwifery evidence is relevant (although not in any way determinative of the case given there was as a matter of fact a review by Ms Hutchon of the decision to assign the pregnancy to the low-risk pathway). I have already considered this expert evidence and commented that there was a lack of logic in the reasoning that Ms Fraser provided in her oral evidence to the court when she suggested that it would have been helpful for the Claimant's Mother to be seen by a consultant. This is to be contrasted with the clear and logical approach of Ms Helleur. She adopted an approach that the information available at the time of booking in did not exclude a chronic renal condition and was something out of the ordinary (and noted, with some force, that midwives are experts in normality). Ms Helleur's approach was consistent with the evidence of Dr DuPont and, ultimately, under cross examination, with the approach that Mr Andrews took (namely that it was incumbent on the obstetrician to assume that the Claimant's Mother be taken at face value when she said she had kidney scarring and "to investigate the matter further at that point with regards to the overall clinical picture"). Insofar as it is necessary to do so I prefer the evidence of Ms Helleur to that of Ms Fraser. It was in my view incumbent on midwife Carbery to refer the Claimant's Mother to Ms Hutchon for further review before a final decision was made as to whether the pregnancy could be managed on the low-risk pathway.
- However, given that the assignment of the Claimant's Mother's pregnancy to the low-risk pathway was subsequently reviewed by Ms Hutchon any failure on the part of the midwife cannot have ultimately caused any damage that the Claimant suffered. It was the review of Ms Hutchon that is key in this case; either it amounted to a breach of the duty of care that she owed to the Claimant (in which case for the reasons I set out in paragraphs 170 to 172 below causation would also be established) or it did not amount to a breach of the duty of care, and for the same reasons set out in paragraphs 170 to 172 below a face to face consultation would have made no difference to the outcome on causation.
- It was clear from Ms Hutchon's evidence that if she had been aware that there was a history of childhood cystitis she would most likely have come to the conclusion that one possibility from the Claimant Mother's history was reflux nephropathy. Ms Hutchon was however also clear that in 2008 she was not aware of any connection between reflux nephropathy and IUGR in the absence of functional kidney abnormality. In other words, even if she had come to the conclusion that she was looking at a possible case of reflux nephropathy, her judgment on the risks associated with this particular pregnancy would not have changed.
- Having carefully considered Ms Hutchon's evidence I am satisfied and find that when reviewing the Claimant's Mother's pregnancy she would, in addition to considering the two pages of notes prepared by midwife Carbery, have considered the (clear) results of the mid-stream urine test taken at the booking in appointment, the letter written by the GP to the Early Pregnancy Unit and any information on the trust's system about the Claimant's mother (including old MSU test results). On the basis of that information Ms Hutchon undertook a review and agreed with the decision to assign the pregnancy to the low-risk pathway. In so doing she did not (as has been suggested in cross examination on behalf of the Claimant) ignore the fact that the Claimant's mother had kidney scarring. It was one of the factors that she took into account when considering that the low risk pathway was appropriate to manage this pregnancy. Ms Hutchon was aware that a history of cystitis and kidney scarring posed an increased risk of urinary tract infections during pregnancy. She took into account that this was a risk that would be addressed on the low risk (or standard) prescription for antenatal care by way of regular mid-stream urine tests.
- Both nephrology experts accepted that the Claimant's Mother's pregnancy would have been managed by the obstetrics department rather than the nephrology department. One must therefore turn primarily to the evidence from the expert obstetricians to answer the question of whether there was a breach of duty in assessing the Claimant's mother's pregnancy as low risk.
- I have carefully considered the evidence from Mr Denbow and Mr Tuffnell. Both were thoughtful and considered expert witnesses. They each have a wealth of experience and clearly approached their tasks from their respective clinical backgrounds, which do vary somewhat. Mr Denbow is and has always been a consultant in a large teaching hospital and very fairly acknowledged the greater depth and breadth of resources that were available to him as a result. Mr Tuffnell was a consultant in a large District General Hospital; he was clearly more familiar with the working conditions that Ms Hutchon was facing in 2008 than Mr Denbow, who expressed genuine surprise in the witness box about the information that Mr Tuffnell shared with him at the experts' joint meeting about the lack of scanning and other resources (such as access to nephrology colleagues) in a District General Hospital in 2008.
- Mr Tuffnell gave evidence that whilst he did not have any first-hand knowledge of the availability of ultrasound resources in the West Midlands in 2008 the description in the 2009 paper by Jason Gardosi et al of "an acute shortage of ultrasound resources" and "a lack of trained ultrasound staff" did not sound surprising to him and that in 2008 there were fewer sonographers available than today. That, together with an expansion of regular 20-week fetal abnormality scans in about 2008 meant "there was less sonographer time to scan women who had a different risk threshold for growth." The decision that Ms Hutchon took in 2008 must be looked at in the real world that she worked in at the time. That world was far closer to the one that Mr Tuffnell worked in in 2008 than Mr Denbow did. I have no doubt that the first option posited by Mr Denbow in his evidence (to assume that this was a case of reflux nephropathy with a risk of IUGR and to proceed down the route of fetal scans from 28 weeks) was a genuine opinion and, as Mr Tuffnell stated in his evidence, not unreasonable. However, it was a view borne out of a different clinical experience to that facing Ms Hutchon in 2008.
- Mr Tuffnell's view that it was reasonable for Ms Hutchon to have reviewed the Claimant's mother's pregnancy as being suitable for the low risk (or standard prescription) pathway without holding face to face consultation was based on the clinical presentation of the Claimant's mother; despite reporting kidney scarring she did not have any signs of renal impairment, had no proteinuria, no hypertension or urinary problems with infection and if she had been checked her renal function would have been normal. Those are all reasonable factors for Mr Tuffnell as an expert witness to take into account. There is nothing illogical or indefensible about this opinion unless it can be shown that Mr Tuffnell had omitted a materially relevant factor i.e. a known association in 2008 between a pregnant woman with reflux nephropathy but no renal impairment and IUGR.
- Mr Tuffnell was very clear that his views would have been different if the Claimant's Mother had been experiencing renal impairment and explained the possible effect of renal impairment in the earlier stages of pregnancy on placental development. However, there was no evidence at all at the time that Ms Hutchon undertook her assessment that the Claimant's Mother had any renal impairment.
- The medical literature available in 2008 and which I have already reviewed did not paint a clear picture on the issue of whether reflux nephropathy absent impaired kidney function posed an elevated risk of IUGR. I have already commented in detail on the 2006 edition of the Handbook of Obstetric Medicine by Catherine Nelson-Piercy and the lack of details and clarity in the context of the statement that "there is a particular association between reflux nephropathy and severe IUGR". The fact that this section, and Table 10.3, were interpreted differently by Mr Denbow and Mr Tuffnell is in my view not as a result of one of them obviously being correct in their interpretation of what the text says and the other not being, but rather in the lack of clarity in the textbook itself.
- In her written closing submission Miss Gumbel KC drew the court's attention to High Risk Pregnancy 3rd edition and the opening comments in the chapter on Renal Disorders that state:
- Whilst these are accurate extracts, it should however also be noted that the first extract set out above goes on to state that:
- This increased risk of pre-term growth-restricted babies as a result of reduced kidney function aligns with the evidence from Mr Tuffnell about the possible effect of renal impairment in the earlier stages of pregnancy on placental development.
- Ms Gumbel KC also submitted in her closing submissions that the table set out at pages 490-491 of High Risk Pregnancies 3rd edition includes fetal screening when there is maternal reflux nephropathy. I have already commented in some detail on this table and the court's view that (as was propounded by Mr Tuffnell) one must consider the table in the context of the combination of clinical factors that the text identifies as making pregnancy in women with reflux nephropathy "particularly high risk." In the present case the Claimant's Mother did not present with any of these clinical factors at the time of assessment by Ms Hutchon or at any time in her pregnancy prior to her presentation on 3 October 2008. The same point can be made about the 2008 paper by Williams and Davison.
- Other literature that was available in 2008 and that the court was referred to does not support the proposition that reflux nephropathy per se is associated with an increased risk of IUGR.
- Having carefully considered all of the contemporaneous literature made available to the court, whilst no doubt Mr Denbow's view that in 2008 there was a known association between reflux nephropathy and FGR is genuinely held, Mr Tuffnell's opposing view that "I would not have thought someone with a history of kidney scarring but without ongoing concerns about their renal function was at higher risk for IUGR" was equally genuinely, and validly held. I note that Mr Tuffnell's expert opinion was supported by Dr Sparey, who stated under cross examination that "I would accept that it would be best practice to see a patient face-to-face where she gives a possible history of possible kidney problems, but I don't think that it was unreasonable of Dr Hutchon to do what she did."
- For all the reasons that I have given Mr Tuffnell's (and Dr Sparey's) opposing approach to that of Mr Denbow amounts to a genuine difference of opinion. It has a logical basis and the conclusions reached are defensible when one looks at all of the evidence available to the court. It follows that the view taken by Ms Hutchon when reviewing the Claimant's Mother's case and agreeing that it was suitable to be managed on the low-risk pathway was reasonable and was one that it was open to a reasonably competent obstetrician working in a District General Hospital in 2008 to make. In all the circumstances, the Claimant must fail on establishing breach of duty and the claim must be dismissed.
- Whilst not strictly necessary, if, contrary to my judgment, there was a breach of duty by Ms Hutchon on 20 May 2008 (and this can only have been on the basis that in 2008 a reasonably competent obstetrician would or should have been aware that reflux nephropathy per se increased the risk of IUGR and mandated growth scans) I agree with the submission made by Mr Booth KC in his closing submissions that the net result would have been a face-to-face appointment between the Claimant's Mother and Ms Hutchon.
- In this context Ms Hutchon explained clearly to the court, both in her written and oral evidence, what her thought processes would have been and what she would probably have done. In her written evidence she said that she would have requested further information from the Claimant's Mother's GP, in addition to eliciting further information from the Claimant's Mother. This would more likely than not have resulted in Ms Hutchon being informed that the Claimant's Mother suffered from cystitis as a child and when she was 17 or 18 was told that she had a scarred right kidney, that the IVP undertaken in 1994 returned a clear result, that there had been no diagnosis of any acute or chronic renal condition and that there was no ongoing referral of specific care or treatment being received.
- Ms Hutchon was clear in her written (and oral evidence) that having considered these factors she would have considered it appropriate for the Claimant's Mother to be under midwifery led care. The rationale for this was that there were no risk factors that supported obstetric led care. It will therefore be apparent that this particular argument on causation also stands or falls with the analysis of the question of whether in 2008 a reasonably competent obstetrician would or should have been aware that reflux nephropathy (absent renal impairment or other clinical factors) increased the risk of IUGR, because an indication of reflux nephropathy (which Ms Hutchon accepted she would have considered if she had been aware of the childhood cystitis in the present case) would not have provided the reassurance that Mr Denbow indicated in cross examination would have been required to refer the Claimant's Mother back to the low risk, midwife led antenatal care pathway. As such, if the Claimant had succeeded on establishing breach of duty he would also have established factual causation, subject to the point considered below.
- In her oral evidence to the court Ms Hutchon also suggested that she might have requested an ultrasound scan of the Claimant's Mother's kidneys at the same time as the 20-week fetal anomaly scan. Both of the expert nephrologists accepted that this was a reasonable possibility (it has to be said with rather more enthusiasm on the part of Dr Andrews than Dr DuPont). Mr Tuffnell also accepted that this was a possibility. It was only Mr Denbow who dismissed this as an option, and it was clear from his reasons that they were largely based on his experience of working in a large teaching hospital, with the consequent access to nephrology colleagues whose opinions he is able to seek (which is in stark contrast to Mr Tuffnell's experience in 2008).
- Mr Booth KC submitted in his closing submissions that if an ultrasound scan of the kidneys had been undertaken at 20 weeks it would probably have been reported as normal, and there would have been no obligation to regard the pregnancy as one requiring anything other than the standard prescription for care (to use Ms Hutchon's words) in the face of such a report. Indeed, on the balance of probabilities when considering the risk of renal scarring (more likely than not there was none) together with the Claimant's mother's normal blood pressure readings, normal urine test results and (if tested) normal renal function, and when considering the paucity of sonographers and scanning resources, it is more likely than not that fetal growth scanning would not have been performed at all. This alternative defence to the issue of factual causation was not propounded until trial and is predicated on the court determining the outcome of something that did not happen, but which could have been done by the Defendant at the time if it had chosen to do so.
- In her closing submissions Miss Gumbel KC submitted that a 20-week scan would not have been sufficient assistance without a nephrology view to explain it, and a nephrologist would have pointed out that an ultrasound scan had a significant risk of being inconclusive. Only a renogram (which was not possible during pregnancy) would have been conclusive.
- Miss Gumbel KC also relied upon the decision in Keefe v Isle of Man Steam Packet Co Ltd as authority for the fact that the suggestion at trial that Ms Hutchon might have asked for scans of the Claimant's Mother's kidneys at 20 weeks should be considered by the court with a degree of benevolence towards the Claimant's evidence (and a correlative degree of criticism towards the Defendant's evidence).
- There is some force in Ms Gumbel KC's submissions. Under cross examination Dr Andrews accepted that unless there were further investigation an obstetrician would have needed to act on what they had been told (i.e. there was kidney scarring). The approach to factual causation taken by the Defendant in closing submissions in effect seeks to circumvent that evidence by saying "if we had carried out further investigation it would more likely than not have indicated no renal scarring." As such it falls within the scenario considered in the Keefe case.
- Taking the Keefe approach (if I may put it that way) the Claimant's evidence (from Dr DuPont and Ms Helleur) was that unless renal scarring could be excluded (and it could not during pregnancy) the Claimant's Mother should have been risk assessed and treated on the basis that she had a scarred kidney. If an ultrasound had been undertaken it would not have been as accurate as a DMSA scan and during pregnancy the possibility of renal scarring could not have been excluded. In that regard Dr DuPont relied upon a paper published by the Canadian Urological Association in August 2017 comparing ultrasound compared to DMSA scan results and which concluded that "unique US studies, even with newer equipment, are not sensitive enough to detect renal anomalies. US could not be a substitute for DMSA scan. We consider US and DMSA scintigraphy to be complementary investigations the former provides structural information and the latter, functional details."
- Adopting a benevolent approach to the Claimant's evidence, whilst as a matter of fact the nephrology experts were both of the view that an ultrasound scan of the Claimant's mother's kidneys was one possible route open to Ms Hutchon, the more cautious approach adopted by Dr DuPont would in my view have been reasonable if there had been a known association between reflux nephrology per se and IUGR, given the risks for the fetus if IUGR had developed. Those risks would also have militated in favour of growth scans from 28 weeks, even taking into account the issues in 2008 around the availability of ultrasound scans. As such, if the Claimant had established a breach of duty I would also have found that the Claimant had established factual causation.
- As far as medical causation is concerned, if it had been necessary to consider this issue, given that the Claimant has pleaded his case on a material contribution basis, I would have found that medical causation was made out given Dr Sparey's acceptance under cross examination that "had the team known that the baby was small they would have been doing CTGs, that they would have detected changes in the CTGs and they would have delivered the baby earlier than was actually the case" and "I think earlier delivery is likely to have resulted in a better outcome."
- Nobody looking at this case could fail to understand the very real human story that it involves. In his day-to-day life "the Claimant" is a 15 year old child who has suffered irreparable brain damage and whose life is moulded by that fact. "The Claimant's Mother" is a loving, caring mother who, together with the Claimant's father provides care for the Claimant day in day out. I have no doubt that they both worry about what the future may bring, in both the short and longer term. I have no doubt that in the last 15 or so years they will have gone over and over the details of the pregnancy. It is human nature to do so, and it is also human nature to wonder whether traumatic events could, or should, have been avoided. In doing that, it is very easy to apply a degree of retrospectivity (it is often said that we all have 20:20 vision with the benefit of hindsight). However, the role of the legal system is not to retrospectively apply 20:20 vision but to consider whether the care that was provided to the Claimant in 2008 (whilst still in his mother's womb) fell below the standard of care that was expected of the Defendant's employees. In this case a close analysis of the evidence reveals that there was no breach of the duty of care owed to the Claimant. Dr Sparey neatly summarised the situation when she said that there was no basis on which to order growth scans and absent such scans "the outcome was sadly inevitable."
HHJ Richardson:
Introduction
The allegations of breach of duty and causation pursued at trial
(a) Ensuring a prompt midwifery referral for a senior medical obstetric review and consultant led obstetric care because of the Claimant's Mother's medical history of cystitis and kidney scarring problems associated with renal disease and suggestive of reflux nephropathy. This risk should have been categorised as a chronic medical condition by midwifery staff on the booking/antenatal forms and resulted in a referral for consultant led obstetric management. This medical risk does not appear to have been taken into account despite being noticed in the Claimant's Mother's records on several occasions at booking.
(b) Senior medical obstetric staff would or should have recognised that the Claimant was at risk of Intrauterine Growth Restriction ("IUGR") if the pregnancy had correctly been assessed as high risk and a referral for consultant led obstetric care had been achieved.
(c) With competent care the Defendant should have recognised the association of a medical history of chronic renal problems with IUGR and regular scans to assess the fetal growth would have been arranged from around 28 to 30 weeks as accepted by Mr Griffin in the letter [that he sent to the Claimants' parents following their meeting with him on 10 March 2009).
"With adequate monitoring during the antenatal period it should and would have been apparent on scanning at 28-30 weeks that the Claimant was developing signs of IUGR. Thereafter increased frequency (depending on findings) of serial scans should have been performed and the Claimant's Mother's pregnancy monitored closely by senior medical obstetric staff who would and should have ascertained when the fetus was at increasing risk of hypoxic ischaemic damage. Delivery would and should have been planned after administration of corticosteroids to promote fetal lung maturation, if time allowed. On the balance of probabilities a medically planned delivery would have occurred between 32 and 33 weeks and avoided the Claimant developing hypoxic-ischaemia in the period prior to delivery."
Summary of key issues
(a) Whether the history given by the Claimant's mother and the description recorded in the notes of "cystitis: kidney scarring" were sufficiently serious to alert a competent obstetric consultant in 2008 to the risk of the mother having reflux nephropathy or chronic kidney disease.
(b) Whether in the circumstances of (a) the Claimant's mother's pregnancy should have been assessed as low risk by the consultant or whether it was a breach of duty for this to be the assessment.
(c) Whether if the assessment had been competent and the pregnancy assessed as high risk because of the history of kidney scarring on the balance of probabilities the Claimant's mother would have had growth scans at 28 weeks and further investigation of Intrauterine Growth Restriction ("IUGR") thereafter.
(d) Whether following scans at 28 weeks and thereafter the Claimant would have been delivered earlier so as to avoid injury.
Chronology of key events
"cystitis: kidney scarring".
' 'S/B C. Griffin P.E.T For magnesium sulphate. Anaesthetist arrived
21:20. To try for IV Access (21.15)
Mag Sulphate commenced @ 25mls/hr, altered to 150 mls/hr
(21.35)
SRC inserted by Mr Griffin ++++ protein All bloods taken + set (sic) by courier BP 150/93 P=83
(21.40)
Written in retrospect
Pt arrived H/O DAM (sic) for 4 days P/A SFH = 29cm Not (illegible) to size CTG = reduced variability. PV/E Cx Os closed Cephalic @ - 2 Plan Made for delivery. Pt + partner informed. Informed Mr Chris Griffin. Paeds steroids given
(untimed)
SS by Mr Griffin O+G Consultant.
EFW = 1.3kgs
Reverse EDF
Small (illegible)
Plan: Stabilise mum & deliver.
△ Severe pre-eclampsia
Clonus 5 beats
Hyperreflexia
MgSO4 stat dose.
IV access x 2 IDC
FBC, UEC's Urate, Coagulations
A Line
(21.50)
A line inserted.
CTG continues baseline 145bpm.
Variability
(22.00)
Nicola Wall cons anaesthetist present.
Deceleration noted ↓ 80bpm
Mr Griffin aware nil ordered.
(22.10)
IV fluids commenced Hartmanns
(22.30)
Note made by the consultant Mr Griffin:
Much improved now.
No clonus
No visual disturbances
No labour CTG No change.
⃣ T/F to BHH as theatre still occupied here & by the time we have blood
results back will be in Heartlands.
Na 13 5 Alb 37 Bili 5 K 4.0 Tot Prot 72 Urate 322 Urea 4.2 ALT 48 Creat
6.0 ALP 136"
(23.05)
Ambulance ordered
(23.06)
Ambulance arrived
(23.30)
"It was a pleasure meeting you today at Solihull Hospital to go over the issues surrounding the birth on 4 October 2008 of your son PXE. We covered a lot of areas during our consultation and I thought I would summarise them as follows:
1. My concerns over your pregnancy care are that you had a risk factor for preeclampsia which was the residual renal disease from your recurrent bladder infections. This in itself should have prompted us to have been a bit more vigilant about the size of baby and even considered a 28 weeks scan/32 weeks scan for growth.
2. I notice that your urine was not tested on 17 July by the midwife at her visit though I do notice that two mid-stream urines were sent on 24 June and 30 July which were both normal.
3. The measurement of 30cm made on 25 September when you were at 32 weeks is difficult to believe when I measured you on the night of admission to find 26cm was the size of your abdomen. On the night of 3 October when you came in I feel that we recognised the severity of your condition and treated you appropriately for this with PXE being born with good Apgars which point towards good compensation for the findings of placental infarction. I think that this placental infarction had occurred between 25 September and date of delivery.
[Advice re future pregnancies given]
In summary the question is could we have prevented such an acute change or course of events. If we had a 28-30 weeks scan the answer would be "probably" as we would have predicted a smaller than normal baby size and would hopefully then with intensive monitoring have picked up your pre eclamptic changes to prevent the placental infarction (lack of your blood supply to the placenta for PXE) which may be linked to any long term problems that PXE may face."
The applicable legal framework
"The test is the standard of the ordinary skilled man exercising and professing to have that special skill. A man need not possess the highest expert skill; it is well established law that it is sufficient if he exercises the ordinary skill of an ordinary competent man exercising that particular art."
And
"A man need not possess the highest expert skill; it is well established law that it is sufficient if he exercises the ordinary skill of an ordinary competent man exercising that particular art . in the case of a medical man, negligence means failure to act in accordance with the standards of reasonably competent medical men at the time."
"In Wilsher v Essex AHA [1987] 1 QB 730 the Court of Appeal for the first time gave detailed consideration to the standard of care required of a junior doctor. (This issue did not arise in the subsequent appeal to the House of Lords). The majority of the court held that a hospital doctor should be judged by the standard of skill and care appropriate to the post which he or she was fulfilling, for example the post of junior houseman in a specialised unit. That involves leaving out of account the particular experience of the doctor or their length of service. This analysis works in the context of a hospital, where there is a clear hierarchy with consultants at the top, then registrars and below them various levels of junior doctors. Whether doctors are performing their normal role or 'acting up', they are judged by reference to the post which they are fulfilling at the material time. The health authority or health trust is liable if the doctor whom it puts into a particular position does not possess (and therefore does not exercise) the requisite degree of skill for the task in hand."
"Mr. Brennan renewed that submission both before the Court of Appeal (who unanimously rejected it) and before your Lordships. He submitted that the judge had wrongly treated the Bolam test as requiring him to accept the views of one truthful body of expert professional advice even though he was unpersuaded of its logical force. He submitted that the judge was wrong in law in adopting that approach and that ultimately it was for the court, not for medical opinion, to decide what was the standard of care required of a professional in the circumstances of each particular case.
My Lords, I agree with these submissions to the extent that, in my view, the court is not bound to hold that a defendant doctor escapes liability for negligent treatment or diagnosis just because he leads evidence from a number of medical experts who are genuinely of opinion that the defendant's treatment or diagnosis accorded with sound medical practice. In the Bolam case itself, McNair J. [1957] 1 W.L.R. 583 , 587 stated that the defendant had to have acted in accordance with the practice accepted as proper by a ' responsible body of medical men.' Later, at p. 588, he referred to 'a standard of practice recognised as proper by a competent reasonable body of opinion.' Again, in the passage which I have cited from Maynard's case [1984] 1 W.L.R. 634 , 639, Lord Scarman refers to a 'respectable' body of professional opinion. The use of these adjectives - responsible, reasonable and respectable - all show that the court has to be satisfied that the exponents of the body of opinion relied upon can demonstrate that such opinion has a logical basis. In particular in cases involving, as they so often do, the weighing of risks against benefits, the judge before accepting a body of opinion as being responsible, reasonable or respectable, will need to be satisfied that, in forming their views, the experts have directed their minds to the question of comparative risks and benefits and have reached a defensible conclusion on the matter." [my emphasis]
"19. If it is a defendant's duty to measure noise levels in places where his employees work and he does not do so, it hardly lies in his mouth to assert that the noise levels were not, in fact, excessive. In such circumstances the court should judge a claimant's evidence benevolently and the defendant's evidence critically. If a defendant fails to call witnesses at his disposal who could have evidence relevant to an issue in the case, that defendant runs the risk of relevant adverse findings see British Railways Board v Herrington [1972] AC 877, 930G. Similarly a defendant who has, in breach of duty, made it difficult or impossible for a claimant to adduce relevant evidence must run the risk of adverse factual findings."
The witnesses of fact
The Claimant's Mother's evidence
The evidence from the maternal grandmother
Mr Griffin's evidence
"As the most experienced fetal maternal medicine specialist at the then Heart of England NHS Trust I was deeply concerned that contemporaneous knowledge and practices were not followed in the case of [the Claimant's mother].
Upon reviewing the notes I felt that an abnormal pregnancy had been normalised. Had I been the consultant in charge of [the Claimant's mother]'s antenatal care I would have ensured that scans were performed at 28 and 32 weeks."
Mrs Hickman's evidence
Midwife Carbery's evidence
"I probably would have questioned it at the time and the fact that the mum wasn't under a renal consultant, wasn't having regular follow-ups and was on no medication I didn't perceive that as a chronic kidney disease and I put it as low."
Ms Hutchon's evidence
"so I think because it didn't say "childhood infection", it just said "cystitis", I think I would have surmised that she had the common type of recurrent cystitis in your teens and 20s and perhaps even an episode of pyelonephritis or something to account for the scar."
"The information that I had was not of childhood infection, it was of just of cystitis and the scar, so although it's possible that it was from vesicoureteral reflux as a child, I didn't have a history of vesicoureteral reflux as a child."
"if [the claimant's mother] had reported a history of kidney scarring, I would have asked her about it to further establish what evidence there was of kidney scarring as there would have been nothing in her medical records from the trust to confirm that diagnosis. In any event, kidney scarring is very different to kidney disease which does require consultant led care in expectant mothers. In the absence of any specific disease or any other chronic medical condition necessitating the need for consultant led care, I would have considered it appropriate for the Claimant's mother to be under midwifery led care and I am likely to have recorded in the notes that she was for "standard care". If I had had any concerns from what the Claimant's mother had told me in clinic about her history, I would have made an entry in the notes to request that the midwife sees her monthly for blood pressure and urine tests so that her condition could be monitored. The rationale being that if there were any concerning features, she could always be re-referred back to consultant led care."
"The urgency for improving antenatal detection of the small for gestation (SGA) or intrauterine growth restricted (IUGR) baby increases with the awareness that foetal growth restriction is a common precursor of adverse outcome . Such surveillance is done by regular fundal height assessment, ultrasound biometry or a combination of both methods.
.
Where ultrasound is not available, fundal height measurement can be used as a proxy for estimating the gestational age of the pregnancy, or the weight of the fetus. More commonly, it is used for fetal growth screening. Where scans are available, ultrasound biometry is used when fundal height is below expectation. Serial assessment of growth by ultrasound in all pregnancies is not feasible, even in developed countries."
"To reach its full potential as a screening tool for intrauterine growth restriction, fundal height assessment needs to be established as part of a fully integrated system. It requires clearly defined methods and standards for measurement and plotting, and care pathways for further investigation and management. The test must complement ultrasound biometry for assessing mothers for whom fundal height is not suitable, or who have an elevated risk of fetal growth restriction or in pregnancies which are already recognised as of increased risk because of suspected abnormal growth.
Thus, the overall performance of a growth screening programme, in terms of the proportion of SGA babies who are detected antenatally, depends on adequate resources for 3rd trimester ultrasound which are not always available. In the West Midlands, a two-pronged approach is being adopted, with intensive fundal height training workshops and a parallel programme of community growth scanning service delivered by midwives trained in special, short ultrasound courses.
A vital component of the service is ongoing audit. Antenatal detection of fetal growth restriction has recently been accepted by health service commissioners as a key quality indicator in the West Midlands, and information about its performance is being audited through routine electronic data collection. This provides an ongoing focus on the importance of growth restriction, and has in turn already led to demonstrable local improvements in maternity services".
The expert midwifery evidence
"the midwife should have asked for an obstetric review and not classed [the claimant's mother] as low risk prior to her being reviewed by an obstetrician. The midwife would not have known the extent of the recurrent cystitis and renal scarring on the basis of the history given by [the claimant's mother] at booking. They had no notes to refer to and could not know that her renal function was normal from the basic information given. In my opinion, it was a breach of duty by the midwife not to refer[the claimant's mother] for obstetric review.
I have seen the evidence of midwives Hickman and Carbery who say that they did not consider [the claimant's mother] to be high risk and that there was no requirement to refer her to consultant care. They say this is because she did not disclose that she was under review, taking medication or having active treatment for the condition. In my opinion the midwives could not have known the extent of the scarring of the kidneys, the renal function or the impact from pregnancy. [The claimant's mother] should have been referred. I defer to obstetric opinion to say what should have been done if she had been referred."
"at the booking appointment [the claimant's mother] gave a history of cystitis and kidney scarring. Whilst this may not constitute a chronic condition, this was not for the midwives to determine as they would not have been able to determine [the Claimant's Mother's] kidney function or the risk during pregnancy of the kidney scarring."
And
"it would be for an obstetrician to determine if she was low risk following a review."
Q I think you accept that the maternal history given at booking of recurrent cystitis and kidney scarring did not constitute a chronic condition?
Her response was
"A. It doesn't absolutely constitute a chronic condition but it doesn't exclude it either."
" .They wouldn't have been able to determine, based on the history that they took, the extent of the scarring or indeed whether there had been any other -- anything else found as a basis for -- as a result of, sorry, the recurrent cystitis."
And:
"They couldn't have known the extent of the scarring and the impact on pregnancy on renal function. So I know that we've discussed risk here this afternoon and risk is a dynamic process. Antenatal booking is a really important process in determining and identifying risk factors, not just risk alone and so, as I've said already, midwives are experts in normality. So kidney scarring is an unusual -- it's not a regular -- it's not a common issue that women are giving in history and so I would have expected a referral to an obstetrician."
"Q. And sometimes there are those grey areas where a consultant opinion may or may not be required?
A. That's right. Yes.
Q. And this is one of those grey areas, isn't it?
A. I disagree. I -- in my view the kidney scarring and not knowing the extent of that kidney scarring or the effect of pregnancy on renal function is something that really mandated a referral to an obstetrician."
"it can be obvious at booking if consultant led care is required. Sometimes a consultant opinion is needed instead because it is not obvious if they need to be involved throughout pregnancy. A midwife can refer for consultant opinion, if it is not clear, and the consultant themselves decide whether they need to take the lead in pregnancy. The history of recurrent cystitis and scarring of the kidneys was from the history as given by [the Claimant's Mother]. She did not give any ongoing history of chronic renal disease. [The Claimant's Mother] was not receiving any medication nor was she under the care of doctors for any kidney issues so midwife Hickman in her statement says that she did not consider that a specific referral for consultant led care was required. As it was, the consultant Ms Hutchon did peruse the records so a consultant was involved with the decision making. Ms Hutchon, like the midwives, felt that [the Claimant's Mother] could be under the auspices of "low risk". Even so as indicated by midwife Hickman in her statement, if a midwife further on in the pregnancy feels that another consultant review is warranted then she would refer again. However, no concerns were evident with the pregnancy until [the Claimant's Mother] was admitted on 3 October 2008. The last routine appointment was on 25 September 2008 and her blood pressure on that day was within a normal range and urinalysis was negative so there were no signs of preeclampsia on that day".
"well it could have been helpful - you know, any face to face discussion could be helpful. But I mean, in this trust it seemed to be the routine that the records were perused by a consultant so - and the midwives knew that, so there was going to be an overview of the records."
The expert nephrology evidence
"we think adult infections have no bearing, generally speaking, in the sense that reflux of urine back up towards the kidney may have ceased and therefore those are just bladder infections with no knock on impact on kidney function."
And that when looking for reflux nephropathy:
"It's the childhood history that you're focusing on because this is something that happens very early on, usually under the age of two years, certainly under the age of five years is the time at which the kidneys are developing and the period of risk."
"It's for the nephrologist to advise what the diagnosis is and what that might portend in pregnancy from the nephrologist's perspective, and it's for the obstetrician to decide what they do with that information in terms of midwife versus obstetrics-led care, in terms of frequency of review, in terms of serial scanning et cetera. That's not my remit."
"[The Claimant's Mother] had no evidence of chronic kidney disease either before or during her pregnancy and index events in 2008. Indeed there remains no evidence of CKD on subsequent follow-ups there has been no evidence of structural renal pathology on repeated imaging. It is presumed that [the Claimant's Mother] has been under the misapprehension that her right lower renal pole is scarred due to the poor quality of the imaging in 1994; this is in fact not the case. It is suggested that subsequent notes recording the presence of renal scarring have all followed from this error."
"If [the Claimant's Mother] had been referred to a nephrologist for evaluation, the recommendation would have been to perform a baseline assessment of blood pressure, urinalysis, urine protein albumin: creatinine ratio, renal function and renal ultrasound. On balance of probability, these would all have been normal and [the Claimant's Mother] would not have required or received further renal input."
"Well, what is striking is that throughout the notes the history of kidney scarring seems to be accepted fact, but in fact we have no evidence of proof of kidney scarring. Now, I don't doubt that this claimant believed that she had kidney scarring, but I believe that was based upon a misinterpretation of the investigations that had been performed."
And
"I believe that you are right that if there is a reported history of scarring, then that should be taken at face value. However, the evidence suggests that the reporting history was incorrect."
"Q. But it is certainly one possibility, and a likely possibility, if you've had childhood repeat cystitis and if the mother were right that she had kidney scarring, then it would be a real possibility, wouldn't it?
A. At that point, without further assessment, yes.
Q. Yes. And while it's a real possibility, you've got to look at these risks as an obstetrician, but that may be a matter for the obstetrician.
A. Yes, that's not for me to say.
Q. Yes. So the real issue in this case, despite your thorough investigation from the notes of what you think might be the actual position and the fact that we don't actually know because we haven't had gold standard testing it, none of that was within the ambit of what the obstetrician knew; what the obstetrician knew was what the mother told her?
A. Indeed.
Q. And so unless there's further investigation, would you agree you've got to act on what you're told until you displace that account?
A. That's perfectly true, yes."
The expert obstetric and fetal medicine evidence
"Unfortunately in this case the significant risk factor of FGR of maternal renal disease was overlooked. The significance of this should have been recognised by the attending midwives or Dr Hutchon. The obstetric team should, on the balance of probabilities, have recognised the significance of the past medical history and should have offered increased fetal surveillance with serial growth scans .If, in the alternative, the previous renal history was not easily accessible, the obstetric team should have made the pragmatic decision to assume the diagnosis of reflux nephropathy (being 'one of the most common renal disorders in women of childbearing age') and/or confirm it with a nephrologist and therefore should have offered serial growth scans due to the known association between reflux nephropathy and FGR. To have dismissed the history without attempting to obtain further information from [the Claimant's Mother's] GP or to have made the reasonable assumption that there was a history of reflux nephropathy (and the obstetric implications thereof) was, in my opinion, a breach of duty."
"I think that it was incumbent upon the obstetric team to investigate that further. I think in the first instance making sure that the patient was seen in the antenatal clinic to then be able to interrogate this further. And it may have been a red herring and it may have been that this was clinically insignificant and things could have stopped there, but they weren't to know that. And we know from the textbook evidence at the time that there was a clear link between reflux nephropathy, even in the presence of normal blood pressure and absence of abnormal renal function, with pre-eclampsia and foetal growth restriction, and so I think to have dismissed that history is of concern.
My view is that the obstetrician would have had a number of choices at that moment. There is the option to recognise the failings of the NHS in 2008 and the inability to get up-to-date information between different arms of the NHS, and therefore to make an assumption that this history sounds like reflux nephropathy, to recognise the clear textbook, widespread used textbook evidence that reflux nephropathy has, in Professor Nelson-Piercy's words, a particular association with foetal growth restriction, and managed accordingly, and that would involve commencing foetal growth scans from 28 weeks' gestation.
The other option would be to contact the GP and to see if the GP was able to give complete information. My understanding of looking at the GP notes is that repeatedly on two or three episodes I think I found the GP has written "renal scarring", but there's no further depth to that. So I'm not entirely sure how much help that would have offered. And allied with that, or
alternatively, to discuss with one's local nephrology team and take their advice about whether or not they think this is significant and you would have been hearing from the nephrology experts about how that would be taken forward."
"I would not be critical of somebody at that point who lumped everything together -- if you forgive me, lumped everything together as a renal condition, and teasing out each individual one I think probably would require going back to the text books to confirm."
"I think there is always a danger of an obstetrician organising a bolt-on test to a fetal anomaly scan, which is focussed on one thing, and who would then be interpreting that? So I don't think that would be the right course to follow. I think that taking advice from the nephrologist on a few options, you know, to say: I've got this lady, this is the history she gives, I was wondering whether or not, I think it would be appropriate. But I think an obstetrician of their own volition themselves organising a bolt-on to the 20-week anomaly scan and who would then interpret it and what the accuracy of that is in detecting reflux nephropathy, because I'm sure that most people would not know what that would be and only a nephrologist would know that answer."
"A. Although there is a definition that we sort of strayed into in our meeting of experts, but I think that she did have renal disease until proven otherwise. We've got her clear history as a child. She's got a clear history of saying that she's got renal scarring and we haven't disproved it or, to my knowledge, we haven't disproven it. I mean, I need to be clear again that I'm not the person who would be able to say if that's been excluded or not radiologically.
Q. So if you were right that any patient who says that they have been told 18 years ago that they have something wrong with them which doesn't feature in their medical records, save by way of apparent reports showing something was clear, at all stages the doctor has to accept the patient's account without looking at the objective evidence?
A. No.
Q. No. It would be illogical to proceed otherwise?
A. It would be totally illogical --
Q. You would have to proceed on the basis of the subjective history, the objective evidence available and your assessment and examination?
A. Exactly, and I think that can only really be done in person with a patient.
Q. And if there had been such an in-person assessment with [the Claimant's Mother] here, and the reasonable obstetrician had been reassured by her and by the information from the general practitioner, it would have been reasonable for that obstetrician to refer her back to the low risk part of it, isn't it?
A. With all the ifs, then yes, I agree."
"Well, I suppose I couldn't say his first option was wrong, which was to just do scans, but I do think that that comes from an environment where access to scans was perhaps different to that in most district general hospitals. So I won't say it would be unreasonable, but I don't think that that would have been, as it were, the approach that I would have taken or most people in the working environment that I was in would have taken.
In terms of the second option, I think that that would have been a sensible thing to ask the GP to highlight any investigations that had been performed, to confirm whether there was any objective evidence of concern and/or whether there'd have been referral to other specialists.
Then the third option, again contacting a nephrologist about negative findings, I think would -- again, I think that's not the environment in which I was working; and in terms of the fourth option I've said that I think that that would have been an acceptable approach."
"I have made my consideration based upon what the witness evidence from the midwife said and from what doctor Hutchon said. And obviously in oral evidence Dr Hutchon expanded on some of the things that she said she would have checked. So my opinion has not changed. I think, if she did those sort of checks that she described, I think she took reasonable precautions to try and identify whether the categorisation was reasonable."
"I did understand that that's what would be his perspective as a nephrologist, but my perspective as an obstetrician would be that if I had someone who had that history but no ongoing review or follow-up, I wouldn't have arranged for her to be seen again in the maternity unit."
"As Dr Hutchon explained, that's why she would this woman would still be having the regular checks of her urine and the regular checks of her blood pressure because that would be looking at the potential consequences."
"Well, those are the problems to look for in any pregnancy and in somebody with kidney scarring, what I would have been thinking about at that time is that they would be at risk of hypertension and proteinuria and those are routinely checked for at every antenatal check. I would not have thought someone with a history of kidney scarring but without any ongoing concerns about their renal function was at higher risk for IUGR, to the degree where I would recommend growth scans rather than surveillance by the routine assessment of growth that was undertaken."
"There's two patients, yes, so if there is a problem with the kidney, then it might be mum's blood pressure would go up and it might be she'd develop pre-eclampsia. It can happen in someone who hasn't got kidney problems and that's the common mistake.
The thing from the foetal point of view, the thing that is probably most significant is the placental development and the maternal kidney doesn't affect the development of the placenta, unless the maternal kidney is compromised at time the placenta's developing, would be my kind of understanding. So in a way growth restriction and its problems are determined from quite early in the pregnancy, when the kidneys are not under particular pressure, which is why I don't think that -- unless you've got kidney problems when you're developing your placenta and getting to 20 weeks, that's why there's not a massive increase in growth restriction in women who've got normal kidney function."
The expert neonatology evidence
(1) The Claimant probably acquired his brain injury in the last week of his intrauterine life i.e. at 32 weeks' gestational age;
(2) Probably delivery of the Claimant should have occurred by 30th September 2008 to 1st October 2008 in order for the brain injury to have been avoided.
The contemporaneous medical literature
"women with more severe renal impairment are at increased risk of adverse pregnancy outcome and complications - especially preeclampsia, IUGR and prematurity (table 10.3)"
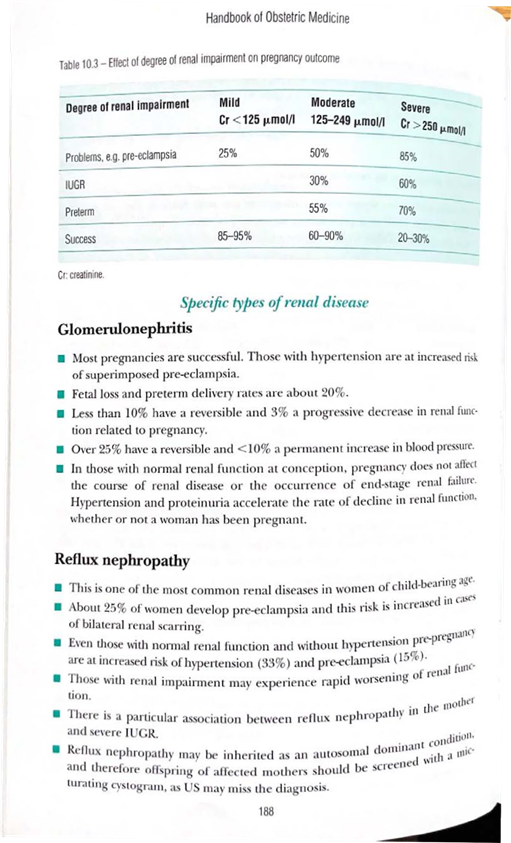
Q. So what is meant by "screening" there?
A. In which bit?
Q. The screening
A. Oh, for pre-eclampsia and for
Q. For the -- what are the steps you'd take for the foetus there?
A. So the -- looking for reflux in a foetus, ultrasound is not particularly good. However, renal pelvis dilatation in the foetus at 20 weeks is a fairly common problem that we see. Often it turns out to be nothing. Sometimes it could be due to obstructions somewhere in the renal tract and other times it could be due to reflux, but we are largely unable to make a definitive diagnosis of that until after birth.
Q. But in terms of during the pregnancy, what would have been the steps taken to monitor the foetus as opposed to the mother?
A. For a growth issue?
Q. Yes.
A. Yes. So there in that circumstance I would suggest growth scans from 28 weeks."
"maternal hypertension, proteinuria, and recurrent urinary tract infection often coexist in women with chronic kidney disease, and it is difficult to tell how much each of these factors contributes to a poor pregnancy outcome. It seems however that each factor is individually and cumulatively detrimental to fetal outcome. Women with severe renal impairment have the greatest difficulty conceiving, the highest rate of miscarriage, and the poorest pregnancy outcome. The degree of renal dysfunction correlates with the risk of a poor pregnancy outcome (table 3)".
Discussion
(1) she had kidney scarring (or the treating obstetrician would have to work on the basis that she had because it could not be excluded during the pregnancy) and this amounted to structural damage to the kidney; and
(2) Dr DuPont was of the view that there were associated health implications i.e. hypertension and pre-eclampsia and IUGR.
"The kidneys undergo marked hemodynamic, renal tubular and endocrine changes during pregnancy. A failure of these adaptations in women with renal disease creates a sub-optimal environment for fetal development and increases the risk of obstetric complications such as preeclampsia, preterm labour, and intrauterine growth restriction [IUGR]"
And
"Pregnancy itself can cause acute renal disease or uncover a previously subclinical renal condition".
"In turn, during pregnancy the diseased maternal kidneys are exposed to the damaging consequences of a prothrombotic state, ascending urinary infections, gestational hypertension, and altered hemodynamics that exacerbate proteinuria. Women with a preconception glomerular filtration rate (GFR) of less than 25 mL/min (serum creatine >177 umol/L; 2.0mg/dL) have a 1:3 chance of pregnancy related decline to end-stage renal failure (ESRF) and are likely to have preterm, growth-restricted babies."
Conclusion
