Freely Available British and Irish Public Legal Information
[Home] [Databases] [World Law] [Multidatabase Search] [Help] [Feedback]
England and Wales High Court (King's Bench Division) Decisions
You are here: BAILII >> Databases >> England and Wales High Court (King's Bench Division) Decisions >> Snow v Royal United Hospitals Bath NHS Foundation Trust [2023] EWHC 42 (KB) (13 January 2023)
URL: http://www.bailii.org/ew/cases/EWHC/KB/2023/42.html
Cite as: [2023] EWHC 42 (KB)
[New search] [Printable PDF version] [Help]
Neutral Citation Number: [2023] EWHC 42 (KB)
Case No: QB2018-000363
IN THE HIGH COURT OF JUSTICE
KING'S BENCH DIVISION
Royal Courts of Justice
Strand, London, WC2A 2LL
Date: 13/01/2023
Before:
HHJ RICHARD ROBERTS
(Sitting as a Judge of the High Court)
- - - - - - - - - - - - - - - - - - - - -
Between:
|
|
Mr Malcolm Richard Snow |
Claimant |
|
|
- and - |
|
|
|
Royal United Hospitals Bath NHS Foundation Trust |
Defendant |
- - - - - - - - - - - - - - - - - - - - -
- - - - - - - - - - - - - - - - - - - - -
Dr Peter Ellis of Counsel (instructed by Slater & Gordon UK Limited) for the Claimant
Mr Charles Feeny of Counsel (instructed by Bevan Brittan LLP) for the Defendant
Hearing dates: 20, 21, 24, 25, 26, 27 October 2022
- - - - - - - - - - - - - - - - - - - - -
Approved Judgment
Introduction
- This is the trial of the Claimant’s claim for damages for clinical negligence for failing to obtain his fully-informed consent for a laparoscopic low anterior resection of rectal cancer with a trans-anal (Ta) total mesorectal excision (TME), and for negligent intra-operative care. The Defendant admits it failed to consent the Claimant adequately but causation is denied. The Defendant denies the Claimant’s allegation of negligent intra-operative care.
- The Claimant says that if he had been adequately consented, he would have chosen to undergo a TME, and not a TaTME, and as a consequence he would not have suffered the following severe multiple injuries:
- Dr Ellis of Counsel appears on behalf of the Claimant and I am grateful for his skeleton argument, dated 18 October 2022, [1] and written closing submissions. Mr Feeny of Counsel appears on behalf of the Defendant and I am grateful for his skeleton argument, dated 18 October 2022, [2] and written closing submissions, dated 27 October 2022.
- There are the following trial files:
- The Claimant served a Civil Evidence Act Notice upon the Defendant on 18 November 2021 in respect of Mr Bilson. The trial was originally due to commence on Monday 17 October and Mr Bilson had made himself available to give his oral evidence on 17, 18 and 19 October. The trial was moved to commence on 20 October 2022 because of a delay in the provision of the colorectal surgeons’ joint statement. Mr Bilson was unable to attend the trial commencing on 20 October 2022 because of a prior business engagement in Canada. The Defendant did not oppose Mr Bilson’s witness statement being admitted in evidence and having regard to the circumstances and the overriding objective, on the first day of the trial I admitted Mr Bilson’s witness statement in evidence.
- At all relevant times, the Royal United Hospital, Combe Park, Bath, Avon (the Hospital) was controlled and managed by the Defendant. The Defendant employed surgical and medical staff to provide medical services pursuant to the National Health Service Act 2006.
- The Claimant was at all relevant times an NHS patient, receiving advice and treatment from the Defendant’s employees or agents at the Hospital. He was aged 56 at the date of surgery and is now aged 63. He is by profession an engineer. Prior to undergoing the TaTME surgery, he had his own business, AMS 1911 Ltd, providing turbo machinery design engineering services to Rolls Royce. Between 1990 and 2015 he had worked on civil and military aero engines, marine propulsion units for the US Navy and land based power generation plants in Derby, Berlin and Bristol, as a permanent employee and on an external contractor basis. He had worked continuously from February 1990 until the operation on 8 December 2015.
- The Claimant relies upon witness statements from:
- The Defendant relies upon witness statements from:
- On 15 September 2015 the Claimant consulted his GP, who noted a two-week history of intermittent rectal bleeding, associated with loose bowel motions. His appetite and weight were normal [10].
- On 22 September 2015 the Claimant was reviewed by his GP, who recorded that there was left iliac fossa abdominal tenderness, a very large liver, and possibly an enlarged spleen. Digital rectal examination revealed only anterior anal fissures. An ultrasound scan of the abdomen and pelvis, and a number of blood tests, were arranged [11].
- On 28 September 2015 the ultrasound scan was reported to show a heterogeneous coarse micronodular appearance in the liver, suggesting liver cirrhosis or possibly cancerous lesions [12]. The blood test results were reviewed by the Claimant’s GP, and noted to show a slightly raised carcinoembryonic antigen (a tumour marker), a slightly raised C reactive protein (a marker of infection and inflammation) and mild abnormalities of liver function. The Claimant was referred to the Defendant for an urgent colorectal surgical assessment [13].
- On 6 October 2015 the Claimant was assessed by Mr Kynaston, specialist registrar to Mr Williamson, in the Defendant’s colorectal clinic [14]. It was recorded that he had a one-month history of change in bowel habit, namely loose stools up to 5 to 10 times per day, associated with the passage of altered blood, abdominal pain, shortness of breath and a cough. On examination it was recorded that his abdomen was soft and non-tender, with obvious hepatomegaly. No low rectal lesions were identified on digital rectal examination and proctoscopy.
- On 15 October 2015 the Claimant underwent a CT scan of the chest, abdomen and pelvis with contrast [15]. This was reported to show a 5cm soft tissue lesion related to the rectum without obvious local extension. There was a 17mm diameter pre-sacral lymph-node inferiorly, further enlarged lymph nodes in the pelvis superiorly up to 22mm in diameter, and smaller upper abdominal lymph nodes. The liver was enlarged and replaced by numerous tiny hypodense lesions. The appearances were suspicious of metastatic disease. The conclusion was bulky mid-rectal tumour with significant pelvic lymphadenopathy, and likely liver metastases.
- On 20 October 2015 the Claimant underwent a colonoscopy at the Defendant’s hospital, which showed a 4cm malignant looking mass in the rectum 10cm from the anal verge [16]. There was a rolled edge with central ulceration. Biopsies were obtained.
- On 3 November 2015 the Claimant underwent an MRI scan of the pelvis and rectum, which showed a 47mm mid/distal rectal polypoid tumour, sited 10.3cm from the anal verge, and 4.6cm from the anorectal junction [17]. There was no convincing extramural venous invasion. The circumferential resection margin was safe. There were multiple enlarged mucin containing mesorectal and superior lymph nodes. The conclusion was mucinous mid/distal rectal tumour, radiological staging T3b N2b Mx, CRM safe, EMVI -ve.
- On 4 November 2015 the Claimant was reviewed by Mr Courtney, a consultant colorectal and general surgeon, at the private Bath Clinic [18]. It was recorded that he was suffering from increasing bleeding and discomfort from the rectal lesion. His case was due to be discussed at the Defendant’s colorectal multidisciplinary team meeting the following day.
- It was noted that the tumour biopsies had shown features which were suspicious but not completely diagnostic of invasive rectal carcinoma. The findings of the CT scan were also noted. The Claimant was advised that he had a bulky mid-rectal tumour with significant pelvic lymphadenopathy, and that he might require pre-operative neoadjuvant radiotherapy due to the enlarged lymph nodes.
- On 5 November 2015, the multidisciplinary team discussed the Claimant’s case at their meeting. It was noted [19],
- Mr Courtney telephoned the Claimant on 5 November 2015, after the multidisciplinary team meeting. The Claimant says in his witness statement at paragraph 15 [20],
- Mr Courtney wrote a letter dated 5 November 2015 to the Claimant’s GP following the Claimant’s consultation on 4 November and the telephone conversation with him on 5 November 2015. In the letter he said [21],
- On 11 and 18 November 2015 the Claimant was assessed by Dr de Winton at the Bath Clinic [22]. It was decided that he would receive a short course of neoadjuvant radiotherapy in order to reduce the risk of loco-regional recurrence before definitive radical surgery and he was referred to the hepato-biliary surgical team at Bristol Royal Infirmary for further advice. An MRI of the Claimant’s liver was carried out on 13 November 2015 [23].
- On 20 November 2015 the Claimant’s case was discussed in the hepato-biliary surgical multidisciplinary meeting at Bristol Royal Infirmary [24] and subsequently with Dr de Winton [25]. Although a definitive radiological diagnosis could not be made, the radiology opinion was that the changes in the liver and possibly in the pancreas did not look like typical disease either from rectal cancer or from any neuroendocrine tumour.
- Between 30 November 2015 and 4 December 2015 the Claimant received a short course of radiotherapy in the form of 25 Gy in 5 fractions.
- On 3 December 2015 the Claimant underwent a pre-operative nursing assessment at the Defendant’s hospital [26].
- On 4 December 2015 the Claimant’s case was discussed again in the hepato- biliary multidisciplinary meeting at Bristol Royal Infirmary [27]. The advice was for the bowel malignancy to be treated radically first, with a liver biopsy to be obtained at the same time.
- On 8 December 2015 the Claimant was admitted to the Defendant’s hospital, where he underwent a TaTME procedure. The operation, which lasted for approximately 8½ - 9 hours [28], was performed by Mr Dalton, Mr Courtney and Mr James. On the morning of the operation, Mr Courtney obtained a written consent [29] from the Claimant for a laparoscopic low anterior resection of the rectal cancer, with a transanal total mesorectal excision, a loop ileostomy and liver biopsy. It was recorded that the serious or frequently occurring risks were bleeding, wound infection, deep vein thrombosis, pulmonary emboli, sepsis, chest infection, anastomotic leak, bile leak and splenectomy.
- On 14 December 2015 the Claimant was discharged [30].
- The histopathology report was noted to show a rectal mucinous adenocarcinoma measuring 50mm in maximum diameter [31]. The resection appeared complete. There were 6 positive lymph nodes out of 30 sampled. The diagnosis was invasive adenocarcinoma with lymph-node metastases, staging pT3 N2, Duke’s C1. The liver biopsy was noted to show biliary hamartoma with no evidence of malignancy.
- On 16 December 2015 the Claimant was assessed by Mr Phull, a consultant urologist, by telephone. He noted that the Claimant had failed an early trial without urinary catheter. He advised a further attempt as an inpatient on 18-19 December 2015. He noted [32],
- On 23 December 2015 the Claimant was reviewed by Dr de Winton at the Bath Clinic [33]. It was recorded that although his indwelling urinary catheter had been removed, he was still needing to use intermittent self-catheterisation to pass urine. He was advised to consider adjuvant chemotherapy using the FOLFOX regimen, however, this would be delayed until his bladder function had improved.
- On 23 December 2015 the Claimant was also reviewed by Mr Phull at the Bath Clinic [34]. It was recorded that he was performing intermittent self-catheterisation two to three times a day with good residual volumes of 600 to 750ml. He was noticing increased bladder sensation. The Claimant was advised that it was too early to know what the long-term functional outcome would be.
- On 23 December 2015 the Claimant was also reviewed by Mr Courtney at the Bath Clinic [35]. It was recorded that he had perianal soreness. However, the port site wounds and extraction wound had healed, and the ileostomy appeared healthy. He was advised that the mesorectum was very adherent to the pelvic sidewall, particularly on the left, due to fibrosis from involved lymph nodes in that area.
- On 6 January 2016 the Claimant was reviewed by Mr Courtney and Dr de Winton at the Bath Clinic [36]. It was recorded that he was passing anal mucus and occasional blood on a daily basis, and perianal pain was disturbing his sleep. On digital rectal examination it was recorded that there was no suggestion of infection, and the anastomosis felt intact. The FOLFOX chemotherapy was postponed as he did not feel well enough to undergo it.
- On 20 January 2016 the Claimant was reviewed by Mr Courtney at the Bath Clinic [37]. It was recorded that his symptoms of anal bleeding were getting worse. Digital rectal examination was normal, but a rigid sigmoidoscopy was noted to show a very inflamed low colonic mucosa at the site of the anastomosis. An oral antibiotic was prescribed.
- On 27 January 2016, the Claimant’s GP noted [38],
- On 1 February 2016 the Claimant underwent a colonoscopy performed by Mr Courtney at the Bath Clinic, due to significant diarrhoea, rectal bleeding and tenesmus [39]. This was noted to show a healed anastomosis, but very severe colitis throughout the colon. The working diagnosis was severe diversion colitis. The plan was to consider reversing the ileostomy.
- On 7 February 2016 the Claimant was readmitted to the Hospital for reversal of the ileostomy [40]. He was discharged on 11 February 2016.
- On 24 February 2016 the Claimant was reviewed by Mr Courtney at the Bath clinic [41]. It was recorded that he was passing less blood and mucus, although some tenesmus and urgency remained. A flexible sigmoidoscopy was noted to show much improved colitis.
- On 8 March 2016 the Claimant commenced FOLFOX chemotherapy.
- On 23 March 2016 the Claimant was reviewed by Mr Courtney at the Bath Clinic [42]. It was recorded that he was having symptoms compatible with low anterior resection syndrome (LARS), namely clustering of stools, urgency and frequency of bowel motions, and anal pain. He was advised to commence Imodium therapy, titrating the dose according to symptoms, and to commence a low fibre diet, with Fybogel as a bulking agent.
- On 26 April 2016 the Claimant’s GP noted [43],
- On 18 May 2016 the Claimant was reviewed by Mr Courtney at the Bath Clinic [44]. It was recorded that he was requiring 8 loperamide tablets a day to manage his LARS. Although his bladder was emptying more completely, it was also noted that he was suffering from impotence, implying damage to the nervi erigentes due to the closeness of the resection margin on the left. He was referred for pelvic floor physiotherapy.
- On 14 July 2016 the Claimant was assessed by Mr Antoniou, a consultant surgeon at St Mark’s Hospital, Harrow, Middlesex, for a second opinion [45]. It was recorded that he was suffering from clustering of bowel evacuation, passing large volumes of stool over a period of approximately 12 hours. He needed to wake at night to open his bowels. A flexible sigmoidoscopy and pelvic MRI scan were advised. He was referred to Dr Wilson at St Mark’s Hospital.
- On 20 September 2016 the Claimant was assessed by Dr Wilson at St Mark’s Hospital [46]. It was noted that the MRI scan and flexible sigmoidoscopy were normal. In spite of loperamide therapy, he was still opening his bowel 6 to 10 times per day, over about 12 hours, with pellet like stools. Manipulation of his diet and additional Fybogel had not helped. He was unable to work. He was advised that good defaecatory technique and regular timings were important, as well as pelvic floor exercises. He was also advised to consult a biofeedback specialist.
- On 3 October 2016 the Claimant was assessed by Mr Hellawell, a consultant urological surgeon at the London Clinic, for a second opinion [47]. It was recorded that he had erectile dysfunction since the rectal surgery, and this had not responded to sildenafil therapy. He was advised that this was due to nerve damage associated with the surgery, and there was a risk it would not fully recover. He was advised to consider prostaglandin injections or a vacuum pump device.
- On 15 December 2016 Mr Hellawell prescribed Alprostadil and noted [48],
- On 15 December 2016 the Claimant’s GP prescribed Caverject [49].
- On 14 January 2017 a trial of Caverject and training was given.
- On 17 January 2017 a testosterone injection was administered [50].
- On 12 April 2017 Mr Speakman, Consultant Urological Surgeon, noted “he has had some success himself” with Caverject “but also quite a few failures”. He noted [51],
- On 17 July 2017 Mr Antoniou, Consultant Colorectal Surgeon, noted [52],
- On 20 September 2017 Mr Speakman, Consultant Urological Surgeon, noted [53],
- On 27 November 2017 the Claimant underwent excision of a metastatic liver nodule, performed by Mr Rees, a consultant hepatobiliary surgeon, at North Hampshire Hospital, Basingstoke [54]. It was noted that there were extensive benign biliary hamartomas, consistent with the previous liver biopsy result.
- In December 2017 the Claimant received a further course of FOLFOX chemotherapy. The oxaliplatin component was discontinued as the Claimant had grade 1 neuropathy. Chemotherapy continued with 5FU [55].
- On 23 February 2018 the Claimant was reviewed by Mr Rees [56]. It was noted that a CT scan of the chest, abdomen and pelvis had shown no abnormalities, and his CEA (carcinoembryonic antigen) remained <1. The benign neuroendocrine tumour at the head of the pancreas remained stable.
- In 1982 Heald et al introduced the technique of total mesorectal excision (TME) as the leading surgical principle to be addressed during rectal cancer surgery [57]. A TME is traditionally performed as a laparotomy (open procedure) or laparoscopic procedure. A transanal approach from below, TaTME, has evolved over recent years. TaTME is explained in the NICE (National Institute for Health and Care Excellence) “Interventional Procedures Guidance on transanal total mesorectal excision of the rectum”, published in March 2015, as follows [58],
- In “Transanal Total Mesorectal Excision: Why, When, and How” (Penna et al, 2017) it is said [60],
- In the joint statement of the colorectal surgeons, Mr Jenkins says that the 2015 NICE guidance on ‘Transanal total mesorectal excision of the rectum’, published 27 March 2015, “would have been based on the scientific literature on TaTME available to date” [61]. The NICE guidance says under “1. Recommendations” [62],
- In the NICE guidance ‘Transanal total mesorectal excision of the rectum, information for the public’, published 27 March 2015, it is stated under the heading:
- In 2020, the Association of Coloproctology of Great Britain and Ireland (the ACPGBI) published a paper entitled “The ACPGBI recommends pause for reflection on transanal total mesorectal excision”. In the paper it says [66],
- The paper makes the following recommendations [67],
- On 15 December 2021, NICE published guidance entitled “Transanal total mesorectal excision for rectal cancer, Information for the public”, saying [68],
- In NICE guidance “Transanal total mesorectal excision for rectal cancer, interventional procedures guidance”, dated 15 December 2021, it is said [69],
- The Defendant admits that, in breach of its duty of care, it failed to consent the Claimant fully. In the amended Defence, dated 8 August 2022, it is said at paragraph 3 [70],
- In addition by email dated 10 January 2020 from NHS Resolution on behalf of the Defendant they admitted breach of duty in the following terms [71]:
- However, the Claimant’s case is that the Defendant’s failure to consent him goes far beyond the Defendant’s admissions. The Claimant says that the Defendant should have:
- In respect of the consenting process, factual and medical causation are both in dispute. Further, there is an allegation of intra-operative negligence. As a consequence, despite the Defendant’s admission that it failed to consent the Claimant adequately, I find that it is necessary to consider the procedure for introducing TaTME procedures at the Hospital (including training, mentoring, supervision and patient selection) and the consenting of the Claimant.
- Whilst I bear in mind that failing to follow NICE guidance is not prima facie evidence of negligence, there would need to be an explanation for not following NICE’s guidance. In Price v Cwm Taf University Health Board [2019] PIQR P14, Birss J (as he then was) said at P22,
- The NICE guidance ‘Transanal total mesorectal excision of the rectum’, published 27 March 2015 says under “1. Recommendations” [73],
- Whilst I acknowledge that the Defendant admitted that it was negligent in the consenting of the Claimant for a TaTME, the Defendant has not disclosed documentation showing that special arrangements for clinical governance, consent and audit or research were put in place prior to the Claimant’s operation on 8 December 2015.
- The Defendant has disclosed a document entitled, “Process for the introduction of new interventional or diagnostic procedures”, dated November 2014 [74]. As is said in the introduction to this document, it “provides a standard framework for the Divisional Boards to manage the introduction of a new interventional or diagnostic procedures” [75]. In the document it is said for example at Paragraph 3, Responsibilities [76]:
- The Defendant has not disclosed any documentation evidencing special arrangements for clinical governance, consent and audit or research, as recommended by NICE, or any standard framework, as required by the Defendant’s own process for the introduction of new interventional or diagnostic procedures. In particular, there are no documents from the Defendant showing:
- There is no reference in Mr Courtney’s witness statements to special arrangements for clinical governance, consent and audit or research being put in place prior to the Claimant’s operation.
- In his closing submissions, Mr Feeny disputed that there were no governance documents, because he said there was reference to them in a Minute from June 2016. There is a Minute of a meeting on 15 June 2016 [77], when Mr Dalton gave a presentation on TaTME. It states that ten TaTMEs have taken place since November 2015 and the plan is to carry out approximately two a month. It was agreed to review again after fifty cases. The Minute says,
- I find that the Defendant’s Minute of 15 June 2016 does not annex any documentation relating to governance procedures. It only refers to a TaTME registry. Mr Feeny said that the governance documents had been lost but the Defendant did not disclose any witness statements or documents referring to governance documents being lost.
- Initially, Mr Feeny said that it was not proportionate to disclose documents relating to governance procedures because the Defendant had admitted that the Claimant had not been properly consented. This position subsequently changed to being that there were documents relating to governance and procedures for implementing TaTME at the Hospital but they had all been lost. I find this unconvincing. In the absence of any witness statement or documentary evidence from the Defendant that it put in place special arrangements for the introduction of TaTME at the Hospital, I am unable to accept that all of the documents have been lost as this is implausible. There would be documents relating to approval from the local ethics committee or the local clinical governance committee. Furthermore, my findings below strongly suggest that there was a systemic failure by the Defendant to put in place special arrangements for the introduction of TaTME.
- The Royal College of Surgeons of England provided guidance for the introduction of new surgical techniques in their document “Good Surgical Practice”, published on 29 August 2014 [78]. It is stated:
- Mr Courtney says in his first statement, dated 31 October 2020, at paragraph 4,
- Mr Courtney does not provide any details of the date of the course, its duration or the course contents. He has not provided a certificate certifying his attendance and successful completion of the course. In cross-examination he said he received a certificate but no certificate has been disclosed.
- The operation was carried out by Mr Dalton with Mr Courtney. No documentation was disclosed as to Mr Dalton’s training and there is no witness statement from him.
- In cross-examination, the Defendant’s colorectal expert, Mr Meleagros, sought to argue that the need for training, mentoring and supervision of TaTME procedures was not identified until 2018 [79]:
- Mr Meleagros sought to characterise the paper “St. Gallen consensus on safe implementation of transanal total mesorectal excision”, published 12 December 2017, which makes a strong recommendation for proper training and proctoring of the first cases [80] as a “watershed moment” [81], despite the fact that he said he had only read this paper for the first time during the trial.
- I reject Mr Meleagros’ evidence and find that the need for training, mentoring and supervision before introducing new surgical operations and procedures was known prior to 2015. I accept Dr Ellis’s submission that [82], “This is all common sense and it’s what your Royal College always promulgates with any new procedures”. The Royal College of Surgeons of England stated in its “Good Surgical Practice”, published on 29 August 2014 and referred to in paragraph 78 above, that the introduction of new surgical operations and procedures should be underpinned by training, mentorship and assessment for all clinical staff. I find that Mr Meleagros was “flying a kite” because training, supervision and mentoring were not referred to in the NICE documents. His argument was unsustainable and damaged his credibility.
- It is common ground that the Defendant did not provide Mr Courtney and Mr Dalton with a mentor. No documentation from the Defendant relating to mentoring has been provided saying that they were provided with a mentor. When asked about this in cross-examination, Mr Courtney suggested that in the present case he did not need one [83].
- I find that the Defendant was negligent in failing to provide a mentor for Mr Courtney and Mr Dalton. Further, it is concerning that far from acknowledging that a mentor was necessary, Mr Courtney suggested that in his case, one was unnecessary.
- In the St Gallen consensus statement, it is said [84],
- It is common ground that Mr Courtney and Mr Dalton were only carrying out their second TaTME but there was no supervision.
- When Mr Courtney was asked about supervision, he again gave the impression that he considered it unnecessary because he and Mr Dalton had been on a training course [85]:
- I find that the Defendant was negligent in failing to provide supervision during the Claimant’s TaTME on 8 December 2015. Again, it is also concerning that Mr Courtney did not consider supervision to be necessary.
- The 2015 NICE interventional procedures guidance states [86],
- Mr Courtney admitted in cross-examination [87],
- None of Mr Courtney’s three witness statements refer to the NICE 2015 guidance at all. He does not acknowledge in his witness statements that patient selection should have been explicitly documented.
- I find that it is informative to consider Mr Courtney’s response when he was asked if he agreed that his failure to document the Claimant’s selection for a TaTME was a breach of the NICE guidance. He replied [88],
- Mr Courtney failed to answer the question. He said, in a similar vein in the way in which he answered questions about his lack of a mentor or supervision during the Claimant’s operation on 8 December 2015, that the failure to document the Claimant’s selection was of no significance because a TaTME was only an extension of a TME operation. I find that a written record of patient selection was required, not least because, as stated in the 2015 NICE interventional procedures guidance [89],
- The Claimant’s expert colorectal surgeon, Mr Jenkins, says in the joint statement [90],
- There was a multidisciplinary team meeting (MDT) on 5 November 2015 [91].
- The Defendant’s colorectal expert, Mr Meleagros, admits that [92],
- I find that the Defendant’s record of the MDT is negligent and substandard in very material respects:
- Mr Courtney consented the Claimant on the day of the operation, namely 8 December 2015, and the Claimant signed a consent form [93].
- The Defendant accepted that it was sub-standard to consent a patient on the day of the operation. Mr Courtney said in cross-examination [94],
- Mr Meleagros was asked if he would accept that anything a patient was told and signed on the day of surgery does not constitute informed consent. He answered [95],
- Further, I accept Mr Jenkins’ evidence that the operation on 8 December 2015 should have been cancelled to enable the Claimant to be properly consented, bearing in mind that NICE had stated that special governance should be in place for TaTME and extra care taken in the consenting process as a consequence of the lack of evidence as to the efficacy and safety of the procedure.
- In cross-examination, it was put to Mr Jenkins that even though the Claimant was not properly consented, the operation had to proceed because there was a whole team ready to go [96]:
- I find that Mr Courtney’s consenting on the day of the operation was not merely negligent and sub-standard, but was entirely consistent with his total disregard for the need for clinical governance, training, mentoring, supervision, documentation of patient selection and an adequate MDT note.
- The 2015 NICE Interventional Procedures Guidance identify in Section 5 [97] seven risks of a transanal total mesorectal excision:
- To summarise, Mr Courtney accepted that the Claimant was not informed of six out of seven material risks identified by NICE. He accepted that his consenting process was sub-standard and not in accordance with the GMC guidance [105]. I accept Dr Ellis’s submission that it is difficult to see how advising the Claimant of the other six risks identified by NICE would have taken more than a few minutes.
- Mr Meleagros, like Mr Courtney, sought to downplay the NICE guidance. In his expert report he says, when considering the consenting process [106],
- In contrast, Mr Jenkins says in his report, dated February 2022 [107],
- I prefer the evidence of Mr Jenkins to that of Mr Meleagros because it is consistent with the guidance from NICE and medical literature. Mr Meleagros accepted that the NICE guidance should have been given to the Claimant. To the extent that he did not agree with the NICE guidance, he provided no or no adequate explanation for it not being applicable in the present case. I find that if Mr Courtney had followed Mr Meleagros’ advice and highlighted the advantages of TaTME, he would have gone wrong because:
- I find that the negligent failure to consent goes far beyond the Defendant’s admission at paragraph 3 of the amended Defence and the Defendant’s email of 10 January 2020 [110]. I find that as part of the consenting process, the Claimant should have been:
- I find it deeply concerning that when Mr Courtney says in his first witness statement, dated 31 October 2020 (almost five years after the index operation), at paragraph 10 [117] what he would have said or done if he had consented Mr Snow in the pre-operative clinic on 11 November 2015, he fails to mention:
- Mr Courtney says [119],
- I find that the Defendant has not provided any adequate explanation for its serial failures to follow the NICE guidance. What Mr Courtney says at paragraph 10 of his witness statement in October 2020 shows that if he had consented the Claimant on 11 November 2015, this consenting would have again been negligent.
- Mr Courtney and Mr Dalton’s operation note, which is extremely brief, recorded [120]:
- In cross-examination, Mr Courtney accepted that the operation note was inadequate for governance purposes, research and investigation [121]:
- Mr Jenkins says in his liability and causation report, dated February 2022, of the operation note [122],
- Mr Meleagros says in his condition and prognosis report, dated 9 July 2022 [123],
- I find that the evidence in this case is all one way: that the note of an operation which lasted nearly nine hours is negligent, as was the consent form and the note of the MDT. It is of concern that Mr Courtney provides no explanation for why the operation note was completed negligently.
- In his closing submissions, Mr Feeny submitted that the multiple failures to follow the NICE guidance in relation to consenting the Claimant and recording the selection process for a TaTME, and the inadequacy of the MDT meeting and the operation record, was a matter of form-filling. He submitted [124],
- I find that the Defendant’s multiple failures to follow and properly document the correct procedure it is not mere form filling but has led to the very serious negligent or sub-standard care which the Claimant has received. It was inappropriate to trivialise it by suggesting it is form filling.
- The Claimant’s case on factual causation is that if he had been properly consented by the Defendant, he would not have undergone a TaTME but a TME laparoscopically with autonomic nerve preservation.
- The Claimant says in his witness statement, dated 18 November 2021, at paragraph 45 [125],
- In her witness statement, dated 18 November 2021, Helen Snow says at paragraph 26 [126],
- Mr Jenkins says in his liability and causation report, dated February 2022 [127],
- The Defendant’s counter-factual case is summarised by Mr Feeny in his skeleton argument at paragraph 5(e) [128]:
- The Defendant’s case is supported by Mr Meleagros in his liability and causation report, dated 30 March 2022 [129],
- In his skeleton argument, dated 18 October 2022, Mr Feeny says at paragraph 2, under the heading, “Issues of Fact” [130],
- In his written outline closing submissions, Mr Feeny says at paragraph 1 that there are only two factual issues to resolve:
- In my judgment, the three issues raised by Mr Feeny in his skeleton argument need to be resolved. They include whether Mr Courtney told the Claimant to cancel the appointment for 10 November 2015 but are not limited to this one question. I find that the issue as to whether Mr Courtney and Mr Dalton at any stage were operating in the wrong plane is not a factual issue, but a medical issue, and I will address this when considering medical causation.
- A conspicuous feature of Mr Courtney’s evidence is that in his three witness statements, he makes no reference at all to:
- I find that Mr Courtney failed to follow the 2015 NICE interventional procedures guidance [131] in multiple respects:
- In his second witness statement, dated 24 October 2021, Mr Courtney says at paragraph 6 [138],
- I find that this is another example of Mr Courtney seeking to downplay the risks of TaTME. Conspicuously:
- I find that Mr Courtney’s disregard for the NICE guidance without any adequate reasons and also his misrepresentation of the NICE guidelines seriously undermine his credibility as a reliable witness. In cross-examination, I found him to be an evasive and unreliable witness for the reasons set out above. Save where his evidence is confirmed by independent evidence, I must approach it with caution.
- I found the Claimant to be a credible and reliable witness. His witness statement is internally consistent and consistent with the documentary evidence. He gave his evidence in a balanced and thoughtful manner. He made concessions contrary to his financial interests, for example saying that he had not decided whether to undergo penile implants (see paragraph 463 below).
- In his skeleton argument, Mr Feeny alleged at paragraph 2 b) [141],
- I find that there was no basis for this allegation. To the contrary, I found that the Claimant gave his evidence in a balanced and reasonable manner without displaying animosity towards Mr Courtney.
- Mr Courtney sets out his account of the Claimant’s consultation with him on 4 November 2015 at paragraph 7 of his witness statement, dated 31 October 2020 [142]. He says that:
- However, in a letter dated 5 November 2015 to the Claimant’s General Practitioner, Mr Courtney says under the heading “Clinic Date: 4 November 2015” [143],
- In cross-examination, Mr Courtney had to accept that his statement that he had not seen a CT scan at the time of the consultation on 4 November 2015 was not correct [144]:
- The Claimant says the consultation with Mr Courtney on 4 November 2015 lasted about twenty minutes. In his witness statement he says [145],
- In cross-examination the Claimant:
- I prefer the Claimant’s account of the consultation on 4 November 2015 at the BMI Bath Clinic because it is internally consistent and consistent with the documentary evidence. In contrast, Mr Courtney’s account that he had not seen the CT scan was, as he admitted in cross-examination, untrue and contradicted by his letter to the Claimant’s GP, dated 5 November 2015.
- I reject Mr Courtney’s contention that the Claimant was shouting at the consultation on 4 November 2015. There is no contemporaneous record of this alleged behaviour and there is no suggestion of it in the letter to the Claimant’s GP on 5 November 2015. It was first alleged in Mr Courtney’s first witness statement, dated 31 October 2020, five years later. I bear in mind that Mr Courtney accepted in cross-examination that he sees thirty to forty patients in clinic a week, and that remembering a consultation seven years ago is difficult.
- I accept the Claimant’s evidence that he did not tell Mr Courtney that he was not prepared to accept a permanent stoma and that this was not discussed because Mr Courtney told him that he would need a temporary stoma and a bag for a few months but it would then be reversed.
- I accept the Claimant’s evidence in cross-examination that he had the impression that Mr Courtney would only remove part of the rectum rather than Mr Courtney actually saying this. This was entirely consistent with his witness statement, dated 18 November 2021, where he says at paragraph 9, “I was absolutely convinced that I was having a partial removal of my rectum” [150]. I accept Dr Ellis’s submission that this was understandable because the Claimant was never adequately consented. The Claimant says and I accept that he was not aware that he was going to undergo a TaTME and did not know this until after the operation. He says in his witness statement [151],
- In his witness statement, dated 31 October 2020, Mr Courtney refers at paragraph 8 to the telephone call he had with the Claimant on 5 November 2015 [152]. He says that he told the Claimant that he had rectal cancer and that the oncologists recommended a short course of radiotherapy prior to surgery. He says,
- I note that Mr Courtney does not say that he advised the Claimant that a TaTME would be the best surgical procedure and that the Claimant agreed to undergo a TaTME.
- In his third witness statement, dated 5 August 2022 (nearly seven years after 5 November 2015), Mr Courtney gives a very different account of the telephone conversation on 5 November 2015. He says [153],
- In his witness statement, dated 18 November 2021, the Claimant says [154],
- The Claimant’s diary entry for 10 November 2015 says of the appointment with Mr Courtney [155],
- The Claimant was asked in cross-examination [156],
- Mr Courtney says in his third witness statement, dated 5 August 2022, that he explained to the Claimant that because of his BMI and narrow male pelvis, he would use a new technique called a transanal total mesorectal excision, in which he and Mr Dalton had been trained. I prefer the Claimant’s account of the telephone conversation on 5 November 2015 to that of Mr Courtney for the following reasons:
- Mr Feeny submits that it is notable that the suggestion that Mr Courtney told the Claimant to cancel the appointment was only made after the Defendant had served a Part 18 request, dated 29 October 2020 [163]. However, I find that it is not surprising because by an email dated 10 January 2020 from NHS Resolution on behalf of the Defendant, it admitted that the Defendant failed to consent the Claimant prior to undergoing the TaTME surgery [164].
- Further, I accept the Claimant’s evidence that Mr Courtney told him that he need not attend the appointment on 10 November 2015 for the following reasons:
- In the amended Defence, it is said at paragraph 5 that even if the Claimant had been properly consented, he would have undergone a TaTME on 8 December 2015 because [165],
- Mr Feeny submits as part of the Defendant’s counter-factual argument on causation that the Claimant was so anxious to receive treatment urgently that he would have consented to the carrying out of a TaTME on 8 December 2015 even if he had been fully consented that day. Mr Feeny refers to the following:
- In cross-examination, it was put to Dr Jenkins that there were time targets for the time between radiotherapy being completed and surgery [168]:
- In cross-examination, the Defendant’s witness, Dr Emma de Winton, Consultant Clinical Oncologist, accepted that if there had been three weeks’ delay after 8 December 2015 in carrying out the operation, it would not have affected the staging and management of the Claimant’s cancer [169].
- Whilst the Claimant naturally wanted to have surgery urgently, I accept his evidence at paragraph 45 of his witness statement, dated 18 November 2021, (see paragraph 123 above) that if he had been adequately consented, he would have refused to undergo a TaTME and would have undergone a conventional laparoscopic TME. If Mr Courtney had not cancelled the appointment on 10 November 2015 and had adequately consented the Claimant on that day, there would have been no reason why the Claimant could not have undergone a laparoscopic TME on 8 December 2015. Even if the operation on 8 December 2015 had had to be put back for three weeks, on the evidence of Dr Jenkins and Dr de Winton, this would not have affected the staging and management of the Claimant’s cancer and therefore would not have prevented the Claimant from undergoing a laparoscopic TME.
- In his outline closing submissions, dated 27 October 2022, Mr Feeny submits at paragraph 5,
- As to (a) above, Mr Courtney and Mr Meleagros agreed that it is substandard to consent a patient on the day of the operation. The Defendant therefore clearly cannot rely upon the Claimant not thinking clearly and rationally on the day of the operation. As to (b), and the Claimant’s desire to have treatment as soon as possible, I have found at paragraph 161 above that there is no merit in this argument. As to (c), I accept the Claimant’s evidence that if he had been properly advised in accordance with the NICE guidance, he would have undergone a laparoscopic TME. As to (d), the Defendant cannot rely on the Claimant’s trust in Mr Courtney when it admits that Mr Courtney’s consenting of the Claimant on the day of the operation was negligent. Furthermore, I have found that Mr Courtney’s statement at paragraph 10 of his first witness statement, dated 31 October 2020 [170], as to how he would have consented the Claimant on 11 November 2015 shows that his consenting would have been negligent even if he had had an appointment with the Claimant on that date.
- I conclude that I found the Claimant to be a truthful witness and find that he has proved on the balance of probabilities that if he had been properly consented, he would have elected to undergo a laparoscopic TME, either on 8 December 2015 or shortly thereafter.
- The Claimant relies upon the following expert medical evidence:
- The Defendant relies upon the following expert medical evidence:
- The parties rely upon the following joint expert statements:
- All of the experts apart from the consultant psychiatrists gave oral evidence before the Court.
- In C v North Cumbria University Hospitals NHS Trust [2014] EWHC 61 Green J (as he then was) said at paragraph 25 (vii):
- I found Mr Jenkins to be a thoughtful and reliable witness who did not overstate the position and made all appropriate concessions. For example, Mr Jenkins contends that the Claimant’s LARS is more severe as a result of having undergone the TaTME. However, when cross-examined about whether this increased severity led to a difference in the Claimant’s quality of life, he said [189]:
- I have found Mr Meleagros to lack the independence required of an expert and to be unreliable:
- Mr Meleagros says in his liability and causation report, dated 30 March 2022 [190],
- It is clear and well-established procedural law [192] that experts provide a list of published literature and only provide copies of unpublished literature. Mr Jenkins annexed a list [193] of medical literature to his report dated February 2022, which included 17 papers. In addition the agenda for Mr Meleagros and Mr Jenkins for their joint discussion said on the first page,
- It transpired at trial that despite this Mr Meleagros had not read three of the papers, one of which, the St Gallen paper, he himself described as a seminal paper once he had read it during the trial. When asked why he had not read three of the papers when he was questioned about them, he repeatedly said that none of them were provided to him [194]:
- Mr Meleagros’ answer displayed a misunderstanding of his duties as an expert to obtain copies of published medical literature himself.
- Mr Meleagros frequently did not answer the question [195]. By way of example:
- When challenged as to errors in his report, he frequently sought to defend them before admitting that he was in error. For example, he was referred to his answer to the first question in the joint statement, where he says [196],
- I found Mr Jenkins a more credible and reliable witness than Mr Meleagros.
- I will consider medical causation by considering the following:
- Mr Jenkins says in his liability and causation report, dated February 2022, at paragraph 16 [198],
- In the joint statement of Mr Meleagros and Mr Jenkins, dated 20 October 2022, Mr Jenkins says [199],
- In cross-examination, Mr Meleagros said in reply to questioning about whether the cancer was mid-rectal or low-rectal [200],
- Mr Meleagros’ agreement in the joint statement and in cross-examination that, “A TME should have been carried out in any event regardless of the precise definition of whether it was low or mid low or mid” is directly contrary to his evidence in his liability and causation report, dated 30 March 2022, where he says, “The only option, if TaTME was to be avoided, was APER” [201].
- I conclude that it is common ground that the Claimant was a suitable candidate for a TME. I accept Mr Jenkins’ evidence that a TME was the most suitable surgical option.
- The Claimant’s case is that his tumour was located mid-rectum. The Defendant’s case is that the Claimant had a low-rectal cancer. Contrary to Mr Meleagros’ evidence that the location is not important, I find that the medical literature shows that it is important because the lower the cancer in the rectum, the greater the likelihood of functional complications.
- The CT scan on 15 October 2015 demonstrated a 5cm lesion in the rectum as “bulky, mid rectal tumour” [202].
- The MRI scan on 3 November 2015 reported “47mm mid/distal rectal polypoid tumour. The inferior edge was situated 10.3cm from the anal verge and 4.6cm from the anorectal junction”. The conclusion of the report states “mucinous mid/distal rectal tumour” [203].
- In Mr Courtney’s letter to the Claimant’s General Practitioner dated 5 November 2015, he says [204],
- Mr Courtney contradicts this in his first witness statement, dated 31 October 2020, where he says at paragraph 10 [205],
- It is common ground that the identification of the location of the tumour falls within the expertise of the parties’ consultant radiologists, Dr Burling and Dr Scullion. They agree that the Claimant’s tumour was mid-rectal:
- Mr Jenkins’ position has been from the outset that the tumour was mid-rectal. Mr Meleagros’ position in the joint statement was that the tumour was mid/low rectal. In the joint statement of the colorectal experts, dated 20 October 2022, it is said,
- In cross-examination, Mr Meleagros sought to challenge the radiologists’ agreement in their joint statement, saying that there were multiple points from which the tumour could be measured, which would determine its location [210]:
- Mr Meleagros went on to say [211],
- I make the following findings:
- I accept the evidence of the radiologists that the Claimant’s tumour was mid-rectal.
- I find that Mr Meleagros’ attempt to undermine the agreement of the radiologists that the tumour was mid-rectal was without foundation and another example of him seeking to “fly a kite”. It was, as he conceded, outside his expertise. Mr Meleagros quoted no authority for his scattergun approach to determining the location of the tumour. When pressed by Dr Ellis, Mr Meleagros fell back on saying that the location made no difference because a TME should have been carried out regardless.
- In the amended Defence, it is alleged at paragraph 5(iii) [213],
- Mr Jenkins says in his liability and causation report, dated February 2022 [214],
- In the joint statement of the colorectal experts, dated 20 October 2022, Mr Jenkins says [215],
- Mr Meleagros says in his liability and causation report, dated 30 March 2022 [216],
- In cross-examination, Mr Meleagros admitted that it was not his opinion that carrying out a TME would on the balance of probabilities have resulted in the need to convert to an APER. He agreed that if the Claimant had undergone a TME, there would have been a less than 50% risk of the operation having to be converted to an APER and colostomy [217]:
- I find that the argument that the Claimant would not have chosen to undergo a TME because on the balance of probabilities it would have resulted in the need to convert to an APER, was raised for the first time in the amended Defence. It was not raised pre-operatively with the Claimant.
- In cross-examination, Mr Meleagros conceded that the risk of converting to APER was less than 50%.
- Therefore, I conclude that the Defendant has failed to prove on the balance of probabilities that if the Claimant had undergone a TME, it would on the balance of probabilities have resulted in the need to convert to an APER.
- In cross-examination, Mr Courtney said [218],
- There is no contemporaneous reference in the medical notes to the Claimant having a narrow pelvis and this being a reason for him undergoing a TaTME. Mr Courtney agreed in cross-examination that there was no evidence before the Court as to the range of a normal male pelvis nor the dimensions of the Claimant’s pelvis [219]:
- In his third witness statement, dated 5 August 2022, Mr Courtney alleged for the first time at paragraph 3 that he told the Claimant on the telephone on 5 November 2015 that he and Mr Dalton would be carrying out a TaTME in part because of the Claimant’s narrow male pelvis. I have found at paragraph 154 above that Mr Courtney did not say this in his telephone conversation on 5 November 2015.
- The consultant radiologists, Dr Burling and Dr Scullion, agreed in the Additional Questions for Radiologists, dated 24 October 2022, that the Claimant did not have a narrow pelvis [220]:
- Mr Jenkins and Mr Meleagros agreed (see paragraphs 180-184 above) that the Claimant would have been a suitable candidate for a standard TME.
- For the above reasons, I reject the Defendant’s contention that the Claimant was not a suitable candidate for a standard TME and that this was a reason why the Claimant would, if properly consented, have agreed to a TaTME.
- Mr Jenkins says in his liability and causation report, dated February 2022 [221],
- In the colorectal experts’ joint statement, dated 20 October 2022, Mr Jenkins says [222],
- In the paper “St Gallen consensus on safe implementation of transanal total mesorectal excision” (Adamina et al 2017), it is said [223],
- In a paper entitled “Transanal total mesorectal excision for rectal cancer: evaluation of the learning curve” (Koedam et al 2018), authored by eight medical practitioners from two hospitals in the Netherlands, it is said [224],
- In the paper “Defining the learning curve of total mesorectal excision: a systematic review and meta-analysis” (Lau et al 2022), it is said [225],
- In his liability and causation expert report, dated 30 March 2022 [226], Mr Meleagros makes no mention of the fact that Mr Courtney and Mr Dalton were in the very early stages of the learning curve as they were only carrying out their second TaTME.
- When asked in cross-examination why he had not dealt with the early learning curve issue, Mr Meleagros said [227],
- When pressed in cross-examination that he had not said this in his report, he said that it was [228],
- Mr Meleagros says in his liability and causation report, dated 30 March 2022 [229],
- He repeated in cross-examination that there was no difference between functional outcomes in TaTME and laparoscopic TME [230],
- I find that Mr Meleagros should have referred in his liability and causation report to the fact that Mr Courtney and Mr Dalton were in the very early stage of the learning curve, having only carried out one previous TaTME. I find the reasons he gave for this in cross-examination unconvincing. It was not indirectly implied. It was not irrelevant. It was plainly relevant because:
- I repeat paragraph 58 above.
- A significant and oft-repeated strand of the Defence to the Claimant’s causation case is that the medical literature shows that there is no difference between the outcomes of a TaTME and a TME. I find that this is a bad point because an equivalence between a TaTME and a TME must be predicated on the medical practitioners carrying out the operations being equally experienced in both and not being in the early learning curve in one. As Mr Jenkins says in his liability and causation report dated February 2022 [234],
- The Claimant’s case is that if properly consented, he would have elected to undergo a TME laparoscopically, and on the balance of probabilities he would not have suffered total impotence, loss of ejaculatory function and loss of orgasmic function (anorgasmia). In the urological experts’ joint statement of Mr Reynard and Professor Sethia, it is said [235],
- In the Defendant’s revised counter schedule of loss, dated 28 October 2022, Mr Feeny says at page 2,
- In the urological experts’ joint statement Professor Sethia says [236],
- I find that there are the following issues regarding the Claimant’s total impotence, loss of ejaculation and anorgasmia:
- The unchallenged evidence shows that the Claimant did not suffer from impotence or loss of ejaculatory and orgasmic functions prior to his TaTME on 8 December 2015:
- It is common ground that damage to the Claimant’s parasympathetic nerves, the superior hypogastrics, has caused his total impotence, urinary incontinence and urinary urgency, and that damage to his sympathetic nerves, the nervi erigentes, has caused his loss of ability to ejaculate and anorgasmia. In the urology experts’ joint statement, dated September 2022, Mr Reynard and Professor Sethia say [241],
- Mr Courtney and Mr Dalton do not state in the operation note that they identified and sought to preserve the pelvic nerves. In cross-examination, Mr Courtney accepted that the Claimant’s pelvic nerves were not identified and preserved, and were probably damaged during the TaTME [242]:
- In cross-examining Mr Jenkins, Mr Feeny said [243],
- The Claimant’s case is that Mr Courtney and Mr Dalton should have identified and preserved the autonomic nerves in the pelvis.
- In a paper titled, “The ‘Holy Plane’ of rectal surgery”, based on a presidential address in October 1987 by T J Heald, the pioneer of TME [244], Mr Heald discusses the need to preserve the nerves and stay in the ‘holy plane’ (the mesorectal fascia) to avoid impaired potency and bladder function. He says [245],
- In a paper published in 2020 by Shiraishi et at [246], of the National Cancer Centre Hospital in Japan, on the preservation of urinary function following TaTME, they demonstrate that a step-by-step method using TaTME can achieve autonomic nerve system (ANS) preservation, and the key anatomy of ANS preservation is 4th pelvic splanchnic nerve level. It is said [247],
- The paper includes four colour photographs [248] showing the autonomic nervous system and the third and fourth splanchnic nerves. In the case of some of the patients studied, the surgeons deliberately went outside the mesorectal plane and carried out a total autonomic nerve system resection in order to remove cancer. In these cases, there was a higher rate of urinary dysfunction.
- In examination-in-chief on the third day of the trial, Mr Jenkins said [249],
- Mr Jenkins said that in this Japanese paper it is said that [250],
- Mr Jenkins said in cross-examination that it was routine in his hospital to document the identification and preservation of hypogastric nerves [251] and that if they were deliberately resected, this would also be documented [252]. Mr Feeny asked [253]:
- Mr Jenkins said in cross-examination [254]:
- It was put to Mr Jenkins in cross-examination that the damage to the pelvic side wall could be through diathermy. He replied [255]:
- In cross examination of Mr Meleagros [256]:
- Mr Meleagros was asked in cross-examination about the Japanese study by Shiraishi et al (2020) and replied [257],
- He was asked to explain the difference between the surgery in Japan and the surgery which the Claimant had. He replied [258],
- I prefer the evidence of Mr Jenkins to that of Mr Meleagros, and find that all reasonably competent and skilled colorectal surgeons identify and seek to preserve the autonomic pelvic nerves. I reject Mr Meleagros’ contention that the preservation of the autonomic pelvic nerves is peculiar to Japanese surgeons because it is contradicted by the medical literature:
- In cross-examination, Mr Meleagros said [265],
- Mr Meleagros’ answer is contradicted by the medical literature, both from the United Kingdom and worldwide; I have referred above to only a very small portion of the papers stating in terms that care should be taken to preserve the pelvic nerves. Mr Meleagros accepted that the foundation study for TME was that of Heald, “The ‘Holy Plane’ of rectal surgery”, from 1988. Mr Heald talked in terms of preserving the pelvic autonomic nerves, saying [266],
- I accept Mr Jenkins’ evidence in cross-examination that it is routine in his hospital to document the identification and preservation of the pelvic nerves [267] and that if they are deliberately resected, this would also be documented [268]. Significantly, when it was put to Mr Courtney that it was startling, bearing in mind the risks of pelvic nerve injury, that none of the relevant nerves were identified or preserved, he did not say that this was not standard practice but rather, “There is no record of it, no” [269].
- I prefer the evidence of Mr Jenkins that Mr Courtney and Mr Dalton should have identified and preserved the Claimant’s pelvic autonomic nerves when they operated upon him on 8 December 2015, not least because it is supported in terms by the medical literature.
- Mr Jenkins says that on the balance of probabilities the injuries to the Claimant’s autonomic pelvic nerves were caused by ‘wrong plane’ surgery. In his liability and causation report, dated February 2022, Mr Jenkins says [270],
- Mr Jenkins says that even after training in TaTME, iatrogenic injury rates and wrong plane surgery are high. In the joint statement it is said [271],
- Mr Jenkins said in cross-examination that surgeons can be unaware that they are in the wrong plane [272]:
- Mr Meleagros accepted in cross-examination that it is recognised that inexperienced surgeons stray outside the correct plane during the learning curve [273]:
- Mr Jenkins says that it is likely that the reason that the TaTME operation took an excessively long time (8½ - 9 hours) is because Mr Courtney and Mr Dalton, who were both early in their learning curves, were in the wrong plane.
- In the colorectal surgeons’ joint statement, dated 20 October 2022, Mr Jenkins says [274],
- In cross-examination, Mr Jenkins said that to have the “multitude of different injuries” which the Claimant has, Mr Courtney and Mr Dalton must have gone into the wrong planes in a multitude of positions [275]:
- Mr Courtney and Mr Dalton took a pathological specimen during the operation, which can be seen in photographs [276]. Mr Jenkins said at paragraph 83 of his liability and causation report, dated February 2022 [277]:
- In cross-examination, Mr Jenkins said that the minimum data required by the Pathology College is a comment on the mesorectal fascial plane and a grading of the specimen [278]. In the present case there was no comment about the mesorectal fascial plane and no grading. Further, he says that although the pictures of the specimen are helpful, they are not annotated [279]. As a consequence of these failings, Mr Jenkins said that one could draw no inference from the specimen as to whether Mr Courtney and Mr Dalton were in the correct plane or not.
- In cross-examination, the Defendant’s expert urologist, Professor Sethia, conceded that it was unlikely that the Claimant had suffered a unilateral nerve injury [280]:
- The Claimant’s urological expert, Mr Reynard, says in his report, dated February 2022 [281],
- Mr Courtney said in cross-examination, “I don’t agree we were in wrong plane surgery” [282].
- Mr Feeny submitted in his closing submissions that there is no evidence from the operation note of any feature which would suggest wrong plane surgery, specifically blood loss, identification of the wrong plane during the course of surgery, or gas emboli. He accepts that the note is unreasonably short, but says that the failure to record these matters if they occurred would go beyond the note simply being inadequate. It would be misleading.
- Mr Feeny submitted that the TaTME surgery was successful in curing the Claimant of cancer and there has been no recurrence.
- In his liability report, dated 30 March 2022, Mr Meleagros says [283],
- In cross-examination Mr Meleagros said that the nerve injury could have been caused by:
- The Defendant’s witness Dr Emma de Winton, Consultant Clinical Oncologist, says in her letter of 11 November 2015 [286],
- I find that the most probable cause of the Claimant’s total impotence, loss of ejaculatory function and anorgasmia was wrong-plane surgery for the reasons set out below.
- I accept Mr Jenkins’ evidence that during the early learning curve of TaTME, there is an association with a higher risk of wrong-plane surgery. Mr Jenkins’ evidence is supported by the medical literature. For example, in the paper ‘St Gallen consensus on safe implementation of transanal total mesorectal excision’ [287] it is said [288],
- Mr Meleagros accepted in cross-examination that it was recognised that during the learning curve, surgeons inexperienced in performing TaTMEs go outside the correct meso-rectal fascia.
- Mr Courtney and Mr Dalton were at the very beginning of their learning curve. This was their second TaTME. They were provided with no mentor. During the surgery, they were unsupervised.
- I find compelling Mr Jenkins’ evidence in cross-examination that to suffer the multitude of different injuries sustained by the Claimant, one would have to go into the wrong planes in a multitude of positions within the pelvis [289]. This point was also made by Mr Reynard, the Claimant’s urological expert, who said in cross-examination that the nerves within the pelvic wall are described as the nervi erigentes, a network. He said that to suffer the multiple damage which the Claimant sustained [290],
- The Defendant’s consultant urologist, Professor Sethia, accepted in cross-examination that it was unlikely that the Claimant could suffer the full spectrum of his injuries (erectile, ejaculatory, loss of orgasm and urinary urge and incontinence) by a unilateral nerve injury. He said [291],
- Mr Meleagros was alone in arguing that, “It could be just a single injury at one site.” [292] It was put to him that there must be multiple nerves involved because the superior hypogastric nerves provide ejaculatory function and contribute to bladder function but entirely different nerves, the nervi erigentes, are concerned with erectile function. I find that despite being asked multiple times how a single injury could cause damage to multiple nerves, he provided no satisfactory answer. Eventually he agreed that unilateral nerve damage could not possibly explain the full spectrum of the Claimant’s complications [293], “But it doesn’t mean the explanation is bilateral damage at the pelvic side walls.” I prefer the evidence of the Defendant’s urological expert, Professor Sethia, that it is likely that the injury was bilateral, not least because it is within his area of expertise.
- I accept the evidence of Mr Jenkins, Mr Reynard and Professor Sethia that for multiple nerves to have been injured, it is more probable than not that Mr Courtney and Mr Dalton went outside the ‘holy plane’, the mesorectal fascia plane, on multiple occasions. This can be seen from the diagram in the paper by Shiraishi et al [294], which shows that the neurovascular bundle and pelvic nerves are all outside the mesorectum.
- I find that whilst it is possible that the Claimant’s multiple pelvic nerve damage was caused by thermal injury, it is far more likely that it was caused by wrong-plane surgery. Professor Sethia did not advance the thermal injury argument. Mr Meleagros did not refer to any literature which supported it. The medical literature before the Court overwhelmingly shows [295],
- I find that there is no basis for Mr Meleagros’ suggestion in cross-examination that damage to the pelvic nerves could have been caused by the insertion of rigid instruments down the anal canal. This was referred to for the first time in his cross-examination and it is not supported by the Defendant’s urological expert, Professor Sethia.
- Whilst it is common ground that radiotherapy increases the risk of impotence, I find that it can be discounted in this case. Firstly, Dr Emma de Winton, Consultant Clinical Oncologist, says that it adds a very small additional risk to the chance of impotence [296]. She said in cross-examination [297],
- Secondly, the Claimant has suffered damage to multiple pelvic nerves, causing total impotence, loss of ejaculatory function, anorgasmia and urinary urge and incontinence. I conclude that the Claimant’s multiple injuries are far more consistent with Mr Courtney and Mr Dalton having gone outside the mesorectal fascia on more than one occasion.
- Mr Feeny argues that the fact that the surgery has been curative of the Claimant’s cancer indicates that the surgeons were in the correct plane. I reject this as a non sequitur. The fact that Mr Courtney and Mr Dalton were in the correct plane at one point does not indicate that they were in the correct plane at all times.
- I find that I cannot rely upon Mr Courtney’s assertion that he was in the right plane, and that his record of the operation does not refer to having been in the wrong plane, bearing in mind:
- For the aforementioned reasons, I find that the Claimant has proved on the balance of probabilities that it is likely that the Claimant’s total impotence, loss of ejaculatory function and anorgasmia were caused by the Defendant by their surgeons going into the wrong plane on more than one occasion and injuring the autonomic pelvic nerves.
- In his causation and condition and prognosis report, dated February 2022, Mr Reynard referred to 17 studies when considering the issue of whether it is likely on the balance of probabilities that the Claimant would have suffered total impotence, loss of ejaculatory function and anorgasmia. Mr Reynard says that these studies show that most men (60-85%) remain potent and have preserved bladder function after anterior resection with TME with autonomic nerve preservation. He referred inter alia to the following literature:
- Mr Meleagros said in the colorectal experts’ joint statement, dated 20 October 2022 [304],
- In his expert report the Defendant’s urologist, Professor Sethia, only relied on one paper, by Lange [305] in 2009, which showed that 76% of the men involved reported sexual dysfunction following TME surgery. However, the study does not differentiate between the degree of sexual dysfunction suffered or state how many patients suffered total impotence.
- In cross-examination, it was put to Professor Sethia that the Lange paper found that of the male patients who were sexually active before treatment, 68.5% were sexually active after three months and 71.5% were sexually active two years after treatment. Professor Sethia sought to critique the Lange paper by saying that many of the papers dealing with sexual dysfunction, including the Lange paper, do not use objective measures of sexual function and that when a sexual function is self-reported, it is notoriously unreliable.
- It was put to Professor Sethia that the study shows that the large majority of patients were sexually active after surgery. He replied that many papers, including the Lange paper, do not use objective measurements of sexual function. Dr Ellis put the following to him [306]:
- Professor Sethia had never suggested that the only paper on which he relied, namely the Lange paper, was unreliable in his expert reports or in the joint statement with Mr Reynard.
- I accept Mr Reynard’s evidence because it is supported by the medical literature to which he refers; I refer to five of the papers at paragraph 281 above. Although this literature often involves relatively low numbers of patients, and is therefore less persuasive, it all points in the same direction: that it is more likely than not that patients undergoing TME with autonomic nerve preservation will maintain erectile and ejaculatory potencies. Mr Reynard summarises his opinion in his causation and condition and prognosis report, dated February 2022 [307],
- Professor Sethia only referred to one paper, by Lange. In the Lange paper, it is said in the introduction [308],
- It is said in the Lange paper [309],
- I find that Professor Sethia did not have an answer to the fact that the Lange paper showed that of the male patients who were sexually active before treatment, 68.5% were sexually active after three months and 71.5% were sexually active two years after treatment. His response, suggesting that many papers dealing with sexual dysfunction, including the Lange paper, do not use objective measures was not said in his report or in the joint statement. To the contrary, he relied upon the Lange paper. Further, I found his evidence that some of the men who claimed to be sexually active may only have been referring to stimulating their partners not credible and a desperate attempt to explain away inconvenient data in the only paper upon which he relied in his report.
- For completeness, I would add that Professor Sethia wrongly said in his liability and causation report that the Claimant had a BMI of 35 [310], which moves it out of Class 1 obesity. In cross-examination he accepted that this was wrong and that in fact the Claimant had a BMI of 32 [311], and so was in Class 1.
- For the aforementioned reasons, I prefer the evidence of Mr Reynard to that of Mr Sethia and find that the Claimant has proved on the balance of probabilities that if he had undergone a laparoscopic TME, he would not have suffered total impotence, loss of ejaculatory function and anorgasmia.
- In his witness statement, dated 18 November 2021, the Claimant says [312],
- The extent of the Claimant’s urinary urgency and incontinence is agreed. The Defendant’s urologist, Professor Sethia, says in his condition and prognosis report, dated July 2022 [313],
- In his expert report, dated February 2022, the Claimant’s Consultant Urological Surgeon, Mr Reynard, says [314],
- Regarding prognosis, Professor Sethia says in his condition and prognosis report, dated July 2022 [315],
- Mr Jenkins says in his condition and prognosis report, dated 29 March 2022 [316],
- Mr Reynard and Professor Sethia agree in their joint statement, dated September 2022 [317],
- Professor Sethia says in the joint statement [318] that,
- Mr Reynard says in the joint statement [319],
- Mr Jenkins says in his liability and causation report, dated February 2022 [320],
- I have found that Mr Courtney and Mr Dalton went outside the mesorectal fascial plane and damaged the Claimant’s pelvic nerves, including the superior autonomic nerve, which regulates bladder functions.
- I prefer the evidence of Mr Reynard and Mr Jenkins to that of Professor Sethia, and find that it is more likely than not that the Claimant’s urinary urgency and incontinence was caused when Mr Courtney and Mr Dalton went outside the mesorectal fascial plane and damaged the Claimant’s pelvic nerves, which regulate bladder function.
- The next issue is whether on the balance of probabilities, the Claimant would have suffered the same degree of urinary urgency and incontinence if he had undergone a conventional laparoscopic TME.
- At paragraph 5(c)(vii) of the amended Defence it is said [321],
- In his liability and causation report, Mr Meleagros says at paragraph 1.30 [322],
- Mr Reynard says in his causation and condition and prognosis report, dated February 2022 [323],
- In the urology experts’ joint statement, dated September 2022, Mr Reynard says [324],
- I accept Mr Reynard’s evidence that NICE and the medical literature show that on the balance of probabilities the Claimant would not have suffered his urinary dysfunction if he had undergone a conventional laparoscopic TME with autonomic pelvic nerve preservation. By way of example, I would refer to:
- In the urology experts’ joint statement, dated September 2022, Professor Sethia says [329],
- Professor Sethia accepts in his report, dated 21 December 2021, that on the balance of probabilities, the Claimant’s urinary urgency and incontinence was not caused as a result of his radiotherapy. He says [330],
- In cross-examination, Mr Meleagros sought to say that in his liability and causation report, dated 30 March 2022, he had said that the medical literature showed that on the balance of probabilities the Claimant would have suffered sexual dysfunction even if he had undergone a TME. However, when pressed he accepted that he had said at paragraph 1.30 [331] that the Claimant would also have suffered urinary dysfunction. He then conceded that this assertion was not supported by medical literature [332]:
- For the aforementioned reasons, I conclude that the Claimant has proved on the balance of probabilities that if he had undergone a laparoscopic TME with autonomic nerve preservation, it is unlikely that he would have suffered urinary urgency and urinary incontinence.
- In “Management guidelines for low anterior resection syndrome - the MANUEL project” (Christensen et al 2021) it is said [333],
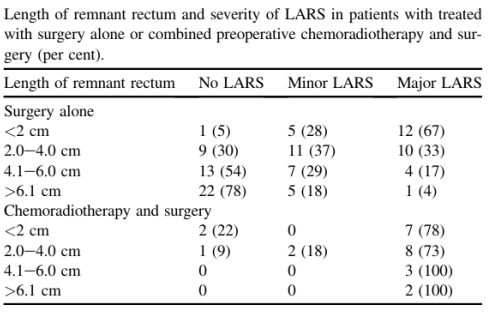
- At the time of the Claimant’s surgery on 8 December 2015, there were no predictive calculations for LARS, such as POLARS. In 2017, a LARS table was introduced. The purpose of this scale was to predict the level of LARS prior to surgery so that patients could decide whether to undergo a colostomy. In the paper “Neoadjuvant therapy abolishes the functional benefits of a larger rectal remnant, as measured by magnetic resonance imaging after restorative rectal cancer surgery”, by Bondeven, Emmertsen et al at Aarhus University Hospital in Denmark in 2015 it is said [334],
- In the paper, “Functional complaints and quality of life after transanal total mesorectal excision: a meta-analysis” (Van der Heijden 2020), it is said [335],
- In the colorectal surgeons’ joint statement, dated 20 October 2022, it is agreed that based upon the height of the tumour, the Claimant would have suffered from major LARS in any event. It is said[336],
- In his liability and causation report, dated February 2022, Mr Jenkins says [337],
- The Claimant’s case is that whilst he accepts that if he had undergone a laparoscopic TME he would have suffered major LARS, he contends that his LARS is significantly worse as a result of undergoing a TaTME and having a low colorectal anastomosis and handsewn purse strings. In his liability and causation report, dated February 2022, Mr Jenkins says [338],
- The Defendant’s case is that, as said by Mr Meleagros in his condition and prognosis report, dated 9 July 2022 [339],
- I have already found that the tumour was mid-rectum and not low-rectum (see paragraphs 194 to 196 above).
- In the “Additional questions for radiologists - Monday 24 October 2022”, Mr Scullion (DS) and Mr Burling (DB) say [340],
- In his liability and causation report, dated February 2022, Mr Jenkins says [341],
- Mr Jenkins refers to a number of papers which show that patients who have a lower anastomosis and a hand-sewn anastomosis are likely to have a higher complication rate including LARS:
- In cross-examination, Mr Jenkins said [347],
- In cross-examination, Mr Jenkins said that damage to the Claimant’s internal anal sphincter had made his LARS worse [349]:
- In his condition and prognosis report, dated 9 July 2022, Mr Meleagros says [350],
- In cross-examination, Mr Meleagros said [351],
- In the joint statement of the colorectal surgeons, dated 20 October 2022, they say:
- The paper “Neoadjuvant therapy abolishes the functional benefits of a larger rectal remnant, as measured by magnetic resonance imaging after restorative rectal cancer surgery”, by Bondeven, Emmertsen et al reported on a study of 125 patients who underwent sphincter-preserving surgery for rectal cancer at Aarhus University Hospital in Denmark in 2015. It is said [359],
- In the Bondeven paper it is also said [360],
- The paper includes a table, which records the following outcomes:
- Mr Jenkins made the point that the Bondeven paper reports on a small study of 125 and he says that as a consequence very little can be drawn from it. In reply, Mr Feeny submitted that the Bondeven paper was authored by experts in the field. He further submitted that the Bondeven paper was approved in a paper entitled “Management guidelines for low anterior resection syndrome - the MANUEL project” (Christensen et al 2021) [361]. They say [362],
- While Mr Jenkins accepts that the authors of the MANUEL project are experts in the field, he replies that they come from the same hospital as the authors of the Bondeven paper.
- I was also referred to the paper “Two dominant patterns of low anterior resection syndrome and their effects on patients’ quality of life” (Kim et al 2021) [363], which concerned a study of 283 patients who underwent restorative anterior resection for left-sided colorectal cancer. This study showed that 40.8% of patients who underwent an anastomosis with end-to-end double stapling had major LARS and 41.5% of patients who had end-to-end hand sewn anastomosis had major LARS.
- It is common ground that little is known about the pathophysiology of LARS but the causes of LARS are multifactorial. Mr Jenkins says in the joint statement [364],
- It is common ground that the functional outcome is likely to be worse if the entire mesorectum is excised. In this case, the consultant radiologists, Dr Burling and Dr Scullion, both agree that the decision to excise surgically the entire rectum and its surrounding mesorectum was appropriate [365].
- It is common ground that the Claimant would have had major LARS even if he had undergone laparoscopic TME by reason of the height of the tumour. Further, Mr Jenkins concedes that the Claimant’s major LARS would have been further exacerbated by him having undergone neoadjuvant radiotherapy.
- I find that the Claimant has failed to prove on the balance of probabilities that the fragmentation of his internal anal sphincter has caused a material exacerbation or worsening of his LARS.
- I accept the Defendant’s contention that, as shown by the Bondeven paper, 80% of patients who received pre-operative chemoradiotherapy reported having major LARS and in these cases, a larger remnant rectum did not offer any benefit in terms of functional outcome. Whilst I accept that the Bondeven paper was based on a small study and is therefore less persuasive, it was carried out by experts in the field of colorectal cancer and was quoted with approval in the MANUEL project. Again, I recognise that the authors of the MANUEL project are in the same hospital as those of the Bondeven study, but I note again that Mr Jenkins accepted that they were leaders in the field. Therefore, I find that on the balance of probabilities if the Claimant had undergone a laparoscopic TME, having regard to the fact that he had undergone neoadjuvant radiotherapy, his LARS was unlikely to have been any less severe.
- Mr Feeny referred the Court to Tahir v Haringey Health Authority [1998] Lloyds Rep (Med) 104, in which Otton LJ said,
- I accept Mr Meleagros’ evidence that if the Claimant had undergone a TME, the anastomotic height would have been unlikely to have been more than 2cm higher. I note that on 18 October 2017 the Claimant had a consultation with Mr Antoniou at the London Clinic. Mr Antoniou wrote [366],
- Even if I accepted Mr Jenkins’ evidence that Claimant’s LARS was worsened by the TaTMe, the Claimant must prove a measurable damage and not a general increment. In cross-examination Mr Jenkins conceded that with a 2cm difference in tumour height you might move down from say 31 to 30 on POLARS [367]. He was asked whether it would be possible to say whether there would be a difference in terms of lifestyle and employment if the Claimant’s POLARS was 31 instead of 30. He replied [368]:
- For the aforementioned reasons, I find that the Claimant has failed to prove on the balance of probabilities that his LARS has been exacerbated or worsened in a measurable way by undergoing a TaTME.
- Mr Meleagros says in his condition and prognosis report, dated 9 July 2022 [369],
- The Claimant alleges at paragraph 69 b) of the amended Particulars of Claim [370],
- There are three issues:
- Dr Scullion says in his report, dated August 2022 [371],
- Dr Burling says in his report, dated February 2022, under the heading “Conclusion” [372],
- Dr Burling said in cross-examination [373],
- In their joint statement, dated 5 September 2022, the radiology experts, Dr Burling and Dr Scullion, say [374],
- Mr Jenkins says in his liability and causation report, dated February 2022,
- In his liability and causation report, dated 30 March 2022, Mr Meleagros says at paragraph 2.26 [375],
- However, in the colorectal experts’ joint statement, dated 20 October 2020, Mr Meleagros says [376],
- In their joint statement, the colorectal surgeons say [377],
- I find that both radiologists and both colorectal surgeons agree that the internal anal sphincter fragmentation was caused by the TaTME.
- Mr Jenkins says in his liability and causation report, dated February 2022 [378],
- In cross-examination Mr Jenkins said [379],
- Mr Jenkins says in the colorectal experts’ joint statement, dated 20 October 2022 [380],
- Dr Burling said in cross-examination [381],
- I find that on the balance of probabilities, the Claimant would not have suffered trauma to his internal sphincter fragmentation if he had undergone a TME because:
- In his liability and causation report, dated February 2022, Mr Jenkins says [382],
- Mr Jenkins continues that on the balance of probabilities, if the Claimant had undergone a conventional TME, his faecal incontinence would have been considerably less frequent, no more than two to three times per week [383].
- In his condition and prognosis report, dated 9 July 2022, Mr Meleagros says [384],
- In the colorectal experts’ joint statement, dated 20 October 2022, Mr Jenkins says [385],
- In cross-examination Mr Jenkins said [386],
- I accept the Claimant’s evidence that since the TaTME he has suffered from faecal urge and incontinence. It is common ground that the Claimant would have suffered from major LARS in any event and that one of the symptoms of LARS is faecal incontinence. In his closing submissions, Mr Feeny submitted that the Court should apply Occam’s Razor, that is that as it is common ground that one of the symptoms of LARS is faecal incontinence, there is no need to look for any other cause for his faecal incontinence.
- I find that Mr Jenkins’ opinion that [387] “… better sphincter preservation would have produced less dysfunction from faecal incontinence, accepting severe LARS would still be likely” is supported by the medical literature. In “Bowel dysfunction after treatment for rectal cancer” (Emmertsen 2008) it is said [388],
- In the colorectal experts’ joint statement, Mr Meleagros accepts that [389],
- Mr Meleagros accepts that there is a risk of faecal incontinence with TaTME because the anal sphincter is stretched by the instruments inserted via the anus, but says that the clinical evidence shows that the Claimant’s anal sphincters have not been damaged. I reject this opinion because:
- I accept Mr Jenkins’ evidence that the Claimant’s faecal incontinence would have been considerably less frequent, and no more than two to three times per week, whereas, as stated by Mr Meleagros in his condition and prognosis report at paragraph 6.13, since the TaTME the Claimant has suffered from faecal incontinence approximately once a day and also during the night.
- I conclude that the Claimant has proved on the balance of probabilities that by reason of undergoing a TaTME he has suffered a significant increase in faecal incontinence, namely twice a day rather than two to three times a week, which he would not have suffered if he had undergone a laparoscopic TME.
- The Claimant is now aged 63. I find that the Claimant is entitled to general damages for pain, suffering and loss of amenities (PSLA) for the injuries summarised below.
- The Claimant has suffered:
- He says in his witness statement, dated 18 November 2021 [393],
- The Claimant’s wife, Mrs Snow, says in her witness statement of 18 November 2021 [394],
- I repeat paragraph 293-297 above.
- Mr Jenkins says in his condition and prognosis report, dated 29 March 2022 [395],
- In the urology experts’ joint statement, Mr Reynard and Professor Sethia say [396],
- The Claimant has suffered a significant increase in faecal incontinence, namely approximately twice a day instead of two to three times a week. He would not have suffered this if he had undergone a laparoscopic TME. The Claimant wears a pad and protective pants regularly. It is unlikely that there will be any improvement and Mr Jenkins says at paragraph 7.1 of his condition and prognosis report dated 29 March 2022 [397], that as the Claimant ages, his faecal incontinence will deteriorate.
- Both expert psychiatrists agree that the Claimant had no psychiatric problems prior to the index surgery:
- Dr Turner, Consultant Psychiatrist, says in his report, dated February 2022 [400],
- In the joint psychiatric statement, dated 20 September 2022, of Dr Turner and Dr Amin, they say [401],
- Prior to surgery, the Claimant and his wife used to visit London two or three times a year and went to the theatre and restaurants. As a consequence of the Claimant’s injuries, they have reduced their visits. On a recent visit, the Claimant went to the restaurant with his wife and friends but did not eat anything so as to reduce his need to visit the toilet, although he still visited the toilet twice during the show. Prior to surgery, he and his wife ate at local restaurants at least twice a week. Since surgery, they have not done so and only eat at a local restaurant with easily accessible toilet cubicles.
- I bear in mind that the impact on the Claimant’s social life is caused by his bladder and urinary incontinence, LARS (for which I have found that no compensation is payable) and faecal incontinence caused by the damage to his internal anal sphincter.
- In the Claimant’s updated schedule of loss, dated 27 October 2022, general damages for pain, suffering and loss of amenities (PSLA) are claimed as follows:
- Mr Feeny submits in the Defendant’s counter schedule of loss [402] that if the impact of the Claimant’s bowel symptoms is as great as the Claimant indicates, then he is failing to mitigate his loss by not agreeing to have a permanent stoma.
- Mr Feeny contends that an aggregate of awards for different types of injury is not appropriate, given that there will be a significant overlap of the different injuries in terms of their impact on the Claimant. He submits that a reasonable figure for general damages for PSLA would be £85,000, including £15,000 for the Claimant’s adjustment disorder. Mr Feeny submits that the Claimant would have suffered some degree of psychiatric harm in any event, due to his rectal cancer.
- I find that the Defendant has failed to prove that the Claimant has not mitigated his loss by not agreeing to have a permanent stoma. Bearing in mind the unsuccessful outcome of the surgery on 8 December 2015, I find that it is reasonable that the Claimant does not wish to undergo surgery for a stoma.
- The correct approach to the assessment of general damages for PSLA is to assess the individual injuries and then consider whether the aggregate of the awards should be reduced to take into account double accounting, increased to reflect the fact that the totality of the injuries is greater than the individual components, or whether no adjustment should be made. This was the approach endorsed by Pitchford LJ in Sadler v Filipiak [2011] EWCA Civ 1728. His Lordship said,
- I find that the Claimant is entitled to general damages for PSLA of £180,000. I have arrived at this figure as set out in the paragraphs below.
- Regarding permanent total impotence, loss of ejaculatory function and anorgasmia, I have had regard to the Judicial College Guidelines 16th edition, pages 30-31, which provide:
- Dr Ellis submits that the Claimant is entitled to an award of £114,900, at the bottom of bracket (b) of the Judicial College Guidelines. He says in his written closing submissions on quantum,
- In my judgment bracket (b) above does not apply because it applies to total impotence and loss of sexual function and sterility in the case of a young person (my emphasis). This cannot apply to the Claimant, who was aged 56 at the date of the index operation and is now aged 63. Bracket (c) awards £43,010 to £88,750 for impotence or significant sexual dysfunction which is likely to be permanent. The Claimant suffers from total impotence and significant sexual dysfunction, and I therefore find that he falls at the top of bracket (c), and I award £88,750.
- Regarding urinary urgency, urinary incontinence, I have been assisted by the Judicial College Guidelines 16th edition, pages 36-37, which provide:
- I bear in mind that the Claimant suffers incomplete voiding (he retains about one third of his bladder volume), reduction of awareness of bladder fullness, frequent voiding 8-9 times daily, with voiding twice at night, urge incontinence and leakage on a daily basis. On the other hand, there is no evidence that the Claimant suffers from pain associated with his urinary urge and incontinence.
- In my judgment the Claimant is entitled to general damages for PSLA for his urinary urgency and urinary incontinence in the sum of £70,000.
- Regarding faecal urgency and incontinence, I have had regard to the Judicial College Guidelines 16th edition, page 36, which provide:
- I bear in mind that the Claimant suffers faecal incontinence during the day and night every day, as opposed to two or three times a week. I find that there is a significant overlap between the Claimant’s major LARS and the faecal incontinence attributable to the injury to his internal anal sphincter and that they together have had a very severe impact upon his life.
- In my judgment the Claimant is entitled to general damages for PSLA for faecal incontinence caused by the injury to his internal anal sphincter in the sum of £30,000.
- Regarding the prolonged adjustment disorder with depression, I have had regard to the Judicial College Guidelines 16th edition, pages 12-13, which provide:
- The consultant psychiatrists agree that the Claimant has suffered a “substantial” and “significant” adjustment disorder and depression by reason of his physical injuries. I find that the appropriate Judicial College Guideline is 4(A)(b) and the appropriate award is £40,000. The Consultant Psychiatrists were not asked in their joint statement whether or to what extent the severity of the Claimant’s adjustment disorder and depression was attributable to the major LARS, from which I have found the Claimant would have suffered even if he had undergone a laparoscopic TME. In the absence of evidence on this point, I award the Claimant general damages for his substantial adjustment disorder and moderately severe depression of £25,000.
- The Claimant seeks an award for pain and discomfort of £29,780.
- I make no award for PSLA for pain and discomfort because I find that on the balance of probabilities this pain is caused by his LARS, for which I have found that no compensation is payable. It is said in the Claimant’s GP records dated 26 April 2016 [403],
- I have thus made the following awards:
- The awards above total £213,750. Standing back and having regard to overlap between the pain and suffering caused by the various injuries, I globalise the award for general damages for PSLA and award the Claimant £180,000.
- The Claimant is entitled to interest on the general damages for PSLA at 2% from the date the claim form was served upon the Defendant, i.e. 8 December 2018, to 13 January 2023. The interest owing on £180,000 is £14,764.93.
- The Claimant’s past and future financial losses are particularised in an updated schedule of loss, dated 27 October 2022.
- The Claimant claims past loss of net earnings in the sum of £60,876. He also claims £2,100 for loss of employer’s pension contributions in 2016.
- The Claimant says in his witness statement, dated 18 November 2021 [404],
- The Claimant says that he could not work at Rolls Royce as he could not fufil the travel requirements due to his severe LARS. I find that on the Claimant’s own evidence, it was the LARS which was preventing him from working and I have found that he is not entitled to compensation for LARS. I further find that his major LARS would have prevented him from working, irrespective of his urinary urge and incontinence and faecal incontinence and urge, and therefore I make no award under this head of loss.
- It is said in the updated schedule of loss, dated 27 October 2022, at page 11,
- In the second witness statement of Mrs Snow, dated 17 October 2022, she says [405],
- In the Defendant’s revised counter schedule, dated 28 October 2022, Mr Feeny says at paragraph 3 that all of the claim for gratuitous care arose from the Claimant’s LARS symptoms and is therefore irrecoverable.
- I reject the Defendant’s contention and find that it is apparent from paragraph 7 of Mrs Snow’s second witness statement that the gratuitous care was in respect of all of his injuries, including his urinary urge and incontinence, caused by damage to his internal anal sphincter.
- The claim for care is broken down into four periods and totals £16,837.61:
- The Defendant did not challenge the hours claimed for gratuitous care or the hourly rates claimed. In my judgment the gratuitous care that is claimed is reasonable for the injuries the Claimant has sustained. I note that the care has been reducing with the passage of time.
- I find that the Court must adopt a broad-brush approach and I assess 50% of the gratuitous care as attributable to the injuries for which I have found the Claimant has proved that he is entitled to receive compensation.
- I conclude that the Claimant is entitled to damages for gratuitous care in the sum of £8,418.81, i.e. 50% of £16,837.61.
- At paragraph 4 of the updated schedule of loss, the Claimant claims incontinence and hygiene products. It is said,
- The Claimant provides a detailed breakdown of the incontinence and hygiene products he has purchased from 1 March 2016 to 20 October 2022, totalling £11,000.75.
- I reject the Defendant’s contention at paragraph 4.1 of the counter schedule that the majority of these expenses were incurred as a result of the Claimant’s LARS and are therefore irrecoverable.
- I find that 50% of these expenses are referrable to the Claimant’s urinary incontinence and the faecal incontinence caused by the injury to the internal anal sphincter and therefore award the Claimant 50% of £11,000.75, i.e. £5,500.38.
- At paragraph 4.2 of the updated schedule, the Claimant claims £1,500 for additional laundry and electricity.
- I find that the Claimant has proved on the balance of probabilities that by reason of his urinary leakage and faecal incontinence attributable to the damage to his internal anal sphincter, he incurred additional laundry costs between 1 March 2016 and 20 October 2022.
- I make an award of 50% of £1,500, i.e. £750.
- At paragraph 4.3 of the updated schedule, the Claimant claims £2,324 for replacement clothing and underwear from 1 March 2016 to 20 October 2022.
- I find that the Claimant has proved on the balance of probabilities that by reason of his urinary leakage and faecal incontinence attributable to the damage to his internal anal sphincter, he required replacement clothing and underwear in the sum of £2,324.
- I award 50% of £2,324, i.e. £1,162.
- At paragraph 4.4 of the updated schedule, it is said,
- In her second witness statement, dated 17 October 2022, the Claimant’s wife, says [406],
- In his witness statement, dated 18 November 2021, the Claimant says at paragraph 71 [407],
- I accept Mr Feeny’s submission that it is more likely than not that the Claimant required a further toilet by reason of his LARS symptoms. Further, I note that at paragraph 68 of the Claimant’s witness statement [408] he says that toilet visits often take 30 to 60 minutes. It appears from what he says in this paragraph that the length of this visit is caused very largely if not entirely by his LARS symptoms. Paragraph 75 of the Claimant’s witness statement reinforces this [409].
- Therefore, I make no award for the installation of an additional en-suite toilet.
- At paragraph 4.5 of the updated schedule, the Claimant claims gardening at £270 per annum for the annual cost of cutting the back hedge, totalling £1,890.
- The Defendant says that the Claimant’s inability to cut the back hedges arises from his LARS symptoms and is therefore irrecoverable.
- I find that on the balance of probabilities the Claimant’s inability to cut the back hedge is caused by his urinary dysfunction, faecal incontinence caused by the damage to his internal sphincter and his LARS. I find that the Claimant is entitled to 50% of the cost of cutting the back hedge, i.e. £945.
- At paragraph 4.6 of the updated schedule, the Claimant makes a claim for the additional cost of his daughter’s boarding fees.
- Prior to the Claimant’s surgery, he used to transport his daughter to all of her extracurricular activities, including to regular hockey training in Exeter and tournaments all over South West England.
- Due to the Claimant’s injuries, his daughter had to board at her school for four nights a week. The boarding fees from 8 February 2016 to 31 May 2017 were £9,016.
- I find that the Claimant is entitled to recover 50% of this claim, i.e. £4,508, on the basis that on the balance of probabilities 50% is attributable to the Claimant’s urinary urge, urinary urge and faecal incontinence caused by the injury to the internal anal sphincter.
- At paragraph 4.7 of the updated schedule, the Claimant seeks to recover travel expenses of £4,305.64.
- I find that the Claimant is entitled to recover his travel expenses in relation to treatment for his urological and sexual dysfunction. These total £857.70.
- I disallow the mileage sought for collecting prescriptions from the surgery because it is unclear if this is for LARS.
- At paragraph 4.8 of the updated schedule, the Claimant seeks to recover £240 for winding up his company, AMS 1911 Limited, on the grounds that by reason of his injuries he was unable to return to work in early February 2016 as planned.
- I accept Mr Feeny’s submission that this is a loss suffered by a third party, and is irrecoverable.
- I have made the following awards for past financial losses:
- The Claimant is entitled to interest on the past financial losses from 8 December 2015 to 13 January 2023: £401.13.
- At paragraph 5.1 of the updated schedule, the Claimant sets out his claim for loss of future earnings. His case is that he would have worked full time until 24 August 2032, when he would be 73, and thereafter he would continue to work as a part-time consultant (50% of full time) for two years.
- I find that the Claimant has failed to prove loss of future earnings for the same reasons as his claim for past loss of earnings fails.
- In the alternative to his claim for loss of future earnings, a claim is made for handicap on the labour market.
- Whilst the Claimant is plainly handicapped on the labour market, I find that this is attributable to LARS and that his urinary and faecal incontinence do not give rise to any greater handicap on the labour market. As a consequence, I make no award for damages for handicap on the labour market.
- I find that the Claimant is not entitled to damages for the cost of Biofeedback because this would appear to be referable to LARS.
- Regarding treatment for bladder overactivity, the Claimant seeks to recover damages for Botox injections. The injections would occur every 9 to 12 months and would cost approximately £3,000 per injection. The Claimant is at risk of requiring intermittent catheterisation, probably needing to self-catheterise approximately 5 to 6 times daily. Catheters cost £50 for a packet of 30 catheters, i.e. £1.67 each. The Claimant is expected to attend a training session by a nurse, costing £100.
- In the up-dated schedule, the Claimant says he will defer Botox treatment until he has retired. In cross-examination, he said that he had no present intention to have this treatment but intended to have it at some point in the future. In the updated schedule, the claim is made from age 73 for life. I note that Mr Reynard says in his causation and condition and prognosis report, dated February 2022, at paragraph 141 [410],
- I find that the Claimant is entitled to recover the cost of 10 Botox injections and that he will receive the first when he is 73. With a discount factor of -0.25%, the multiplier for annual injections over 10 years is 10.13 (Ogden Table 36), and the adjustment because the loss will not occur for another 10 years is 1.0253 (Ogden Table 35). 10.13 x 1.0253 = 10.386. £3,000 x 10.386 = £31,158.
- In the joint statement Mr Reynard and Professor Sethia say [411],
- I allow £55 per month over 10 years from age 73. £55 x 12 x 10.13 x 1.0253 = £6,854.95. I allow £350 for an initial consultation, in ten years’ time. £350 x 1.0253 = £358.86.
- The total amount which I award for Botox injections is therefore £31,158 + £6,854.95 + £358.86 = £38,371.81.
- Mr Reynard, Consultant Urological Surgeon, says in his report, dated February 2022 [412],
- The Claimant has sought and I have accepted that he is entitled to Botox treatment for life from age 73. In the light of this, I find that it would amount to double recovery to make an award for the implementation of sacral neuromodulation.
- The Claimant claims the cost of implantation of a penile prosthesis.
- In cross-examination, the Claimant said [413],
- The Claimant’s honesty is to his credit. I find that he has not proved on the balance of probabilities that he will undergo treatment for a penile prosthesis. I also bear in mind that I have awarded Botox treatment from age 73 for life, and I find that he is unlikely to undergo the implementation of penile prosthesis in addition to this. Therefore I make no award for this head of loss.
- The psychiatrists, Dr Turner and Dr Amin, say in their joint statement, dated 20 September 2022 [414] in answer to question 1b),
- In the light of this agreement, I allow 10 sessions of CBT at £200 per hour, i.e. £2,000.
- In his report, dated February 2022, the Claimant’s psychiatrist, Dr Turner, says at paragraph 32 [415],
- I allow three booster courses of three sessions each at £200 each, i.e. £600 x 3 = £1,800.
- In the joint statement, Dr Turner and Dr Amin agree [416],
- I find that the Claimant is entitled to recover the cost of psychosexual counselling, namely 15 sessions at £200, totalling £3,000.
- I find that the Claimant is entitled to recover travelling expenses for the medical treatment he will undergo, namely botox injections, one consultation on intermittent self-catheterisation, cognitive behavioural therapy and marriage counselling.
- I note that in the claim for past travelling expenses, the Claimant has received much of his treatment at the BMI Bath Clinic, which involves a round-trip of 54 miles, and I assess the travel costs on the basis that future medical treatment will also be received there.
- In respect of travelling expenses for Botox injections, I award 54 miles @ 45p = £24.30 p.a. x 10.386 [417] = £252.38.
- In respect of travelling expenses for one consultation on intermittent self-catheterisation, I award 54 miles @ 45p = £24.30 x 1.0253 because the loss will not occur for another 10 years (Ogden Table 35) = £24.91.
- I have found that the Claimant is entitled to 19 sessions of CBT. I therefore award travelling expenses of 54 miles @ 45p x 19 = £461.70 for CBT.
- I have found that the Claimant is entitled to 15 sessions of marriage counselling. I therefore award travelling expenses of 54 miles @ 45p x 15 = £364.50 for CBT.
- I therefore award £1,103.49 for travelling expenses.
- At paragraph 6.3 of the updated schedule the Claimant claims for toilet roll, wet wipes and incontinence pads a multiplicand of £2,316.01.
- I find that 50% of these expenses are referrable to the Claimant’s urinary incontinence and the faecal incontinence caused by the injury to the internal anal sphincter and I therefore award a multiplicand of 50% of £2,316.01, i.e. £1,158.
- The multiplier for life is 22.76 (Ogden table 1). £1,158 x 22.76 = £26,356.08.
- The Claimant for additional laundry at paragraph 6.4 of the updated schedule. This includes a 10% annual increase. It is clear law that an increase for inflation is not recoverable.
- For the first year, the Claimant seeks £250. I have found that 50% of the additional laundry costs are referrable to the Claimant’s urinary incontinence and the faecal incontinence caused by the injury to the internal anal sphincter and I therefore award 50% of £250 = £125.
- The multiplier for life is 22.76 (Ogden table 1). £125 x 22.76 = £2,845.
- At paragraph 6.5 of the updated schedule the Claimant claims £3,000 per annum for holidays to cover excess luggage for his equipment and incontinence products, a hotel room with two en suite toilets and business class travel by air. He says in the updated schedule that he and his family usually have two holidays in Europe and one long haul holiday each year.
- In his witness statement the Claimant says at paragraph 79 [418],
- I find that on the balance of probabilities the Claimant’s LARS symptoms would necessitate this additional expenditure and therefore I make no award for additional travelling expenses.
- The Claimant claims £350 per annum for the cost of replacement clothing and underwear at paragraph 6.6 of the updated schedule.
- Bearing in mind that the Claimant would have required some replacement clothing and underwear because he would have suffered from LARS in any event, I allow 50% of £350. i.e. £175.
- The multiplier for life is 22.76 (Ogden table 1). £175 x 22.76 = £3,983.
- At paragraph 6.7 of the updated schedule, the Claimant claims future gardening costs for cutting his back hedge of £280 per annum until age 76. I repeat paragraph 437 above and allow 50%, i.e. £140 per annum. The multiplier for 13 years is 13.21, and I therefore award £1,849.40.
- I have made the following awards for future losses:
- I summarise below the awards I have made:
i) Permanent total impotence, total inability to ejaculate and anorgasmia;
ii) Urinary incontinence and urgency;
iii) Faecal urgency and incontinence;
iv) Exacerbation of Lower Anterior Resection Syndrome (LARS);
v) Moderate prolonged adjustment disorder and depression.
i) Trial bundle of 1833 pages;
ii) Supplemental trial bundle of 696 pages;
iii) Core medical records bundle of 412 pages
iv) Medical records bundle of 1807 pages.
Reference to page numbers in the footnotes below is to the trial bundle unless otherwise stated.
Admission of Mr Bilson’s witness statement
Parties
Lay witnesses
i) Himself, dated 18 November 2021 [3];
ii) His wife, Mrs Helen Snow, dated 18 November 2021 [4];
iii) Christopher Bilson, dated 28 February 2021 [5].
i) Mr Edward Courtney, Consultant General Colorectal Surgeon, dated 31 October 2020 [6], 24 October 2021 [7], 5 August 2022 [8];
ii) Dr Emma de Winton, Consultant Clinical Oncologist, dated 3 December 2020 [9].
Chronology
“…Surgical OPA 10.11.15 (EDC) in context of imaging and clinical bx [biopsy] - adenocarcinoma - for liver MRI. Refer to oncology - if liver mets [metastases] for chemo, if not will need SCRT [short course radiotherapy]….”
“Mr Courtney called me to tell me that I should make an appointment to see the oncologist, Dr Emma de Winton and that I needed to have an MRI of my liver. He told me that the laparoscopic operation would be at the RUHB as it was major surgery and it would not be done privately but on the NHS.”
“I have spoken to Mr Snow to inform him of the MDT plan; this is to get an MRI of the liver to characterise the lesions in the liver first. If the lesions in the liver look benign, in view of the enlarged nodes in the mesorectum, it was thought that he would benefit from some neo-adjuvant treatment first, possibly short course radiotherapy. He therefore needs to see an oncologist and he is therefore going to see Emma de Winton privately at the Bath Clinic next Wednesday, 11th November.”
The laparoscopic TaTME surgery
Subsequent management
“Prior to his surgery … had no significant urinary symptoms that were bothersome.”
“No longer doing ISC [intermittent self-catheterisation] - managing to PU [pass urine] with a struggle.”
“Erectile dysfunction 2o [secondary] to pelvic surgery, not currently sexually active but wishes to regain this asap. Sildenafil [Viagra] issued.”
“Some success in using the vacuum pump but for various reasons finds it quite uncomfortable and not ideal. He also is not able to currently achieve an orgasm.”
“He has also never had an orgasm since his operation and whilst the parasympathetic nerves are important for erections, the sympathetic nerves are also important for ejaculation.”
“He has unfortunately lost complete sexual function and is unable to gain an erection or even achieve an ejaculation … various urologists … feel this is now permanent.”
“Has no spontaneous erections and relatively poor response to the Caverject injections.”
Transanal total mesorectal excision (TaTME)
“3.2 … With the patient under general anaesthesia and in the lithotomy position, standard laparoscopic mobilisation of the left colon and upper rectum is performed. After insertion of an operating platform into the anus, the lower rectum including the total mesorectum is mobilised in a reversed way using standard laparoscopic instruments.
3.3 The transanal part of this procedure starts with insertion of a purse-string suture to close the rectal lumen, followed by a full thickness rectotomy. After identification of the total mesorectal excision (TME) plane, the dissection progresses proximally until connection is made with the dissection from above. The specimen can be removed through the transanal platform or, if the tumour is large, through the abdomen using a small incision. Anastomosis [59] to connect the colon and the anus can be done using sutures (hand-sewn technique) or staples. When anastomosis is not possible, the patient is given a permanent stoma. When an anastomosis is done, a temporary ileostomy is usually created.”
“TaTME is an advanced complex technique that requires dedicated training and experience in TME surgery.
…
TaTME is a complex minimally invasive technique that requires advanced surgical skills as well as the knowledge and experience of recognizing anatomical planes, structures from a very different viewpoint.”
NICE guidance, March 2015
“1.1 Current evidence on the safety and efficacy of transanal total mesorectal excision (TaTME) to remove the rectum is limited in both quantity and quality. Therefore, this procedure should only be used with special arrangements for clinical governance, consent and audit or research.
1.2 Clinicians in England wishing to undertake TaTME should take the following actions:
- Inform the clinical governance leads in their NHS trusts.
- Ensure that patients understand the uncertainty about the procedure’s safety and efficacy and provide them with clear written information. In addition, the use of NICE’s information for the public is recommended.
…
1.4 Clinicians should enter details about all patients undergoing TaTME (for malignancy or a benign indication) onto the TaTME registry and review local clinical outcomes.
1.5 NICE encourages further research into TaTME of the rectum. Patient selection should be explicitly documented.”
i) “What has NICE said” [63],
“There is not much good evidence about how well this procedure works or how safe it is. It should only be used if extra care is taken to explain the risks and extra steps are put in place to record and review what happens.”
ii) “What does this mean for me?” [64],
“Your health professional should fully explain what is involved in having this procedure and discuss the possible benefits and risks with you. In particular, they should explain the uncertainty about the evidence on how likely it is to improve your symptoms and possible complications.”
iii) “Benefits and risks” [65],
“When NICE looked at the evidence, it decided that there was not enough evidence to know if the procedure is safe enough and works well enough.
…
The studies showed that the risks of transanal total mesorectal excision included:
- The doctor not being able to complete the procedure successfully using the transanal technique. …
- Problems with the connection between the anus and the colon, that allowed the contents of the bowel to leak out. …
- Strictures (narrowing) at the connection between the anus and the colon, that needed further treatment.
- A colocutaneous fistula forming. …
- Damage to the urethra (the tube that carries urine from the bladder) that needed more treatment …
- Faecal incontinence (leaking poo) after the procedure and problems with flatus (gas).
- Problems with erections after the procedure.”
National moratorium of TaTME
“The Association of Coloproctology of Great Britain and Ireland (ACPGBI) has noted with concern the results of transanal total mesorectal excision (TME) procedures reported by the Norwegian Colorectal Cancer Registry, recently published in the British Journal of Surgery [1]. The major cause for alarm has been the unexpectedly high rate of early multifocal local pelvic recurrence. These findings have led to a national moratorium on transanal TME for rectal cancer in Norway.
Other published causes for concern about this novel approach to TME include a relatively high incidence of urethral injuries occurring during both the learning curve and in established practice [2], irrespective of completion of appropriate accredited training [3], an unexpected incidence of carbon dioxide embolism [4] and high rates of morbidity during the learning curve, even within a structured national training programme [5].”
“Our recommendations are:
1 Temporary closure of the proctoring programme to new sites;
2 Extending the number of proctored cases from the current recommendation of 5–10 where sites are still completing the proctoring process;
3 Individual institutions to reconsider whether to continue transanal TME after review of local data, and subject to formal notification to local clinical governance authorities and permission of the medical director;
4 Transanal TME should only be carried out in institutions that undertake more than 40 rectal cancer resections (with rigorous exclusion of rectosigmoid cancer resections) each year, to allow sufficient ongoing experience to maintain surgical competency in the procedure;
6 Concentration of institutional experience in transanal TME by limiting performance of the procedure to two or three colorectal surgeons. Isolated practitioners are discouraged in order to ensure adequate local service delivery;
7 Use of procedure-specific enhanced patient consent;
8 Mandatory entry of data about patient demographics, patient selection, operative details and outcomes on the International Transanal TME Registry;
9 Updating the international registry with long-term oncological outcomes in patients who underwent resection for rectal cancer;
10 Independent review of the data held by the International Transanal TME Registry;
11 Assessment of the level of English and Welsh case ascertainment and data completeness in the International Transanal TME Registry through cross-referencing with NHS Digital data;
12 Collection of transanal TME as a data item in the National Bowel Cancer Audit for England and Wales, and by the Scottish Colorectal Cancer networks.”
NICE Guidance 2021
“This procedure can only be done as part of a research study. This is because there is not enough evidence to be sure how safe it is.”
“1.1 Evidence on the efficacy of transanal total mesorectal excision of the rectum is adequate. Evidence on its safety is inconsistent. It also shows the potential for major safety concerns, including damage to adjacent structures and seeding of malignancy. Therefore, this procedure should only be used in the context of research.
…
3.5 The committee noted that this is a highly challenging procedure so extensive training and mentorship is needed for it to be done safely.
3.6 The committee noted that the Association of Coloproctology of Great Britain and Ireland has published recommendations on this procedure.”
Failure to consent the Claimant
“For the purposes of this action only, it is admitted that the level of care afforded to the Claimant was substandard such that there was a breach of duty on the part of the Defendant and/or their employees, servants or agents. The Defendants stand by the open email correspondence dated 10 January 2020 sent by NHS Resolution as referred to in paragraph 69 of the Particulars of Claim. In addition, having received more detailed allegations than those set out in pre-action correspondence the Defendant formally admits that the Claimant was not counselled as to:
i. The risk of LARS …;
ii. The risk of urogenital injury …;
iii. The risk of reverting to an open procedure ….”
“For the purposes of the claim against the Trust, the Trust admits that the Claimant had not been appraised of all material risks prior to undergoing transanal total mesorectal excision (taTME) on 8 December 2015. The risks of anterior resection syndrome, urinary and sexual dysfunction were not discussed and this constitutes a breach of duty.”
i) Informed him that Mr Courtney and Mr Dalton had only performed one previous TaTME procedure and were therefore at the very beginning of their learning curve, where there is a significantly higher risk of unfavourable outcomes;
ii) Advised the Claimant of the NICE guidance, including NICE’s advice that when it looked at the evidence, it decided that there was not enough evidence to know if TaTME is safe enough and works well enough [72].
Failure to follow NICE guidance
“I agree with the judge that this departure from these guidelines is not prima facie evidence of negligence. Nevertheless, what must be right is that a clinical decision which departs from the NICE Guidelines is likely to call for an explanation of some sort.”
Procedure for introducing TaTME at Defendant’s hospital
“1.1 … Therefore, this procedure should only be used with special arrangements for clinical governance, consent and audit or research.”
“Ensuring that patients are made aware of the ‘new’ status of the procedure they are to undergo;
Preparing appropriate patient information leaflets for the new treatment/procedure”
i) A policy on information to be given to patients undergoing a TaTME, including the provision of written information, for which NICE had already provided a clear working model;
ii) A pro forma to record patient selection, which should be copied to the patient’s records;
iii) A policy to keep records of patients undergoing a TaTME and for regular reviews;
iv) A training policy to include supervision and mentoring or proctoring.
“S Dalton gave a presentation on Transanal TME (Total Mesorectal Excision) which covered a brief summary, governance, data recording on TATME registry, outcomes, risks/benefits and cost implications (copy of presentation attached).”
Training
“1.2.4 Introduction of new techniques
Introduction of new clinical interventions and surgical techniques (including equipment) that deviate significantly from established practice and are not part of an NHS local ethics committee research programme must be underpinned by rigorous clinical governance processes, having the patient’s interests as the paramount consideration. If you are introducing
new surgical techniques and technologies you should:
- Discuss the technique with colleagues who have relevant specialist experience and seek formal approval from your medical director.
- Follow local protocols with regard to obtaining approval by the local ethics committee or the local clinical governance committee. These should include the provision of evidence that the new technique is safe and that all clinical staff who plan to use the new technique will undertake relevant training, mentorship and assessment.”
“My surgical colleague and I both attended the Oxford transanal TME course and on the basis of the perfect quality of the two specimen operations we performed [on cadavers], we were advised by Mr Roel Hompes, a leading international authority on the procedure, that we should start performing it in Bath.”
Mr Meleagros: “I don't think NICE was making any comments about this sort of granular detail of the level of training and mentoring and supervision and so on. They were not making these recommendations. They're not in the NICE document.”
No mentoring
“Dr Ellis: But isn't it normal when you're embarking on a new keyhole surgical technique, whatever it is, isn't it usual that the faculty or the training facility will appoint you personal mentors?
Mr Courtney: Well, they do in some cases where people need proctoring, yes.
Dr Ellis: But you didn't have one?
Mr Courtney: No.
Dr Ellis: And nor did Mr Dalton?
Mr Courtney: No.”
No supervision
“This consensus strongly recommended … proctoring of the first cases before embarking on independent practice of TaTME. Guidance from surgeons experienced in TaTME help new adopters of the technique avoid mistakes made in the past and progress at an efficient pace with more appropriate and specialised equipment becoming widely available. To start a TaTME practice, a minimal annual volume of 10 complete dissections for cancer was agreed on.”
“Dr Ellis: So the system was that you would supervise each other effectively yes?
Mr Courtney: We went on the training course together, yes, and we both completed the training, yes.”
No documentation of patient selection
“Patient selection should be explicitly documented.”
“I think in Mr Snow’s case it [the selection process] hasn’t been documented, no.”
“Because I think there is a little bit of confusion, if you don't mind me saying, in that transanal TME is an extension to laparoscopic TME. So in transanal TME the abdominal part of the operation, the laparoscopic part, is done as far down the pelvis as you can possibly safely go and at that point where you are ceasing to make progress safely, because as the pelvis becomes very narrow, particularly towards the lower part of the pelvis, the idea is that you can then switch to a transanal approach to complete the surgery.”
“This procedure should only be used with special arrangements for clinical governance, consent and audit or research.”
Multidisciplinary team meeting
“In 2010 and 2011, the NHS National Cancer Peer Review Programme, Evidence Guide for Colorectal MDTs meetings indicated that MDTs should include a register of attendance amongst the multitude of compliance measures and components of the operational policies of an MDT. Measure 11-2D-107 indicates that MDT attendance must be recorded and evaluated. In 2015, this would likely have still been embedded in clinical practice. The team should hold its meetings weekly, record core members’ attendance and have a written procedure governing how to deal with referrals which need a treatment planning decision before the next scheduled meeting. (Guidance only - e.g. letters, emails or phone calls between certain specified members, retrospective discussion at the next scheduled meeting.)
11-2D-125 The core MDT, at their regular meetings, should agree and record individual patient's treatment plans. A record should be made of the treatment plan.
There is no evidence that national guidance was adhered to both in terms of attendance record [regarded as standard for cancer MDTs in the NHS or in relation to a treatment plan record. There is no evidence for the assertions made above as no explicit record is made. It would be useful to see what record of attendance was made at that time in the Defendant’s hospital MDT if maintained in a different file or location.”
“There is no record of the MDT decision or care plan.”
i) Most importantly, there is no record that a decision was made to carry out a TaTME, nor is there a record of a care plan. Indeed the MDT note does not state what operation was to be carried out on the Claimant.
ii) There is no record of alternative surgical procedures, namely TME carried out as a laparotomy or a laparoscopy, being considered.
iii) There is no record of the Claimant being carefully selected. Mr Courtney said that the selection of patients for TaTME was recorded in the note of the MDT, but there is no such record here.
iv) The names of the attendees are not recorded and they have not signed the note of the MDT. No separate record of attendees at the MDT has been disclosed and Mr Courtney did not say that such a record was kept in this case.
Consenting process on day of operation
“Mr Courtney: Well, we had a -- we had a conversation on the day of his surgery, which was when I consented him. I accept that the consent process was sub-standard, because it's not my usual practice to take consent on the day of surgery. My usual practice is to take consent in the clinic prior to surgery. So in this case I had - I took it on the day of surgery because it would have normally happened the week before.
Dr Ellis: And in terms of the detail of the discussion, was the discussion on the day of surgery equivalent to that which you would have had in the clinic?
Mr Courtney: It wasn't as full as I would have had, no. … It wasn't -- I didn't go through all the, or didn't have time to go through everything that I would have done had I been in the clinic.”
“Yes, totally. I never do it. I consent patients weeks in advance.”
“Mr Feeny: Mr Jenkins, you're a very experienced surgeon and sometimes in the courts we can forget about what happens in clinics and operating theatres and places like that but there is a whole team ready to go, isn't there, at that time. Everyone is geared up to start that surgery, aren't they?
Mr Jenkins: That's -- that's not an acceptable reason to put somebody through an operation.
Mr Feeny: I'm not suggesting it is. I'm just trying to explain.
Mr Jenkins: And it would not be the first time that I have cancelled major extensive surgery because I do not feel the patient is ready or has fully comprehended what is about to happen to them.
Mr Feeny: On the day --
Mr Jenkins: At the hospital I would rather take the cost of losing a day of operating than either have my conscience or some aspect trouble me that I made the wrong decision in that regard.”
Defendant’s consent form
i) The doctor not being able to complete the procedure successfully using the transanal technique. In cross-examination, Mr Courtney admitted that this was not recorded on the consent form [98] but was a material risk and should have been included in it [99].
ii) Problems with the connection between the anus and the colon, that allowed the contents of the bowel to leak out. This was recorded on the consent form.
iii) Strictures (narrowing) at the connection between the anus and the colon, requiring further treatment. In cross-examination, Mr Courtney admitted that he had not recorded this on the consent form, it was a material risk and should have been included in the consent form [100].
iv) A colocutaneous fistula forming. In cross-examination, Mr Courtney admitted that this was not recorded on the consent form but was a material risk and should have been included [101].
v) Damage to the urethra. In cross-examination, Mr Courtney admitted that this was not recorded on the consent form but was a material risk and should have been included [102].
vi) Faecal incontinence after the procedure and problems with flatus (gas). In cross-examination, Mr Courtney admitted that this was not recorded on the consent form but was a material risk and should have been included [103].
vii) Problems with erection after the procedure. In cross-examination, Mr Courtney admitted that this was not recorded on the consent form but was a material risk and should have been included [104].
“He should have informed the Claimant accordingly and he should have highlighted the advantages of TaTME (as detailed in this report) as well as the lack of evidence that TaTME is associated with a greater risk of complications compared to the conventional surgical techniques.”
“23.1 No evidence exists to date indicating superiority of this still novel technique and UK guidance [e.g. from Association of Coloproctology of Great Britain and Ireland; ACPGBI] in 2020 has recommended a “pause” on its use with more stringent recommendations for when it should be considered to be re- established.
23.2 Studies have yet to confirm any superiority although the technique is regarded as feasible and safe in correctly selected patients.”
i) As is said in the NICE Information for the Public, published 25 March 2015 [108],
“When NICE looked at the evidence, it decided that there was not enough evidence to know if the procedure is safe enough and works well enough.”
ii) Mr Meleagros’ advice that there is a lack of evidence that TaTME is associated with a greater risk of complications compared to the conventional surgical techniques puts a misleading spin on the NICE guidance. The advice of NICE was not that there was a lack of evidence that TaTME has a greater risk of complications than TME but that there is not enough evidence that TaTME is safe and works well.
iii) The advice from NICE in 2015 has been vindicated by the fact that TaTME is suspended in the UK, other than for research, because of uncertainty as to its efficacy and safety.
iv) There is no reference by Mr Meleagros in this paragraph to informing the Claimant of the seven risks which NICE identified in their 2015 interventional procedures guidance.
v) I find the above passage from Mr Meleagros’ report all the more concerning because Mr Meleagros answered in cross-examination when asked whether he would agree with the advice of NICE referred to above, “Yes” [109].
Findings as to consenting of Claimant
i) Advised that NICE had considered the evidence on the safety and efficacy of TaTME and found that it was limited in both quantity and quality and that patients needed to understand that there was uncertainty. Mr Meleagros agreed with this in cross-examination [111].
ii) Given the 2015 NICE guidance “Transanal total mesorectal excision of the rectum, information for the public”. In the joint statement of the colorectal experts, Mr Meleagros says [112],
“The Claimant should have been provided with a copy of the patient guidance.”
Mr Meleagros agreed in cross-examination that the 2015 NICE guidance should have been given to the Claimant [113].
iii) Informed that Mr Courtney was only carrying out his second TaTME. Conspicuously, in his three witness statements Mr Courtney does not say how many TaTMEs he had carried out prior to the Claimant’s operation. In the joint statement of the colorectal experts, dated 20 October 2022, Mr Meleagros says [114],
“The Claimant should have been informed as to how many TaTME procedures had been performed at the hospital.”
iv) Informed of the alternative operations he could have undergone, namely a TME laparotomy and a TME laparoscopy. Mr Jenkins, Consultant Colorectal Surgeon, says in his report dated February 2022 [115],
“55. It is also clear that Mr Snow was not offered reasonable alternatives including open TME surgery, laparoscopic TME surgery or no treatment, for example.
55.1. This was a breach of duty.”
Mr Meleagros says in his report, dated 30 March 2022, at paragraph 1.10 [116],
“I agree that the Claimant should have been advised of the options, namely open anterior resection (AR) with TME (total mesorectal excision), laparoscopic AR + TME and TaTME.”
v) Informed of all of the risks identified by NICE in their 2015 interventional procedures guidance at section 5, and in particular the risks referred to at paragraph 110 (ii), (iii), (iv) above.
How Mr Courtney says he would have consented Claimant on 11 November 2015
i) Informing the Claimant, in accordance with the NICE guidance, of “the uncertainty about the evidence on how likely it is to improve your symptoms and possible complications” [118];
ii) Providing the Claimant with the 2015 NICE guidance “Transanal total mesorectal excision of the rectum, information for the public”;
iii) Ensuring, in accordance with the NICE guidance, that patients understand the uncertainty about TaTME’s safety and efficacy;
iv) Advising the Claimant that he had only carried out one previous TaTME and that the learning curve had been strongly associated with increased risk of complications not normally associated with a TME;
v) Advising of the material risk of damage to the urethra;
vi) The risk of erectile dysfunction.
“I would have made clear to him that those risks are risks of the need for surgery to remove the rectum due to cancer, not of the proposed approach.”
That is contrary to the NICE guidance that these are risks associated with a TaTME and is yet another example of him intentionally misrepresenting the NICE guidance and downplaying the risks of TaTME. It is clear from Mr Courtney’s written and oral evidence that he does not accept the guidance of NICE on TaTME and as a consequence did not follow it.
Operation note of 8 December 2015
“…I: 10mm umb[ilical] port, 12mm RIF [right iliac fossa] 5mm epigastric and left ports.
P: medial to lateral dissection, IMV [inferior mesenteric vein] and IMA [inferior mesenteric artery] taken with hemolock clips. Splenic flexure fully mobilised. Lateral dissection continued to pelvic brim.
1 nylon purse string inserted some faecal leakage, washed out ++. Transanal gel path port inserted, TATME dissection performed with diathermy to join abdominal dissection. Tethering at 5 o’clock and difficult dissection. Some lap abdominal assistance.
Specimen delivered through Alexis [wound retractor/protector] in extended midline port incision, sigmoid descending junction divided and colon delivered to anal canal.
Hand sewn colo-anal anastomosis with 30 Maxon interrupted tension free good blood supply.
Defunctioning ileostomy in RIF.
PDS loop 1 to fascia, clips to skin.
14G drain to pelvis… .”
“Dr Ellis: Bearing in mind the special conditions imposed by NICE on college governance consent record keeping, it’s surprising, isn’t it, that an operation lasting nearly nine hours has been reduced to so few lines. It reads rather like an uncomplicated laparoscopic appendicectomy?
Mr Courtney: Yes.
Dr Ellis: It’s not adequate for governance purposes or research and investigation, is it?
Mr Courtney: Well, it’s not a long enough operation note, yes, I agree.
Judge Roberts: Sorry, it’s not.
Mr Courtney: It’s not a long enough operation note, I agree.
…
Dr Ellis: So it’s accepted it’s not detailed enough.
Mr Courtney: Yes.
Dr Ellis: For number 2?
Mr Courtney: Yes.
Dr Ellis: When special conditions are imposed, but it’s startling, isn’t it, bearing in mind what we know about potential risks including pelvic nerve injury, there is no record, is there, that any of the relevant nerves were ever identified or preserved?
Mr Courtney: There’s no record of it, no.
Dr Ellis: No. And what probably happened, didn’t it, is that during the part described as a difficult dissection, this is where those pelvic nerves, which presumably hadn't been identified and preserved, were injured?
Mr Courtney: I presume so, yes.”
“70. Insufficient detail is provided [in the operation record] to understand the planes that were actually encountered during Mr Snow’s operation and whether nerves were identified
…
Blood loss is also not clarified.
74. The operation duration would be regarded by most colorectal surgeons, and certainly rectal cancer surgeons, as being excessive but may reflect the procedural difficulties encountered that are not well documented or assessable from the operation note.”
“The duration of each of the separate parts of the operation is not documented in the theatre records. In particular, the time taken for preparation, for the abdominal laparoscopic procedure, for the TaTME procedure, the anastomosis, the formation of loop ileostomy and abdominal closure are not recorded in the documents provided.”
“There is a view in the medical profession that they spend too much of their time filling in forms and not enough time seeing patients. All I can say, my experience of these matters is that the documentation in this case is not uniquely of a standard which one doesn’t see in relation to these cases. There is a huge amount of documentation now required in case notes and that comment is made, well we’re not here to fill in forms, we’re here to deal with patients.”
FACTUAL CAUSATION
“Had Mr Courtney explained that I was to undergo a TaTME procedure, even without knowing it was a new procedure, if he had explained what I now understand to be the elevated risks (relative to conventional bowel surgery) with urogenital injury, impotence and LARS, I would not have let him operate on me. Had I known that there was not much good evidence as to how safe the procedure was; the greater risk of complications generally during the local surgeons ‘learning curve’; the absence of long-term statistically significant local evidence on safety and efficacy compared with established treatments; the possibility of undergoing a very lengthy operation; the risks associated with excision of the whole rectum with a very low join and distal hand sewn purse string suture; and the prolonged period of sphincter stretch with the anal device and possible long-term consequence, I would not have let him, or anyone else, proceed, even if I had found out on the date of the operation.”
“Had we known about other treatment options and the risks associated with this new procedure and that Malcolm was only the second taTME patient of the RUH, he would definitely have declined the operation on the 8th December 2015. ”
“55. It is also clear that Mr Snow was not offered reasonable alternatives including open TME surgery, laparoscopic TME surgery or no treatment, for example.
55.1. This was a breach of duty.
55.2. This is also in spite of Mr Courtney’s experience in laparoscopic TME which would have been a suitable alternative to offer.
56. The issue of whether Mr Snow would have opted for one of these alternatives in favour of TaTME is for the court to determine. However, in my opinion a hypothetical reasonable patient who had been properly appraised of the relative benefits and relative risks of TaTME and the alternative procedures in 2015 is unlikely to have opted for TaTME at the RUHB.”
“In the circumstances, it is, on the Defendants’ case, overwhelmingly likely that even with fuller information the Claimant would have accepted Mr Courtney’s advice to undergo a TaTME in particular, because of the risk of colostomy from any other procedure.”
“2.34 In my opinion, based on clinical experience, even if the Claimant had been warned preoperatively of the risks of urinary and sexual dysfunction and anterior resection syndrome, he would have consented to the surgery because the alternative would have been far worse and totally unacceptable to the Claimant.”
Issues of fact
“(a) The significant issues of fact in relation to the Claimant’s discussions with Mr Courtney on 4 and 5 November 2015, in particular as to:
(i) The detail of discussion which took place on 4 and 5 November 2015;
(ii) Whether Mr Courtney stated on either date that he would only remove part of the rectum;
(iii) Whether Mr Courtney told the Claimant that he did not need to attend the appointment on 10 November.”
i) Whether Mr Courtney told the Claimant to cancel the appointment for 10 November 2015;
ii) Whether Mr Courtney and Mr Dalton at any stage were operating in the wrong plane.
Credibility of Mr Courtney
i) The 2015 guidance by NICE on TaTME;
ii) Any of the medical literature relating to TaTME.
i) NICE said at paragraph 1.2 [132] “Ensure that patients understand the uncertainty about the procedure’s safety and efficacy”. Mr Courtney failed to do so on 8 December 2015 and when he says at paragraph 10 of his witness statement, dated 31 October 2020 [133], what he would have told the Claimant on 11 November 2015 if he had seen him then, he again fails to say that he would have advised the Claimant about the uncertainty about TaTME’s safety and efficacy. He provided no explanation in his three witness statements or in his oral evidence for departing from the NICE guidance.
ii) NICE said at paragraph 2, “Provide [patients] with clear written information”. Mr Courtney provided no written information to the Claimant. He does not say in his witness statement of 31 October 2020 that he would have given the Claimant this written information if he had seen him on 11 November 2015. The Defendant’s colorectal expert, Mr Meleagros, said that the Claimant should have been provided with written information [134].
iii) NICE said “This procedure should only be used with special arrangements for clinical governance, consent and audit or research”. Mr Courtney makes no reference in his witness statements or oral evidence to any special arrangements for clinical governance, consent and audit or research at the Hospital. The Defendant has not disclosed any documents showing special arrangements for clinical governance, consent and audit or research. The only document disclosed are the slides from a presentation given by Mr Dalton on TaTME [135].
iv) NICE said at paragraph 1.5, “Patient selection should be explicitly documented” [136]. Mr Courtney did not document the Claimant’s selection. In cross-examination, Mr Courtney said he documented patient selection in every other TaTME he performed. The Defendant provided no documentary evidence to support that. Furthermore, Mr Courtney offered no explanation for why, if he did document every other patient’s selection, he did not do so in the Claimant’s case.
v) Mr Courtney’s evidence shows that, contrary to the NICE guidance, Mr Courtney considered a TaTME to be only a variation on a TME. He said in cross-examination that, “We did most of the operation in the standard fashion and only when we couldn’t proceed safely laparoscopically is when we started doing the transanal approach.
vi) In contrast to the NICE guidance that,
“1.1 Current evidence on the safety and efficacy of transanal total mesorectal excision (TaTME) to remove the rectum is limited in both quantity and quality. Therefore, this procedure should only be used with special arrangements for clinical governance, consent and audit or research.”
Mr Courtney says at paragraph 10 of his first witness statement, dated 31 October 2020, that he would have made it clear to the Claimant that these risks are risks of the need for surgery to remove the rectum, not of the TaTME [137]. I find that this is a misrepresentation of the NICE guidance.
“It should be noted that TaTME is still being performed worldwide and the procedure was suspended at the Trust pending further investigation of oncological safety, rather than due to the risk of any complications.”
i) He wrongly states that TaTME was suspended pending further investigation of oncological safety, rather than due to the risk of any complications. The 2020 paper by the Association of Coloproctology of Great Britain and Ireland [139] states that there were other serious concerns alongside that of oncological safety, including a relatively high incidence of urethral injuries occurring during both the learning curve and in established practice. I accept Mr Jenkins’ evidence that such injuries result from surgeons wrongly going out of the mesorectal fascia plane, as the Claimant alleges happened in the present case.
ii) In his third statement, dated 5 August 2022, he does not say that NICE said in their 2021 guidance [140], and it remains the position that,
“1.1 Evidence on the efficacy of transanal total mesorectal excision of the rectum is adequate. Evidence on its safety is inconsistent. It also shows the potential for major safety concerns, including damage to adjacent structures and seeding of malignancy. Therefore, this procedure should only be used in the context of research.”
Credibility of Claimant
“The Claimant has over a period of time developed a very clear animus against Mr Courtney. The Claimant has sought to blame and indeed vilify Mr Courtney in a way that would not be consistent with a reasonable understanding of the evidence. … The Claimant’s case [on Mr Courtney cancelling the appointment on 10 November 2015] has to be understood in the context of his animus to Mr Courtney.”
Claimant’s consultation with Mr Courtney on 4 November 2015
i) He did not have access to any of the Claimant’s scans or notes at the BMI Bath Clinic.
ii) He could not discuss specifics with the Claimant at the consultation.
iii) The Claimant was very anxious and upset and shouting at him.
iv) The Claimant was adamant that he was not prepared to accept a permanent stoma.
“Diagnosis:
- Mid rectal tumour - biopsies highly suspicious but not diagnostic of adenocarcinoma
- MRI staging T3b N2b Mx, CRM sfe, EMVI-ve
- CT scan - cirrhotic liver. Extensive small liver nodules ? regenerative/dysplastic nodules related to the patient’s cirrhosis rather than colorectal metastases”
“Dr Ellis: When you say in your statement ‘I didn’t have access to the imaging’, that’s not true, is it? You had access to the reports and that’s why they’re in the letter?
Mr Courtney: Well, I had access to the CT. The MRI is often not reported until the time of the MDT...
Dr Ellis: I understand. So you accept that your statement is incorrect?
Mr Courtney: Yes. It would read incorrect, yes
…
Dr Ellis: So your statement is factually wrong in that regard?
Mr Courtney: Yes, well I think this was made seven years later.
Dr Ellis. Quite. And memory fades?
Mr Courtney: Yes. So I think, you know, I see 30 to 40 patients in clinic a week, so I think remembering a consultation seven years ago is difficult…”
“6. I recall Mr Courtney said I would need a temporary stoma and a bag for a few months but it would be reversed afterwards once the join in my bowel had healed. Mr Courtney explained that the CT scan showed liver abnormalities, which made detecting cancer more difficult, so I would need another MRI scan, focused on my liver. He said that he would take a biopsy of my liver during the operation to establish beyond doubt what the abnormalities were (metastases or cirrhosis). He also said that there would be a multi-disciplinary team meeting (MDT) the next day when they would discuss my case. I asked if I could attend, I was told I couldn’t, but I understood he would be there along with an oncologist and a radiographer. Mr Courtney said that he would telephone me the next day to let me know the outcome of the MDT. I asked if the operation would happen sooner if I used my private medical insurance to have it at the BMI Bath clinic. He replied that he would let me know when he spoke to me the next day.
…
9. The notes I made following the consultation on 4th Nov 2015 (Exhibit MS 1) [146] which recorded that: my pain and bleeding (from my anus) had worsened; Mr Courtney said that the CEA bowel cancer marker was normal (I later found that it was high). There was discussion about laparoscopic surgery, primarily that the recovery time would be shorter Mr Courtney said it would not be unheard of people returning to work after a laparoscopic surgery within 6 to 8 weeks. He did not mention any risks with the operation, he did not discuss any alternatives other than laparoscopic surgery. I remember telling him that my mother had had bowel cancer and had made a full recovery from her operation. I was absolutely convinced that I was having a partial removal of my rectum.”
i) Denied that he was agitated at the consultation on 4 November 2015 and said that he was calm [147].
ii) Said that he did not say he was not prepared to accept a permanent stoma and that there was no such discussion [148]:
“Mr Feeny: … The first is this: that you at all times have been very keen to avoid a colostomy, haven’t you, a permanent colostomy?
Mr Snow: No. At that time, I wasn’t. At that time it wasn’t really discussed, because I was going to have a temporary colostomy.
...
I read that in his statement and I’m just saying no, that did not happen.”
iii) Said that he thought the operation he was having was a partial removal of the rectum and that the tumour would be removed laparoscopically [149].
Findings as to Claimant’s consultation with Mr Courtney on 4 November 2015
“22. … I did not have a chance [on 8 December 2015] to read what was written on the Consent Form. It was only much later that I had an opportunity to read my medical records when I saw that he had written ‘Trans-anal Total Mesorectal Excision’.
23. I was not aware at the time that I was asked to consent to a TaTME operation. I had never heard of this operation, it had never been discussed and certainly the risks associated with this procedure had not been mentioned at all. In any case, the handwriting of Mr Courtney is not legible to a lay person, so even if I had been shown the consent form I would not have been able to read it.”
Telephone conversation on 5 November 2015
“I recall that the Claimant was adamant that he wasn’t prepared to accept a permanent stoma and so a transanal approach to the surgery (TaTME) was the best way to achieve the necessary surgical outcome of full clearance of cancer, and try to meet that aim.”
“3. I explained that given his high BMI (32) and narrow male pelvis that we would utilise a relatively new, and licenced, access technique called a trans-anal total mesorectal excision (TaTME) to aid safely removing the rectum. I explained that Mr Dalton and I had been trained in this relatively new technique and that I would elaborate with him when I saw him in clinic face-to-face the following week at the RUH. Mr Snow cancelled this clinic appointment.”
“15. I recall the next day (Wednesday 5th Nov 2015) having detailed discussions at work, allocating my current task list to others, with a best return date of 1st Feb 2016 and a worst case return date around end of March 2016. Mr Courtney called me to tell me that I should make an appointment to see the oncologist, Dr Emma de Winton and that I needed to have an MRI of my liver. He told me that the laparoscopic operation would be at the RUHB as it was major surgery and it would not be done privately but on the NHS. He advised that I did not need to attend the appointment already arranged for Tuesday 10th Nov because I had seen him the day before. I telephoned the RUHB to cancel the appointment, as advised by Mr Courtney, which I noted in my diary. I did not default the appointment on 10th November as alleged by RUHB. There was no logical reason why I would have missed the appointment other than acting upon Mr Courtney’s advice. At no time was I told that the appointment on the 10th was ‘planned in order to discuss the Claimant’s proposed treatment’. Had I known that ‘proposed treatment’ was up for discussion, I would definitely have attended the appointment.”
“Cancelled as saw him privately last Wed.”
“Mr Feeny: In terms of not going to the appointment on 10 November, how did it come about that you didn’t go to that appointment?
Claimant: Because I asked him if I needed to go. And he - that appointment was made, as I said earlier, through the NHS booking and because I saw him privately I asked if I needed to go to that appointment and he said I didn’t need to go.
Mr Feeny: Sorry, when did that conversation take place?
Claimant: When he phoned with the MDT results, on 5 November.”
Findings as to telephone conversation on 5 November 2015
i) The information referred to at paragraph 3 of Mr Courtney’s third witness statement was not included in Mr Courtney’s first witness statement, dated 31 October 2020, where he also gave an account of the telephone call of 5 November 2015 [157]. Nor was it included in his second witness statement, dated 24 October 2021 [158].
ii) Mr Courtney never provided this account until his third witness statement, dated 5 August 2022, nearly seven years after the telephone call, and 2½ months prior to trial. When he agreed in cross-examination that he was wrong to have stated that on 4 November 2015 he did not have access to the Claimant’s CT scan, he replied [159], “I see 30 to 40 patients in clinic a week, so I think remembering a consultation seven years ago is difficult…”. I do not find it credible that Mr Courtney’s memory of a telephone call on 5 November 2015, has significantly improved over 6½ years after the event and after disclosure of the Claimant’s witness statement.
iii) The Claimant had put the Defendant on notice at paragraph 38 of the amended Particulars of Claim [160], dated March 2020, that his case was that he was not seen preoperatively by any member of the Hospital surgical team in order to discuss the proposed surgical procedure, reasonable alternative procedures, and their respective potential benefits and potential risks. If the information at paragraph 3 of Mr Courtney’s third witness statement had been true, it would have been included in Mr Courtney’s first witness statement.
iv) None of this information is recorded in Mr Courtney’s contemporaneous letter to the Claimant’s GP, dated 5 November 2015 [161]. It was critical information to share with the GP. I find that it is inconceivable that Mr Courtney would have omitted this information from the letter, which only says [162],
“I have spoken to Mr Snow to inform him of the MDT plan; this is to get an MRI of the liver to characterise the lesions in the liver first. If the lesions in the liver look benign, in view of the enlarged nodes in the mesorectum, it was thought that he would benefit from some neo-adjuvant treatment, first short-course radiotherapy. He therefore needs to see an oncologist and he is therefore going to see Emma de Winton privately at the Bath Clinic, next Wednesday 11th November.”
v) If Mr Courtney had explained to the Claimant that he would perform a TaTME and the reasons for selecting this procedure, he would have completed the written selection documentation referred to by NICE. He did not do so.
i) I found the Claimant a far more reliable witness than Mr Courtney.
ii) The Claimant’s account that he asked Mr Courtney if he needed to attend the appointment on 10 November 2015 as he had seen him privately and that Mr Courtney told him that he did not, is confirmed by the Claimant’s contemporaneous diary entry on 10 November 2015.
iii) The Claimant is by nature conscientious and thorough. He prepared notes with questions before meetings with his treating doctors and notes after meetings. Far from cancelling appointments, the Claimant asked Mr Courtney if he could attend the MDT meeting on 5 November 2015. I find it highly unlikely that he would have cancelled the appointment of his own volition.
Timing of surgery
“(a) There was urgency in the Claimant undergoing surgery:
(i) The government set a target of treatment within 62 days.”
i) On referral on 29 September 2015, the Claimant’s General Practitioner noted [166],
"This man has significant health-related anxiety. He finds waiting intolerable. This is tricky to manage, so early investigations is (sic) crucial and would be appreciated."
ii) Dr Robinson, Specialist Registrar in Respiratory Medicine, wrote after seeing the Claimant on 22 October 2015 [167],
"He was contacted at short notice due to a cancellation which coincided with being two days after his colonoscopy for investigation of his rectal bleeding. Mr Snow was understandably extremely anxious at the appointment in relation to the results of his colonoscopy, but I confirmed with him that this was by pure coincidence only."
iii) In Mr Courtney’s letter of 5 November 2015 he wrote:
“He does have an appointment with me next week at the RUH, but because of increasing anxiety he decided to come and see me sooner.”
“Dr Jenkins: It doesn’t necessarily mean that the surgery has to be done within 31 days. In the real world interpretation of that. … It doesn’t reflect any oncological urgency. It’s a metric to ensure the patients are processed in a suitable timeframe.
…
The first aspect is if a patient chooses to defer treatment, that is entirely their choice and even if it might yield what is called a breach then the trust must accept that. They cannot coerce a patient into treatment, be that earlier or otherwise. That’s the first thing.
The second thing is when it comes to short course radiotherapy, there has been a historical concern regarding morbidity and if it is delayed beyond a week, although the timeframes are very broad across the NHS, then that may induce a worsening of outcome. There are data from NHS England that look at time to surgery from short course radiotherapy and actually find little detriment to clinical outcome, post-surgical outcome by waiting a couple of weeks, up to three weeks, four weeks.”
Finding as to timing of surgery
Conclusion as to factual causation
“… the Defendant’s case is that it is highly improbable that Mr Snow would not have proceeded surgery as advised by Mr Courtney on 8 December 2015:
(a) As Mr Snow acknowledged, he was not thinking clearly and rationally at this stage. …
(b) His primary concern at this time was understandably to have treatment as soon as possible ....
(c) Mr Courtney, subject to referring to the NICE guidance, could and would have reasonably advised the Claimant that in Mr Courtney's opinion TaTME was the most suitable procedure for the Claimant.
(d) The Claimant acknowledges that he had complete trust in Mr Courtney at this stage.”
MEDICAL CAUSATION
i) Reports of Mr John Jenkins, Consultant Colorectal Surgeon:
a) Liability and causation report, dated February 2022 [171];
b) Condition and prognosis report, dated 29 March 2022 [172];
ii) Report of Mr John Reynard, Consultant Urological Surgeon, dated February 2022 [173];
iii) Report of Dr David Burling, Consultant Radiologist, dated February 2022 [174];
iv) Report of Dr Trevor Turner, Consultant Psychiatrist, dated February 2022 [175].
i) Reports of Mr Luke Meleagros, Consultant Colorectal Surgeon:
a) Liability and causation report, dated 30 March 2022 [176];
b) Condition and prognosis report, dated 9 July 2022 [177];
ii) Reports of Professor Krishna Sethia, Consultant Urologist:
a) Liability and causation report, dated 21 December 2021 [178];
b) Condition and prognosis report, dated July 2022 [179];
iii) Report of Dr David Scullion, Consultant Radiologist, dated August 2022 [180];
iv) Report of Dr Shazad Amin, Consultant Psychiatrist, dated 28 July 2022 [181].
i) Joint colorectal expert statement, dated 14 October 2022 [182] and 20 October 2022 [183];
ii) Joint urology expert statement, dated September 2022 [184];
iii) Joint radiology expert statement, dated 5 September 2022 [185], 20 October 2022 [186] and 24 October 2022 [187];
iv) Joint psychiatry expert statement, dated 20 September 2022 [188].
Credibility
“…The task of the Court is to see beyond stylistic blemishes and to concentrate upon the pith and substance of the expert opinion and to then evaluate its content against the evidence as a whole and thereby to assess its logic. If on analysis of the report as a whole the opinion conveyed is from a person of real experience, exhibiting competence and respectability, and it is consistent with the surrounding evidence, and of course internally logical, this is an opinion to which a judge should attach considerable weight.”
Mr Jenkins
“I think it would be difficult to prove a difference in terms of quality of life”
Mr Meleagros
i) I found Mr Meleagros’ evidence that the need for training, supervision and mentoring in respect of TaTME was not known until 2018 unsustainable (see paragraph 82 above). The need for training, supervision and mentoring when introducing a new surgical procedure is stated in terms in the Royal College of Surgeons of England’s ‘Good Surgical Practice’, published in 2014, and is common sense.
ii) I found Mr Meleagros’ evidence as to what advice should have been given to the Claimant when he was consented in December 2015 failed to reflect the 2015 NICE guidance (see paragraph 108 above). He provided no adequate reason for departing from NICE’s advice. I bear in mind that NICE’s concerns in 2015 were validated by the fact that in 2021 TaTMEs were suspended, with the procedure now only used in this country in the context of research.
iii) I find below that Mr Meleagros’ attempt to go behind the consultant radiologists’ agreement that the Claimant’s tumour was mid-rectal, not low, was not within his expertise and was unsustainable (see paragraphs 194 to 196 below).
iv) It will be seen from paragraphs 241 to 244 below that I reject Mr Meleagros’ evidence that only the Japanese carry out autonomic nerve preservation and prefer Mr Jenkins’ evidence. The medical literature shows that autonomic nerve preservation has been carried out for thirty years all around the world, including in the UK.
“There is no evidence of differences in the surgical risks between open or laparoscopic AR + TME and TaTME, or in the duration or severity of postoperative symptoms.”
This statement would only be valid if Mr Courtney and Mr Dalton were experienced in performing TaTME procedures, as they were in performing open or laparoscopic TMEs. That was not the case. Mr Courtney said in cross-examination that he had carried out hundreds of TMEs [191] . However, he had only carried out one TaTME prior to the Claimant’s operation.
“Please confirm that you have read the statements of case, the factual witness statements, each other’s reports and the literature.”
“Yes, so once again I admit that none of the article copies were sent to me. … I was always under the impression that each side discloses literature to the other side.”
“Dr Ellis: I'm sorry, you're not answering the question again.
Mr Meleagros: -- with the exception of urethral injury.
Dr Ellis: You're not answering the question again.”
“The cancer extended below this point due to its pedunculated nature to 7.1-7.6cm from the anal verge.”
He was asked if this was correct and said that it was. There was then the following exchange [197]:
“Dr Ellis: No. Now, pedunculated means on a stalk. Yes?
Mr Meleagros: It could mean that but the stalk could be broad.
Dr Ellis: I'm sorry, the dictionary definition of a peduncle, as we all know, is a stalk. This hasn't got a peduncle, a stalk?
Mr Meleagros: You're right, it hasn't. Wrong use of the word.”
Conclusion as to credibility of colorectal experts
Overview of medical causation
i) Would the Claimant have been suitable candidate for TME?
ii) The location of the tumour;
iii) Abdomino-perineal excision of rectum (APER);
iv) Did the Claimant have a narrow pelvis?
v) Early learning curve for TaTME;
vi) Total impotence, loss of ejaculatory function and anorgasmia;
vii) Urinary urgency and incontinence;
viii) LARS;
ix) Injury to internal anal sphincter.
Would Claimant have been suitable candidate for TME?
“The decision to offer Total Mesorectal Excision [TME] was entirely valid and would be regarded as the surgical ‘gold standard’ for removing mid and distal [lower] rectal cancers where restoration of bowel continuity [bowel join or anastomosis] is regarded as appropriate. This would have been the case in Mr Snow.”
“LM will say as follows. The rectal cancer was above the pelvic floor and it did not infiltrate the anal sphincters. Therefore, based on this criteria, open anterior resection with TME would have been feasible. …
JTJ Opinion: The tumour was in the mid rectum and TME would be regarded as the standard approach in this circumstance and both open and lap TME were offered by the Defendant’s Hospital at that time. It would be presumed that in the absence of taTME that either option would have been offered to the Claimant. Please note at no point was APER considered or mentioned as an outcome to the Claimant neither as an option for a mid-rectal cancer nor as an outcome after commencement of a planned TME, by any of the approaches available at that time.”
“Because the issue has arisen and that’s why -- I don’t think it’s important because we are agreed that a TME should have been carried out in any event regardless of the precise definition of whether it was low or mid low or mid. We are agreed that the same operation should have taken place but because this issue arose - -.”
Location of tumour
“Diagnosis:
Mid-rectal tumour.
…
Essentially it would appear that he has a bulky mid-rectal tumour.”
“The tumour was positioned very low in the rectum”.
i) They say in their joint statement dated 5 September 2022 [206],
“The MRI scan shows a mid-rectal cancer with height above anal canal as documented in the radiology expert witness reports.”
ii) They say in their joint statement dated 20 October 2022 [207],
“3. In which third of the rectum:
a. Is the origin of the tumour in the wall?
Mid rectum
b. Is the most distal intraluminal part?
Mid rectum.
…
5. Do your answers to the above questions cause you to alter your agreement (JS Q2) that the tumour was mid-rectal based upon the pre-operative MRI scan?
No.”
i) By Mr Meleagros [208],
“Given that the cancer was 4.5-4.6cm above the anorectal junction (based on wall attachment) or 3cm above anorectal junction (based on luminal distal extension) in my opinion it could be classified as a mid/low rectal cancer.
However irrespective of the precise classification of the cancer as mid rectal or low rectal the surgical treatment would have been the same, namely in the form of TME (total mesorectal excision) with resection of most or the entire rectum leaving either a very short cuff of distal rectum for anastomosis or resulting in an anastomosis at the anorectal junction or just above it, namely a coloanal anastomosis.”
ii) By Mr Jenkins [209],
“At the time of diagnosis and assessment by the Defendant’s Trust team the conclusion was that the rectal cancer was in the ‘mid rectum’ on CT, although on the MRI was recorded as ‘mid-distal’ rectum implying that the lesion was on the boundary between the mid and lower rectum with the greatest part of the lesion lying in the mid rectum and that the lesion in itself was not sited or originating in the low [or distal] rectum. The radiology reassessment by Dr Burling reflects the likely site of the lesion as the mid rectum and as the tumour is agreed to be polypoidal and the base or site of origin is in the area generally regarded as the mid rectum. The polypoidal or ‘mushroom-like’ nature of the rectal cancer means that a significant component of the lesion lies out with the wall and would not be used to determine the true height of the lesion which would be better represented by the distance to the ‘stalk’ of the rectal cancer. Therefore, in reference to LM opinion above, the lesion is better defined as 4.5cm from the anorectal junction than 3cm in any of the post treatment opinions given to Mr Snow previously and I would dispute the opinion of Mr Antoniou as a result. … The English National Low Rectal Cancer Development Programme [LOREC] defined a low rectal cancer ‘on MRI-based anatomical definition as where the mesorectum tapers at the origin of the levators, at the pelvic sidewall. This usually corresponds to a measurement of within 6 centimetres of the anal verge’ … Taken together, even at its lowest point this rectal cancer would not have been regarded by this definition as a low [or distal] rectal cancer. There is agreement that Total Mesorectal Excision [TME] or low anterior resection would be the most suitable surgical option.
…
This was a mid-rectal cancer entirely suited oncologically and technically to TME be that open or laparoscopic.”
“The other thing that I’m not clear when it comes to our radiology colleagues’ reporting is whether the distance is measured in the sagittal plane, the side view, where they draw these two lines in the anal canal and then another line at an angle in the rectum, or whether the distance is measured as a single perpendicular line from where they think the anal verge is to the tumour. And that distance would clearly be shorter because it is the hypotenuse of a right angle triangle.
…
So all in all I’m not trying to make a case that I disagree with any definitions of low, middle or rectal; I’m just saying that the whole thing is a lot more nuanced than that and as practising surgeons, we’re more interested as to whether we have sufficient tissue below the lower border of the cancer to allow us to perform a so-called sphincter saving resection and that’s why inadvertently I use the term low, not necessarily to apply to the definition of low rectum but to apply the definition that in the eyes of a practising colorectal surgeon such as myself, this cancer is low.
…
Dr Ellis: But all these qualifications about which measuring points were used, whether you can see the skin around the anal canal entrance or not, where the height of the tumour is, is it from a sagittal line or a perpendicular, from a hypotenuse, et cetera et cetera. This wasn’t something that suddenly dawned on you when you came to court yesterday and read the report about pelvimetry, was it?
Mr Meleagros: Actually it was, unfortunately. I realised when I was speaking to Dr Scullion outside court yesterday morning when he arrived.
Dr Ellis: So did you tell him about your concerns?
Mr Meleagros: Yes.
Dr Ellis: The inaccuracy of the measurements?
Mr Meleagros: Yes, I did in our conversation but as you rightly point out I am not a radiologist.”
“I don’t think it’s important because we are agreed that a TME should have been carried out in any event regardless of the precise definition of whether it was low or mid low or mid.”
Findings as to whether tumour was mid-rectal or low-rectal
i) It is common ground that the location of the tumour lies within the expertise of the consultant radiologists. Dr Burling and Dr Scullion are in agreement that based upon the scanning, the tumour was mid-rectal.
ii) Mr Meleagros conceded that the issue of the position of the tumour in the rectum was not within his expertise.
iii) Notwithstanding this, he sought to undermine the radiologists’ evidence with a scattergun approach of saying that the measurements of a low tumour could be taken from numerous different points: a sagittal line, a perpendicular, a hypotenuse etc. He said that this approach had only “dawned” on him outside Court when speaking to Dr Scullion. I accept Dr Ellis’ submission in his closing submissions at paragraph 8b that Mr Meleagros’ ‘definition’ is contrary to the medically recognised definition, by which tumours are classified according to which third of the rectum they are situated in.
iv) Although Mr Meleagros said he discussed his ‘definition’ with Dr Scullion, the Defendant’s radiologist, before the latter gave evidence, I find it of significance that Dr Scullion did not seek to qualify his agreement in the radiologists’ joint statement that the tumour was mid-rectum or refer to any discussion with Mr Meleagros when he gave evidence to the Court.
v) Mr Meleagros’ ‘definitions’ were not put to the Claimant’s radiologist, Dr Burling, in cross-examination.
vi) Contrary to Mr Meleagros’ opinion that whether the cancer was mid-or low-rectum was of no importance, it was of importance. I accept Mr Jenkins’ evidence in cross-examination that [212],
“Ultra lows are recognised in the surgical community to have a poorer outcome compared to standard TME which would be defined as a low anterior resection”
Abdomino-Perineal Excision of Rectum (APER)
(iii) In the Claimant’s case, TME was not an option due to the location of the tumour (10cm from the anal verge), a bulky tumour, a male pelvis and obesity (BMI 32). Proceeding with a TME would on the balance of probabilities have resulted in:
(a) the need to convert to APER;”
“26 I note that data from the National Bowel Cancer Audit [NBOCA] for the years 2015-2018, show that the RBUH colorectal service has a non-restoration rate/APER rate higher than the national average reaching; nearly 40% in some years brackets [nboca.org.uk).
26.1 Whilst such data are highly nuanced in interpretation, RBUH performs less than 40 rectal cancer operations per annum with a higher APER rate and hence lower restoration rate than the national average.
26.2 APER refers to Abdomino-Perineal Excision of Rectum and is an operation that removes the rectum and anus leading the patient with a permanent colostomy. In such an instance the procedure would also be described as non-restorative i.e. the continuity of the bowel has not been maintained or is not achievable.
26.3 In my opinion, units with higher rates of APER may not have developed expertise in managing low tumours with ‘standard’ TME surgery and hence may seek alternatives such as taTME to remedy this.”
“With Lap TME the likelihood of conversion to APER intra-operatively would be highly unlikely and if it was felt to be an outcome of genuine concern or likelihood then it would have been explicitly stated to the patient in the preparatory phase. This was not the case and contrary evidence is not presented. However, nothing can be stated to be completely avoidable, nevertheless, the need for conversion would be extremely rare. The Defendant’s Trust were experienced in APER [based on NBOCA data from 2015] and it would be presumed they would identify preoperatively those most suited for APER. … There would be no oncological requirement for abdomino-perineal excision [APER] based on the tumour location.”
“2.11 … The only option, if TaTME was to be avoided, was APER. …
…
2.21 Thereafter, in the scenario proposed by the Claimant, the surgeon would have attempted laparoscopic AR +TME with TaTME but would, on the balance of probabilities, have failed due to technical reasons. On the balance of probabilities, the surgery would have been converted to APER and therefore, the Claimant would have had a permanent colostomy and would have been at a slightly higher risk of sexual dysfunction.”
“Dr Ellis: On a balance of probabilities, I know you prefer to avoid that, it was highly unlikely that an experienced laparoscopic surgeon doing it their usual way from the top down, highly unlikely that this would have been converted to an APER and colostomy, isn't it? It's less than 50 per cent risk?
Mr Meleagros: It’s less than 50 per cent, yes, …”
Findings as to APER
Did Claimant have a narrow pelvis?
“I think because of his narrow pelvis and fatty mesorectum, myself and Mr Dalton are both of the agreement that if we hadn't done a transanal TME he would have probably ended up with a AP resection because access to the lower rectum was extremely difficult.”
“Dr Ellis: There’s no evidence before the court as to either what the range of a normal male pelvis is or what the dimensions were in this case?
Mr Courtney: No.”
“5. What is the diameter of pelvic outlet?
DS and DB: We have agreed it is 91mm on MRI and 92mm on CT.
6. What threshold is used to define a narrow male pelvic outlet?
DS and DB: We have agreed the threshold is 82.7mm as per article available in latest trial bundle.”
Early learning curve for TaTME
Claimant’s evidence
“38. It is clear that the RBUH Unit and Mr Courtney were very early in their ‘learning curve’ for taTME.
38.1 The early phase of taTME adoption and ‘learning curve’ has been strongly associated with increased risks of complications and the occurrence of complications not normally associated with TME/rectal cancer surgery.
…
39. Complications from taTME are much higher during the ‘learning curve’ and hence outcomes, both functional and oncological are inherently poorer.
…
44. There is no evidence that Mr Courtney and team were mentored during their early cases either from Mr R Hompes or a similarly experienced surgeon.”
“In general, it is accepted for new procedures and for surgeons learning new skills there is a period of proficiency gain that is generally related to impaired outcomes, specific to the technique and specific to the surgeon. This would tie in with caution around the procedure at that time and in official guidance and the uncertainty at that time should have been expressed to the Claimant. Longer operation times often reflect early stages in proficiency gain.”
“The learning curve for safe and independent practice of TaTME is yet to be established but progress is slow even for the experienced laparoscopic colorectal surgeon. …
The panel agrees that the overall learning curve is long and demanding, with more than 20 cases required. No consensus could be reached on a given number of procedures to reach proficiency.
…
However, surgeons did experience intra-operative equipment and technical difficulties in up to 40% of cases, with incorrect plane dissection, pelvic bleeding, unstable pneumopelvis and, more worryingly, visceral injuries such as urethral division. Indeed, one of the most dreaded specific complication of TaTME is the injury of the urethra during initial anterior dissection.” (my emphasis)
“Conclusions: the learning curve of TaTME affected major (surgical) postoperative complications of the first 40 patients. … When implementing this new technique, a thorough teaching and supervisory program is recommended to shorten the learning curve and improve the clinical outcomes of the first patients.”
“Although many structured training programs have been developed world-wide to assist surgeons in implementing this new technique, the learning curve (LC) of taTME has yet to be conclusively defined. This is particularly important given the concerns regarding the complication profile and oncological safety of taTME.
In light of the recent concerns regarding the safety of taTME culminating in the Norwegian moratorium on this procedure, the analysed studies suggest that there is a significant LC during the uptake of taTME with the estimated number of procedures required to achieve proficiency in taTME ranging from 30 to 140 cases.
…
Extreme caution should be exercised when taking up this procedure, perhaps for a subset of carefully selected patients in the hands of experienced and well-trained teams dedicated to ongoing audit.”
Defendant’s evidence
“I agree that there are problems during the learning curve. But those problems are to do with interoperative bleeding, interoperative urethral injuries, interoperative carbon dioxide emboli and post-operative problems, such as anastomotic leak and also inadequate, oncologically inadequate TME specimens.”
“Indirectly implied [in my report] when I refer to the articles regarding functional outcomes in TaTME and laparoscopic TME.”
“1.17 There is no evidence of differences in the surgical risks between open or laparoscopic AR + TME and TaTME, or in the duration or severity of postoperative symptoms.”
“And I stand by what I said which was that the learning curve issues as I outlined them with the complications and the inadequate oncological specimen were not directly relevant to the causation issues, which are to do with functional outcomes. And because there were no differences in functional outcomes in these articles, I did not think that it was relevant to discuss learning curve with respect to improvement in functional outcomes as you reach the plateau of your learning curve.”
Findings as to early learning curve for TaTME
i) Mr Meleagros accepted in cross-examination that the Claimant should have been informed by Mr Courtney that he was only carrying out his second TaTME as part of the consenting process.
ii) I accept Mr Jenkin’s evidence that [231],
“38.1 The early phase of taTME adoption and ‘learning curve’ has been strongly associated with increased risks of complications and the occurrence of complications not normally associated with TME/rectal cancer surgery.”
iii) Mr Jenkins’ evidence is supported by the medical literature, such as the St Gallen consensus paper [232] and the paper by Koedam [233]. The St Gallen paper states that in the early learning curve in up to 40% of cases there are technical difficulties, including incorrect plane dissection, which is in issue in the present case. Further, I accept Mr Jenkins’ evidence that the St Gallen paper refers to urethral division, which is caused by incorrect plane dissection. It is the Claimant’s case that, by reason of Mr Courtney and Mr Dalton going outside the mesorectal plane on more than one occasion, his pelvic nerves were damaged and this has caused total impotence, total loss of ejaculation and orgasm, and urinary urge, and urinary incontinence.
“138. In the literature indicating equivalence between taTME and lapTME, the outcomes are contingent upon a taTME service that has been established and has already ascended the ‘learning curve’; at such a point, the outcomes from taTME may become comparable to established open and laparoscopic TME outcomes but no earlier, in my opinion.”
Total impotence, loss of ejaculation and anorgasmia
“The Claimant underwent what was described as a TaTME (trans-anal total mesorectal excision) on 8 December 2015. JR notes that the Particulars of Claim state “The Hospital’s colorectal surgeons had performed their first TaTME procedure in November 2015, and were therefore early on a ‘learning curve’…”. JR notes that the anaesthetic chart records an anaesthetic lasting from 0900 to 1800, so the procedure lasted in the order of 8-9 hours.
In JR’s opinion most individuals operated on by surgeons experienced in TaTME do not experience bladder dysfunction or erectile dysfunction. Had the Claimant undergone an open or laparoscopic TME by experienced surgeons or a TaTME after their learning curve for this procedure had passed, he would not have experienced bladder dysfunction or erectile dysfunction. In JR’s opinion the cause of his bladder dysfunction and erectile dysfunction was due to the procedure being done very early during a surgical learning curve.”
“The Defendant’s position, per Mr Meleagros and Professor Sethia, is that intra-operative nerve injury resulting in damage to the nerves controlling urinary and sexual function is a non-negligent complication which is a recognised risk of all forms of pelvic surgery.”
“As above KS says that bladder and erectile dysfunction are recognised complications of both procedure so he was at risk of both sexual and urinary complications whichever procedure was undertaken. The evidence is that there is no significant difference between the rate of these complications after laparoscopic TME or TaTME.”
Issues regarding total impotence, loss of ejaculation and anorgasmia
i) What was the Claimant’s sexual function prior to his TaTME operation on 8 December 2015?
ii) On the balance of probabilities, were the Claimant’s pelvic autonomic nerves damaged during the TaTME on 8 December 2015?
iii) Should the Claimant’s pelvic autonomic nerves have been identified and preserved by Mr Courtney and Mr Dalton?
iv) On the balance of probabilities, was the Claimant’s total impotence and loss of ejaculatory function and anorgasmia caused by Mr Courtney and Mr Dalton, who were early in the learning curve, entering the wrong plane?
v) On the balance of probabilities, would the Claimant have suffered total impotence, loss of ejaculatory function and loss of ability to orgasm if he had undergone an open or laparoscopic TME?
Claimant’s sexual functioning prior to TaTME
i) The Claimant says in his witness statement, dated 18 November 2021 [237],
“My complete loss of erectile function and ability to orgasm happened after the TaTME surgery”
ii) Helen Snow says in her witness statement, dated 18 November 2021, at paragraph 19 [238],
“Malcolm did not have impotence before the December surgery; he had normal erections.”
iii) The Defendant’s consultant urologist, Professor Krishna Sethia DM FRCS, says in his report, dated 21 December 2021 [239],
“Before October 2015 the Claimant had had no problems with erectile function.”
iv) Mr Jenkins says in his condition and prognosis report, dated 29 March 2022 [240],
“7.3. Erectile and ejaculatory function - current and future function
Mr Snow’s erectile function has been lost almost immediately after rectal surgery. He assured me that he had normal erectile function after radiotherapy and prior to surgery but unfortunately has been without any function whatsoever immediately after surgery. He has been unable to ejaculate either.”
On the balance of probabilities, were the Claimant’s pelvic autonomic nerves damaged during the TaTME on 8 December 2015?
“We agree that both his sexual and bladder dysfunction are result of his surgery.”
“Dr Ellis: … it’s startling, isn’t it, bearing in mind what we know about potential risks including pelvic nerve injury, there is no record, is there, that any of the relevant nerves were ever identified or preserved?
Mr Courtney: There’s no record of it, no.
Dr Ellis: No. And what probably happened, didn’t it, is that during the part described as a difficult dissection, this is where those pelvic nerves, which presumably hadn’t been identified and preserved, were injured?
Mr Courtney: I presume so, yes.”
“It’s not disputed the nerves must have been injured during the course of surgery.”
Should the Claimant’s pelvic autonomic nerves have been identified and preserved?
Claimant’s evidence
“If you look carefully at the pelvic side wall you can usually see the nervi erigentes behind the presacral in the same fascial plane curving tangentially round the mesorectum to form a neurovascular confluence posterolateral to the vesicles.
…
Navigating inside it [the mesorectal fascia] guarantees unimpaired potency and bladder function - often valuable prizes indeed. Pilotage of this difficult passage requires, above all, practice and expertise.”
“By dissecting embryological planes between the mesorectum and hypogastric nerve fascia on the posterolateral side, the 3rd and 4th pelvic and pelvic plexus are preserved. After continuing dissection along the mesorectum from the lateral to the anterolateral side, the dissection layer connects below Denonvillier’s fascia at the anterolateral side, and the neurovascular bundle is completely preserved.”
“I think this was a very honest and indeed elegant study done by a Japanese group and the Japanese have excelled in some of the technical aspect of colorectal surgery. And what they have identified is there is a constellation of nerve injuries that can arise as a result of transanal retrograde rectal mobilisation that are associated with functional outcomes. In this circumstance, urinary dysfunction is measured but would also apply to sexual function. But it indicates, to me, that the more extensive the nerve injury, the greater number of components of nerve injuries that occur and the greater the magnitude of the urinary dysfunction that follows and based on longitudinal assessment of these patients, the greater the durability of the insult.”
“Certain patterns of autonomic nerve resection are related to bladder -- urinary dysfunction, but also are strongly related to surgery that goes outwith the standard mesorectal plane.
They describe this as beyond TME surgery. But in essence, this is surgery that is deliberately going outwith the standard planes to ensure disease clearance.
…
They have categorised four patterns and the pattern with the poorest outcome would be most consistent with Mr Snow's functional outcome and that would be best described as a full house of autonomic nerve resection or injury.
…
What the paper has said to me is that injury in one site will produce dysfunction that is mostly transient. For permanent dysfunction then it requires multiple sites of autonomic nerve injury/resection to produce this.” (my emphasis)
“Mr Feeny: But if you’ve got to the section, to the point you want, you don’t go looking for nerves, do you?
Mr Jenkins: No, it’s part of the anatomical steps in a mesorectal dissection.”
“I think there is an imperative. Part of the anatomical dissection of the mesorectum requires identification of the superior hypogastrics to permit entry into a safe mesorectal plane. … It’s a fundamental step in the procedure.”
“There are a multitude of mechanisms for nerve injury inter-operatively. There can be stretching that might produce a neuropraxia, a bruising of the nerve which results. There can be thermal injury which may produce a permanent injury to the nerve but in my opinion often produces a more transient disturbance given that the nerve fibres that are still intact, you can regenerate. … In my opinion it will produce a transient. It is the division or resection that produces permanent loss of function.”
Defendant’s evidence
“Dr Ellis: And that’s the whole point about nerve identifying and preserving surgery going back to the 1980s when Professor Heald seems to have kicked it off long before the Japanese. The very point is if you make an effort, as Mr Jenkins said, if you go and look for them you will find them and we have photographs demonstrating that.
Mr Meleagros: Yes.
…
Mr Meleagros: I accept that Professor Heald, the pioneer of TME went and learned the anatomy and saw the anatomy and said this is possible. Of course it’s possible. It’s perfectly possible, the nerves are there so if you look for them carefully you will find them.
Dr Ellis: Exactly.
Mr Meleagros: But the point is in surgical practice this does not happen.
…
Dr Ellis: I mean, that’s not correct, is it? Because these studies going back to the 1980s refer very clearly with careful dissection to the nerves being visible, don’t they?
Mr Meleagros: Yes, so these fascial layers are very flimsy, so you can very easily enter them and see the nerves.
…
In Western patients we just don't see them very often or very rarely as I described to your Lordship. And we don't deliberately look for them.”
“The elegant dissection photographs that we see in that article by the Japanese, which show these nerves, these sacral routes, is not something that we do in this country. The Japanese undertake that dissection because they undertake lateral pelvic lymph node dissection. … We don’t remove them in this country but in Japan they do dissection beyond this fascia I was just describing. That’s why they identify these nerves.”
“So as I was saying, the Japanese, they often go outside the, let’s call it the TME plane, or what Heald called the holy plane.”
Finding as to whether Claimant’s pelvic autonomic nerves should have been identified and preserved
i) In “The ‘Holy Plane’ of rectal surgery”, dated September 1988 [259], Mr Heald talked in terms of preserving the pelvic autonomic nerves, saying [260],
“Navigating inside it [the mesorectal plane] guarantees unimpaired potency and bladder function - often valuable prizes indeed. Pilotage of this difficult passage requires, above all, practice and expertise.”
ii) In the paper “Bowel dysfunction after treatment for rectal surgery” (Emmertsen 2008) it is said [261],
“Anterior resection with Total Mesorectal Excision (TME) is the golden standard for rectal cancer surgery. The resection is done Ad Modum Heald where the tumour and the mesorectum are excised by sharp dissection with preservation of the autonomic nerves of the pelvis”
iii) In “Risk factors for sexual dysfunction after rectal cancer treatment” (Lange 2009) it is said [262],
“The practice of TME in rectal cancer treatment improved autonomous nerve preservation substantially. Subsequently, the rates of sexual dysfunction (SD) were reduced.” (my emphasis)
iv) In a paper by Nesbakken et al of the Department of Surgery, Oslo, Norway (1999) it is said [263],
“Total mesorectal excision (TME), according to the technique described by Heald, was introduced as the standard method for treatment of rectal cancer in the authors’ departments in 1992. In this operation the autonomic nerves are carefully preserved and one would expect few genitourinary complications.”
v) In a French paper, “A prospective study of sexual and urinary function before and after total mesorectal excision with autonomic nerve preservation for rectal cancer” (Pocard et al 2001), it is said [264],
“Urinary and sexual dysfunction is a well-recognised complication of colorectal operations. However, major advances have been made in understanding erectile and ejaculatory physiology. Walsh and Schlegel have used these advances to suggest improvements to the techniques avoiding postoperative impotence and ejaculatory dysfunction. In the TME technique, the rectum is mobilised circumferentially under direct vision with sharp dissection along the parietal pelvic fascia. This procedure, combined with an awareness of the pelvic autonomic nerve pathways, was highlighted by Enker as the autonomic nerve preservation technique (ANP), thereby minimising sexual and urinary dysfunction. One recent study demonstrated that mesorectal excision for rectal cancer has resulted in a low frequency of serious bladder and sexual dysfunction.
…
The operations were performed by senior surgeons. All the patients underwent TME according to the principles described by Heald et al. Care was taken to preserve the superior hypogastric plexus descending on the anterior surface of aorta and dividing in the 2 hypogastric nerves running down on each side of the pelvis to the inferior hypogastric plexus and the pelvic splanchnic nerves (nervi erigentes) from S-2, S-3, and S-4. … No patient had lateral pelvic side wall involvement, which could have required nerve resection.” (my emphasis)
“I have not seen any literature from this country, at least, describing a technique of laparoscopic TME with deliberate identification of nerves reflected in reduced functional disturbance.”
“Navigating inside it [the mesorectal plane] guarantees unimpaired potency and bladder function - often valuable prizes indeed.”
On the balance of probabilities, was the Claimant’s total impotence and loss of ejaculatory function and anorgasmia caused by Mr Courtney and Mr Dalton, who were early in the learning curve, entering the wrong plane?
Claimant’s evidence
“69. TaTME has been associated with high rates of ‘wrong plane surgery’, particularly during the ‘learning curve’.
69.1. Such inadvertent dissections expose anatomy such as nerves and other pelvic structures to inappropriate injuries and hence a patient to their unfortunate legacies.
…
70. Insufficient detail is provided [in the operation record] to understand the planes that were actually encountered during Mr Snow’s operation and whether nerves were identified
70.1. either near the IMA [blood vessel origin]; at the pelvic brim with the superior hypogastric or lower in the anterior pelvis at the fascia of Denonvilliers’; whether the dissection ran anterior or posterior to his layer;
70.2. as all these areas may have implications for subsequent urogenital function, in relation to bladder, erectile and ejaculatory function.
71. I have assumed that the difficulties encountered during surgery mostly reflect ‘wrong plane surgery’ as, on the balance of probabilities, maintenance of correct anatomical planes would have allowed a more rapid [the Claimant’s operation lasted 8½ - 9 hours] and more event-free intra-operative course.”
“JTJ Opinion … Literature indicates that even after training in taTME that iatrogenic injuries rates are high in incidence [Atallah et al, 2017] and wrong plane surgery in nearly 10% when witnessed in action during training.”
Mr Feeny: There’s another point here, which is that if a surgeon is in the wrong plane there will be warning signs during the course of the surgery.
Mr Jenkins: No. Sadly that has been the problem. That is why there have been urethral transections. … Sadly it’s not the case that there are early warnings. That is why surgeons have found themselves transecting urethras because they couldn’t see the crash about to happen.
…
I have watched over the years many trainees get into the wrong plane and stay in the wrong plane. There is a concept of conscious competence, conscious incompetence and unconscious incompetence and you don’t know what you don’t know. If you're dealing with an approach that you’re unfamiliar with, you will not have necessarily gained the right experience to have the early warning alert that tell you to re-engage with a different plane.”
“Dr Ellis: … That’s what Mr Jenkins described yesterday, didn’t he? He talked about inexperienced surgeons either consciously or unconsciously straying outside the correct plane. It’s recognised that this happens during the learning curve, isn’t it? Even if you’re experienced from top down.
Mr Meleagros: It is recognised, yes.”
“Operative difficulty as alluded to in the operation note would infer technical issues that would most likely relate to entry into an incorrect plane as ‘tethering at 5 o’clock’ implies to me that structures were encountered that would not have been were a correct plane adhered to ie incorrect plane.”
“Mr Feeny: It’s not disputed the nerves must have been injured during the course of surgery. The question is whether that denotes wrong surgical technique. Yes? That it can only happen through wrong surgical technique?
Mr Jenkins: If the correct anatomical plane, which is the mesorectal fascia, is followed … then it would be reasonable to say that it is unlikely to produce significant nerve injury. Indeed there were reports where autonomic nerve preservation has been performed, the incidences of urinary and sexual dysfunction are relatively low.
…
Mr Feeny: So the question then is a factual one: did they get into the wrong plane?
Mr Jenkins: Yes, based on the outcome and based on the scant intraoperative operation note detail.
…
I described it as a full house earlier, but in order to achieve the multitude of different injuries we saw on Mr Snow, by definition, in my opinion … one would have to go into the wrong planes on a multitude of positions within the pelvis. … In a multitude of positions during mesorectal dissection. And I would propose, based on my own experience and my understanding of proficiency gain literature, that that is far more likely to occur on your second patient.”
“The formal histopathology specimen report does not clarify whether the specimen had followed the suitable mesorectal fascial plane dissection as would be reflected in many modern rectal cancer histopathology minimum data set reporting templates.”
“Dr Ellis: My point was simply this: you couldn’t achieve all of Mr Snow’s erectile, ejaculatory, orgasm, bladder dysfunctions by a simple injury at 5 o’clock, could you? I think you accept that. Even the 2 to 3 centimetre plexus where some fibres merge is not at 5 o’clock?
Professor Sethia: I accept that.
Dr Ellis: And in fact you couldn’t achieve the full spectrum of Mr Snow’s injuries, could you, with unilateral nerve injury in this case; it is unlikely, isn’t it?
Professor Sethia: I think it is unlikely.
Dr Ellis: And it follows, therefore, that it is more likely than not that Mr Snow has suffered multiple nerve injuries at different sites?
Professor Sethia: I think he’s -- my opinion is he’s probably suffered a bilateral nerve injury.”
“116. Bladder and erectile function outcomes are negatively impacted upon by neoadjuvant radiotherapy (I understand that the Claimant was warned of the risk of radiotherapy but he experienced no problems with erection after his treatment).”
Defendant’s evidence
“2.15 The histology report on the resection specimen does not state that the mesorectal plane had been breached or was not intact/complete or included extra tissue, in any part of the resected rectum. Specifically, the report states ‘metastatic lymph node is seen close to the posterior mesenteric resection wall … closest radial margin is 16mm which is left anterior’. The histology report also states that the cancer was at ‘18mm from the distal resection margin’.”
i) Thermal injury with the use of diathermy, which is the energy modality used for the dissection [284].
ii) The insertion of rigid instruments down the anal canal, touching the side walls of the pelvis or the front of the sacrum. He said, “So I think direct traumatic or mechanical injury can shear some of these nerves” [285].
…
There is no report of excessive bleeding in the records of the operation on 08/12/2015. In my opinion there is no evidence of wrong plane surgery, either breaching of the mesorectum or the pelvic side-walls, notwithstanding the limitations in assessing this as noted above.”
“On this basis, given our best information currently, I have consented Malcolm to radiotherapy treatment, having discussed the risks of acute and late toxicities with a small increase in the risk of impairment in wound healing and impaired rectal function and a very small additional risk to the chance of impotence.”
Findings as to whether on the balance of probabilities the Claimant’s total impotence and loss of ejaculatory function and anorgasmia were caused by wrong-plane surgery
“The learning curve for safe and independent practice of TaTME is yet to be established but progress is slow even for the experienced laparoscopic colorectal surgeon. …
The panel agrees that the overall learning curve is long and demanding, with more than 20 cases required. No consensus could be reached on a given number of procedures to reach proficiency.
…
However, surgeons did experience intra-operative equipment and technical difficulties in up to 40% of cases, with incorrect plane dissection, pelvic bleeding, unstable pneumopelvis and, more worryingly, visceral injuries such as urethral division. Indeed, one of the most dreaded specific complication of TaTME is the injury of the urethra during initial anterior dissection.” (my emphasis)
“You would have to hit the net at multiple points in order for the net no longer to work.”
“My opinion is he’s probably suffered a bilateral nerve injury.”
“Total mesorectal excision with pelvic autonomic nerve preservation showed relative safety in preserving sexual and voiding function.”
“Radiotherapy on its own would be very unlikely to cause impotence, at the dose used.”
i) I have found that Mr Courtney is an unreliable witness;
ii) In any event, I accept Mr Jenkins’ evidence that surgeons can enter and continue in the wrong plane without being aware of it, particularly when in the early stage of the learning curve.
iii) Mr Courtney’s record keeping is substandard. Mr Courtney accepted that the note of the operation was substandard. Therefore, no weight can be placed on the fact that the operation note does not refer to the surgeons being in the wrong plane.
iv) The operation lasted 8½ - 9 hours, which is significantly longer than usual, and would suggest that the surgeons encountered difficulties;
v) I accept Mr Jenkins’ evidence the specimen obtained during the operation did not have a comment on the mesorectal fascial plane or a grading, as required by the Pathology College, and as a consequence no inference can be drawn from it as to whether or not Mr Courtney and Mr Dalton were in the correct plane.
On the balance of probabilities, would the Claimant have suffered total impotence, loss of ejaculatory function and anorgasmia if he had undergone a conventional TME?
Claimant’s evidence
i) A paper by Havenga et al from Memorial Sloan Kettering in New York in 1996. The study involved 175 patients and assessed sexual and urinary function after total mesorectal excision with autonomic nerve preservation for primary carcinoma of the rectum and found that [298],
“The ability to engage in intercourse was maintained by 86 percent of the patients younger than 60 years of age, and by 67 percent of patients 60 years and older. Eighty-seven percent of male patients maintained their ability to achieve orgasm.”
ii) A paper by Masui et al from Yokohama in 1996 [299]. The study involved 134 patients undergoing autonomic nerve preservation operations for rectal cancer and found that in 87.7% and 66.9% of patients, erectile and ejaculatory potencies respectively were maintained.
iii) A paper by Quah et al from Singapore in 2002 [300]. The study showed that of 22 men who underwent open TME, only one was left impotent. The remaining 21 had preserved ejaculation. Of 14 men who underwent laparoscopic TME, impotence was reported in 5 cases.
iv) A paper, “Assessment of sexual and voiding function after total mesorectal excision with pelvic autonomic nerve preservation in males with rectal cancer”, by Kim et al from South Korea in 2002 [301]. The study found that following total mesorectal excision with pelvic autonomic nerve preservation in men with rectal cancer, erection was possible in 80.9% of patients and penetration ability was possible in 75%. Complete inability to achieve an erection and to have intercourse was only observed in 5.5% of patients. The abstract states [302],
“Conclusion: Total mesorectal excision with pelvic autonomic nerve preservation showed relative safety in preserving sexual and voiding function.”
v) A paper by Pocard in 2002 [303]. This was a study of 14 men who underwent total mesorectal excision with pelvic autonomic nerve preservation. The study found that 69% of those who were sexually potent preoperatively had unchanged sexual activity and potency post-surgery. After three months, four patients reported a reduced rigidity of erection, returning to normal by one year.
Defendant’s evidence
“Wrong plane surgery has long been recognized with open and laparoscopic TME and not only during the learning phase (curve). It is not a new concept that has arisen since the introduction of TaTME. The Claimant does not refer to the recognized occurrence of wrong plane surgery with the established surgical techniques but addresses the issue solely in relation to TaTME.”
“Dr Ellis: But it’s self-evident, isn’t it, if you’re sexually active you’re having sex. We don’t know how often or with what degree of satisfaction but you can’t be sexually active without an erection, can you?
Professor Sethia: Yes, you can. You can be sexually active because you can, for example, stimulate your partner and that would count as sexual activity, without you necessarily personally achieving sexual satisfaction.”
Finding as to whether Claimant would have suffered total impotence, loss of ejaculatory function and anorgasmia with a laparoscopic TME
“129. It is my view that while there is a significant risk of sexual dysfunction post anterior resection with TME and ANP [autonomic nerve preservation], most men (something in the order of 60-85% or thereabouts in most series) remain potent and most men have preserved bladder function after anterior resection with TME and ANP. Therefore, if the Court determines that the extent of pelvic dissection that would have been required (based on the expert colorectal opinions in this case) would have been equivalent to a TME with autonomic nerve preservation he would probably have preserved erectile and ejaculatory function.”
“The practice of TME in rectal cancer treatment improved autonomous nerve preservation substantially. Subsequently, the rates of sexual dysfunction (SD) were reduced.”
“Of the male patients sexually active before treatment, 31.5 percent indicated not to be sexually active at 3 months after surgery. This percentage remained more or less stable over time (28.5 percent at two years). However, only 59 male patients (15.2 percent) never indicated to be sexually active after treatment.”
Claimant’s urinary urgency and incontinence
“71. I suffer urinary symptoms as well. Since my surgery in December 2015, I am less aware of bladder fullness, I have to strain to initiate and maintain a flow when I pass urine, the flow is slower and weaker and there is always a second phase of flow, accounting for around 30% of the voided volume. Even though after passing urine there is still residual urine in my bladder.
I empty my bladder 8-9 times daily and have to get up at least twice during the night to pass urine. I suffer urinary urgency and incontinence on a daily basis so I have to wear an incontinence pad. I buy packets of Tena and wipes mostly from Boots or our local supermarket. On average I use 3-4 pads daily but on a bad day it has been up to 12 pads per day.”
“15. The Claimant told me that since March 2016 he has been voiding without relying on CISC. He voids an average of 8 times in a 24 hour period. He feels that he has to strain to void and that his bladder empties incompletely. He has documented the average time of his visits to the toilet at approximately 20 minutes. He suffers from occasional sudden episodes of urgency. He experiences occasional small leaks and wears 2-3 small pads during the day and one at night. There has been no change in these symptoms over the past 5 years. He said that he tried various medications none of which have helped.
…
18. He feels that his urinary symptoms do restrict his social activities as it takes him such a long time to void. He used to work as a project engineer but had to leave this job as he was unable to travel. He now works for the Ministry of Defence.”
“43. He voids urine spontaneously. He strains to a degree to initiate a void and maintain a flow.
44. Voiding time is longer than prior to the index surgery. He has calculated that approximately 1 hour a day is spent voiding urine because (a) the flow is slower (b) he waits after an initial void and there is always an additional volume of urine to be voided.
45. He has some reduction of awareness of bladder fullness.
46. Daytime voiding frequency is 8-9 times daily.
47. Night-time voiding frequency is 2 times.
48. He experiences urinary urgency several times every day and urge incontinence on a daily basis. He wears pads for this leakage. He wears 3 pads per day. He has tried trospium and solifenacin with no effect and the same applies to Mirabegron.
51. He experiences hesitancy in initiating a flow of urine. The strength of the flow is lower than before the index surgery.
…
53. He experiences a feeling of incomplete bladder emptying.”
“19. … As his symptoms have not changed for 5 years they are extremely unlikely to improve spontaneously now.”
“I feel that it is highly unlikely his urinary bladder function will improve. He links this to a significant deterioration in his quality of life. He reports that each time he passes urine he is concerned that he may soil himself and therefore he must sit upon the toilet to not only pass urine but also to avoid any episodes of faecal incontinence. He reports that around 50% of the time that he passes urine that he experiences the need to evacuate still. He experiences the faecal evacuation as involuntary much of the time. As Mr Snow ages, it is my opinion, that the function will progressively deteriorate over time meaning that he may not only require incontinence pants for faecal incontinence but this may be required for urinary difficulties.”
Are Claimant’s urinary incontinence and urgency caused by pelvic nerve damage?
“We agree that both his sexual and his bladder dysfunction are result of his surgery.”
“Both bladder and erectile dysfunction are well-recognised complications of any type of surgery to excise the rectum and can occur in the most experienced hands. Therefore in his opinion the fact that the Claimant has these complications does not necessarily indicate poor technique.”
“In JR’s opinion most individuals operated on by surgeons experienced in TaTME do not experience bladder dysfunction or erectile dysfunction. Had the Claimant undergone an open or laparoscopic TME by experienced surgeons or a TaTME after their learning curve for this procedure had passed, he would not have experienced bladder dysfunction or erectile dysfunction. In JR’s opinion the cause of his bladder dysfunction and erectile dysfunction was due to the procedure being done very early during a surgical learning curve.”
“In my opinion, the onset of urinary and urogenital dysfunction immediately after the operation reflects the issues stated above. Dissection in the anterior plane at taTME may injure erectile nerves but also nerves laterally in the pelvis may be damaged to produce bladder dysfunction. This occurred rapidly after surgery in Mr Snow.”
Findings as to cause of the Claimant’s urinary urgency and incontinence
On the balance of probabilities, would the Claimant have suffered urinary urgency and incontinence if he had undergone TME?
Defendant’s evidence
“Accordingly even if, which is denied, the Claimant had undergone a TME as opposed to a TaTME it is denied that he would have avoided significant bladder and erectile dysfunction. The Defendant reiterates that set out in (c) (vi) and (vii) above, namely that the same would have arisen in any event.”
“Given that the Claimant had a mid to low rectal cancer and was due to undergo a TaTME on the balance of probabilities he was expected to suffer with urinary and sexual dysfunction. He should have been warned accordingly.”
Claimant’s evidence
“130. It is my view that his symptoms of urgency several times every day and urge incontinence on a daily basis which is due to urodynamically proven bladder overactivity (on 10 October 2019) is due to partial denervation of his bladder (further evidenced by his residual urine volume - he retains about one third of his bladder volume - and by his urinary hesitancy, his need to strain to a degree to initiate a void and maintain a flow and his reduced strength of urinary flow). This would probably not have occurred had he undergone a conventional low anterior resection, preserving the anal canal and sphincters with total mesorectal excision (TME) and nerve preservation.”
“In JR’s opinion had he undergone an open or laparoscopic TME or a TaTME after the surgical learning curve, he would have avoided bladder and sexual dysfunction.”
Findings as to whether Claimant would have suffered urinary urgency and incontinence if he had undergone TME?
i) The paper by Havenga et al from Memorial Sloan Kettering in New York in 1996. The study involved 175 patients and assessed sexual and urinary function after total mesorectal excision with autonomic nerve preservation for primary carcinoma of the rectum and found that [325],
“The majority of patients had few or no complaints related to urinary function. Serious urinary dysfunction such as neurogenic bladder was not encountered.”
ii) The paper by Quah et al from Singapore in 2002 [326]. The study showed that of 40 patients who underwent open TME, none experienced a significant deterioration in bladder function. Of the 40 patients who underwent laparoscopically assisted mesorectal resection, two required long-term intermittent self-catherisation.
iii) The paper by Pocard in 2002 [327]. This was a study of 14 men in Paris who underwent total mesorectal excision with pelvic autonomic nerve preservation. The study found that there was no difference in pre-operative and post-operative urinary function.
iv) The 2015 NICE interventional procedures guidance says [328],
“Acute urinary retention was reported in 3% (1/37) of patients in the TaTME group and in 11% (4/37) of patients in the laparoscopic TME group in the non-randomised comparative study of 74 patients (p=0.16; no further details provided). Transient urinary disorders were reported in 9% (5/56) of patients in the case series of 56 patients; all patients were treated by temporary urethral catheterisation. After 3 months, all patients reported normal urinary function.”
“1) In respect of anterior resection with TaTME, are the experts able to agree what the current medical scientific knowledge is in relation to:
a) The risk of urological dysfunction, compared with open and laparoscopic TME?
KS says that the reported incidence of bladder dysfunction is between 0 and 30%.”
“25. Chemotherapy may induce a peripheral neuropathy which in turn could affect bladder function. Up to approximately 20% of men may suffer significant urinary symptoms after chemotherapy but these tend to develop over a period of months and are commoner in patients displaying other symptoms/signs of peripheral neuropathy.
26. Urinary incontinence is a very uncommon long term result of pelvic radiotherapy alone.”
“Mr Meleagros: That’s why I said severe and incidentally you said urinary, but I think in this paragraph I just talk about sexual.
Dr Ellis: Well, no, you didn't, because if you look at the top of page 336 that's why I asked you. On a balance of probabilities he was expected to suffer with urinary and sexual dysfunction?
Mr Meleagros: Yes, you are right, sorry, sorry. So I think urinary was stretching it a bit.
Judge Roberts: So that's stretching it a bit?
Mr Meleagros: I think I was referring to sexual when -- because these figures are sexual dysfunction, not urinary.
Dr Ellis: So on a balance of probabilities he was not condemned inevitably to bladder dysfunction, was he? That's what you have just said.
Mr Meleagros: Yes, I agree there. Because the subsequent data does not support this statement. So I went beyond what the papers that I was aware of said, these are primarily on sexual.”
Low Anterior Resection Syndrome (LARS)
Introduction
“The spectrum of such dysfunction is broad, and can include incontinence, constipation and clustering of stool, all of which have a negative impact on health-related quality of life. This wide range of complaints has been collaged into a pragmatic definition, i.e. low anterior resection syndrome (LARS).”
“Low anterior resection syndrome score
The LARS score is a validated and simple scoring system developed for quick evaluation of the presence and severity of LARS. The LARS score is based on five questions, with the corresponding scoring value weighted according to impact on quality of life.
The questions concern the following: incontinence for flatus, incontinence for liquid stool, frequency of bowel movements, clustering of stools, and urgency. The calculated score ranges from 0 to 42 points, based on which patients are classified into three groups: no LARS (0-20 points), minor LARS (21-29 points), and major LARS (30-42 points).”
Known LARS risk factors
“Known risk factors for the development of LARS are a low level of anastomosis, poor preoperative function and neoadjuvant chemoradiotherapy. With the TaTME technique, surgeons might choose a lower anastomosis for technical rather than oncological reasons, and urethral injuries are more likely. […] The height of anastomosis was not reported systematically, but was significantly lower after TaTME in the study of Mosquera and colleagues.”
Major LARS in any event
“LM will say as follows: … Based on tumour height of 10cm or less the POLARS predicts the Claimant would experience major LARS. The score increases slightly from 30 (tumour height 10cm) to 31 (tumour height 9 or 8cm) to 32 (tumour height 7 or 6cm) to 33 (tumour height 5cm). LARS is 34 if the tumour height was 4cm or 3cm. Therefore, based on this score the Claimant would have been advised that he was at risk of major LARS in any event.
JTJ Opinion: Agreed that the major LARS was likely with the Claimant and this should have been explained to the patient but explicit predictive calculations such as POLARS would not have been available in 2015. POLARS was published in 2017.”
“The impact on ‘major’ LARS is further exacerbated by the use of neoadjuvant radiotherapy.”
Overview
“137. In my opinion, Mr Snow’s earlier post-operative function would have been better with ‘standard TME’ be that open or laparoscopic, and his urgency and clustering would probably have been less, even though his overall LARS score may have ultimately been ‘the same’.”
“6.12 As stated previously LARS is a well reported sequelae of low anterior resection. The incidence of LARS does not differ following TaTME compared to open or laparoscopic TME, as reported in the literature. Therefore, according to the articles in the literature LARS is a sequelae of low anterior resection with low colorectal or coloanal anastomosis, independent of the surgical technique employed.”
Mid-rectum tumour
Radiologists’ agreed evidence
“2. What is the height of the anastomosis?
DS and DB: We agree the height/position is at the anorectal junction. We agree the height or position is at the junction between anal canal and rectum, which we are saying is 41mm or 42mm depending if it’s measured on ultrasound or MRI respectively.
3. How does this differ from the average height after a standard TME?
DS and DB: We agree, on average the we (sic) rectal cuff is frequently 10-20mm and we agree that there is variability between centres and patients. We agree that usually there is a discernible cuff of rectum after laparoscopic or open TME and both have rarely seen cases with no discernible rectal cuff.
4. By comparing the pre and post operation MRIs, how much rectal cuff is left behind?
DS and DB: We have agreed there is no discernible rectal cuff. We agree that scarring at the site of anastomosis could obscure any rectal remnant tissue.”
Mr Jenkins’ evidence
166.5. On the balance of probabilities, functional outcomes overall would have been better with conventional TME [laparoscopic and open]
166.5.1 For example: faecal incontinence would have been considerably less frequent, no more than 2 to 3 times per week, as a double stapled anastomosis would have been performed, with a higher staple line.’
i) In “A new solution to solve old problems: Trans-anal TME” (Heald 2013) it is said [342],
“In my opinion, as a frequent ‘voyeur’ of demonstration laparoscopic surgery, it is common for these difficulties to place the anastomosis lower down and nearer to the pubo-rectal sling than some cancers require from the oncological point of view. There is no doubt that the function enjoyed by a patient with an anastomosis at 6 cm from the anal verge is superior to that with one at 3 cm i.e. true colo-anal.”
ii) In the paper “Bowel dysfunction after treatment for rectal surgery” (Emmertsen 2008) it is said [343],
“Risk factors for developing LARS are low colorectal or ultra-low coloanal anastomosis, end-to-end anastomosis, anastomotic leakage, acute or chronic inflammation and adjuvant radiotherapy, with the level of anastomosis being the most important factor.”
iii) In the paper “Functional results and quality of life after transanal total mesorectal excision” (De Nardi 2018) it is said [344],
“The level of anastomosis also plays a significant role while lower anastomosis, particularly colo-anal anastomosis and intersphincteric resections, can lead to a higher risk.”
iv) In the paper “Quality of life and anterior resection syndrome after surgery for mid to low rectal cancer: a cross-sectional study” (Trenti et al 2018) it is said [345],
“A major LARS was observed in 83.3% of the patients who underwent CAA [hand-sewn coloanal ansastomosis] and in 56.6% of the patients who underwent CRA [low mechanical colorectal anastomosis].”
v) It is said in the paper “LARS is associated with lower anastomoses but not with the transanal approach in patients undergoing rectal cancer resection” (Filips et al 2021) [346],
“Furthermore, as demonstrated in the current study, lower anastomoses are associated with a higher complication rate, including LARS. Consequently, very low colorectal anastomoses should be avoided whenever possible and oncologically safe, regardless of the technique used for rectal recisions.”
“‘…the Kim [348] paper that you took me to earlier shows that with an ultra-low anastomosis, which was more akin to what Mr Snow has in situ at present, there is a significant difference in the LARS scores, measured as a odds ratio, compared to standard low anterior resection.
….
You will see the ultra-low anterior resection, which we discussed yesterday my views are very similar to what I have seen in Mr Snow in my opinion, is 5.2, 5.3, over five times more likely to produce major LARS. Whereas radiotherapy, which we have accepted is a significant risk factor, is 2.6 times more likely to produce major LARS. So my interpretation of that is that the surgical component, when it is so low, when the join is done so low, produces a far more likely situation to get major LARS and there’s a greater and indeed independent risk for major LARS, more so than radiotherapy.
…
Ultra-lows are recognised in the surgical community to have a poorer outcome compared to standard TME which would be defined as a low anterior resection…”
“Mr Feeny: Your position is that if there had been a bigger rectal remnant it would have been better [the LARS]?
Mr Jenkins: That is part of it, but the other component which is not necessarily addressed under the banner of LARS is his continence and there is a separate issue with his sphincter, which is not necessarily related to LARS, which confounds the LARS, potentially, and in my opinion makes his LARS worse … .”
Mr Meleagros’ evidence
“6.23 Therefore, the presence of anatomical abnormalities in the internal anal sphincter have not been shown to correlate with functional abnormalities and in particular with more severe LARS symptoms or incontinence.”
“Mr Meleagros: Length of rectal remnant.
I know there is a dispute about how much rectum would have been left but I think we will have to agree now that whatever procedure was undertaken it would have ended up being less than 2 centimetres, especially given St. Gallen saying you have to be 5 centimetres below the mid rectal cancer which brings the rectal remnant to just the anorectal junction. So with surgery alone with a rectal remnant of less than 2 centimetres, major LARS, 67 per cent.
Dr Ellis: With chemo as well?
Dr Meleagros: No, no, the first set of figures, surgery alone. If you add chemo-radiotherapy it goes up from 67 to 78.”
Colorectal experts’ joint statement
i) Mr Jenkins says [352],
“If the anastomosis is around 4cm from the anal verge [and at the upper end of the anal sphincter] as has been suggested then this is more in keeping with such studies and if a lapTME had been conducted then a higher anastomosis would have been more than likely yielded. Even with a higher anastomosis with lapTME the distal resection margin clearance would still have been sufficient and there is no evidence to support suggestions of disadvantage in oncological terms.”
ii) Mr Jenkins says [353],
“Laparoscopic TME will generally produce a higher anastomosis than taTME amounting to 2.6cm average difference.”
iii) Mr Meleagros says [354],
“The height of Mr Snow’s anastomosis is likely to have been 0.5cm higher if lapTME had been performed.”
iv) Mr Meleagros says [355],
“Most articles in the literature do not provide clear definitive and unequivocal statements regarding the relationship between the height of the anastomosis above the anal verge and the severity of LARS. … Therefore, LM will say that the significance of the anastomotic height above the anal verge in relation to the severity of LARS is not confirmed.”
v) Mr Meleagros says [356],
“On review of the relevant literature, LM has not identified a threshold difference in anastomotic height that would result in a significant influence on LARS scores.”
vi) Mr Jenkins says [357],
“Agree. Although the differences reflect that LARS is affected by multiple clinical risks and factors more than just height; as a general rule and from data on handsewn colo-anal anastomosis, the lower an anastomosis, then the poorer the function overall and higher the rate of faecal incontinence.”
vii) Mr Meleagros says that the anastomotic height could not have been 2.6cm higher with a laparoscopic TME, having regard to the measurements on the formalin treated specimen. He says that even if the anastomosis had been 0.3 - 0.5cm higher, this would not have made any difference to the Claimant’s LARS [358].
Discussion
“Results: Overall, major LARS was observed in 38 per cent of patients. In the patients who underwent surgery alone, major LARS was reported by 27 per cent, and a larger remnant rectum was associated with a better functional outcome. In contrast, 80 per cent of patients who underwent combined preoperative chemoradiotherapy and surgery reported having major LARS. No association between the length of remnant rectum and the risk of major LARS was observed in patients treated with combined neoadjuvant therapy and surgery.
Conclusion: Both the length of remnant rectum and preoperative chemoradiotherapy had a major impact on the severity of bowel dysfunction after restorative rectal cancer surgery. No functional benefit from an irradiated rectal remnant was observed.”
“A recent study has suggested that this increased functional impairment after radiotherapy may be due to impaired afferent nerve function in the pelvis, causing neorectal hyposensitivity. The preservation of an irradiated remnant of rectum and its contribution to functional outcome has not previously been investigated.
…
In the present study, the impact of the length of remnant rectum on functional outcome was investigated in patients who had undergone restorative sphincter-preserving surgery for rectal cancer. In patients treated with surgery alone major LARS was reported by 27 per cent, and bowel function deteriorated with less length of remnant rectum as the level of the anastomosis approached the anal verge. In contrast, 80 per cent of patients who received preoperative chemoradiotherapy reported having major LARS, and in these patients a larger remnant rectum did not offer any benefit in terms of functional outcome.”
“Afferent sensory loss
The length of the retained remnant, as measured on MRI scan, correlates with better functional outcome. This beneficial effect is lost in irradiated patients. Both randomized control trials and epidemiological studies show a greatly increased risk of severe LARS following neoadjuvant therapy.”
Findings as to LARS
“The constellation of symptoms representing LARS has a multitude of related factors of which anastomotic height represents one aspect.”
“It is not sufficient to show that delay materially increases the risk or that delay can cause injury. The Plaintiff has to go further and prove that damage was actually caused, that is, that the delay caused injury. In my judgment, it is not sufficient to show a general increment from the delay. He must go further and prove some measurable damage.”
“Digital rectal examination confirmed approximately 1cm of rectum being in situ with anastomosis at this level … proctoscopy once again revealed a low colorectal anastomosis with evidence of friable tissues at the join.”
Mr Feeny: But if we were talking about a difference say between 31 and 30, in practical terms, functional terms, lifestyle, employment, all those issues, it would be impossible to say there was any difference?
Mr Jenkins: I think it would be difficult to prove a difference in terms of quality of life --
Mr Feeny: Yes.
Mr Jenkins: -- between 30 and 31.
Mr Feeny: Yes and restriction on employment, again it would be difficult to --
Mr Jenkins: I cannot comment on that.
Mr Feeny: Okay. But the expression you used in the joint statement, it’s at page 46 of it, is, you say, difficult to quantify. And it's difficult to quantify because it's so slight?
A. Mm.
Injury to internal anal sphincter
“6.9 The Claimant’s description of his bowel function during the interview on 22/06/22 was that he has up to 10 visits to the toilet in 24-hour period including three during the night when he is woken up with the sudden urge to have a bowel movement. The Claimant clarified that some of these visits to the toilet are to pass urine which he cannot do standing and he has to sit on the toilet. Sometimes when he passes urine he also passes stool. To pass stool alone, he visits the toilet approximately four times a day. He stays in the toilet between 45 minutes and an hour and has to sit back down onto the toilet two to three times in quick succession in order to achieve completed evacuation. Sometimes he has to return to the toilet shortly after he has left it. The night time visits to the toilet are also in order to pass urine also.
…
6.13 The Claimant described faecal incontinence. This primarily takes the form of faecal leakage which occurs post-defaecation. It also occurs if he tries to resist the desire to defaecate for protracted periods of time. The Claimant stated that he experiences this approximately once a day and also during the night when he wakes up with urgency to defaecate.”
Issues
“Causing injury to the internal anal sphincter through prolonged use of the TaTME anal port.”
i) Has the Claimant proved on the balance of probabilities that he sustained injury to his internal anal sphincter during the TaTME?
ii) On the balance of probabilities, would the Claimant have sustained injury to his internal anal sphincter if he had undergone a laparoscopic TME?
iii) Has the Claimant proved on the balance of probabilities that he has suffered faecal urgency and incontinence which is caused in whole or in part by injury to his internal anal sphincter.
Was the injury to the internal anal sphincter caused by the TaTME?
“9. In my opinion, and in the absence of any other known causative injury, it seems likely that this trauma occurred during surgery for excision of the rectal cancer.”
“The internal sphincter is fragmented. In my radiology experience, fragmentation most commonly occurs after surgery for haemorrhoids or anal fissure, particularly where a Lord’s stretch of the anal canal was utilised (bimanual stretching of the anal canal, under anaesthetic or sedation). As this procedure is no longer widely undertaken in the UK, the incidence of internal sphincter fragmentation has declined.”
“Yes, of the number of times, and I've done many thousands of these examinations, and of the large majority, almost all of the cases where I have seen fragmentation of the internal sphincter, which is a specific appearance, that would be in the context of a traumatic event, and usually Lord's Stretch. …
So fragmentation, by deduction in the Lord's Stretch is an intentionally traumatic dilatation by a manual dilatation of the anal canal. So, yes, trauma is the most common association.”
5) Are the experts able to agree the appearances of the endo-anal ultrasound scan of 2 February 2022?
Yes. The scan demonstrates fragmentation of the internal sphincter muscle.
6) Are the experts able to agree whether the appearances of the endo-anal ultrasound scan are consistent with any known mechanisms of injury?
Yes. Both experts agree that the likely cause of the fragmented sphincter is trauma which most probably occurred between the MRI scans and at the time of surgery.”
“87. My opinion is that the operation duration was excessively long and in my opinion reflects aspects of the learning curve related to the early phase of taTME in the unit and also operative difficulties that were likely due to ‘wrong plane surgery’.
…
88. Anal endosonography by Dr D Burling in 2022 indicates significant disruption of the internal anal sphincter and this is indicative of significant stretching of the anal canal producing anal injury.
…
165.10 On the balance of probabilities, the internal anal sphincter was injured as a result of [TaTME] surgery and substandard surgical care and that injury would otherwise have been avoided with conventional TME.
…
166.4 There is clear evidence of post-operative and sphincter injury that would be related to taTME equipment and technique and would further confound the poor functional outcomes.”
“There is a potential risk of incontinence with TaTME because the anal sphincter is stretched by the instruments inserted via the anus. The Claimant has not had anal manometry or endoanal ultrasound studies to investigate the function/structure of his anal sphincters. However, the Claimant was examined by Mr Moran in Basingstoke on 07/06/2017, who wrote ‘rectal examination was normal with quite good sphincters clinically’. Therefore, based on clinical evidence the Claimant’s anal sphincters have not been damaged by the TaTME.”
“The injury to the anal sphincter is caused by the transanal insertion of stapling instruments and/or the use of anal retractors.”
“LM will say as follows. The TaTME was carried out using the transanal GelPath port. This measures 4cm in diameter. The handsewn coloanal anastomosis was performed with the aid of the Pratts retractor. The internal anal sphincter disruption noted on endoanal ultrasound, performed by Dr. Burling was likely caused by the transanal instrumentation. …
JTJ Opinion: It is agreed that transanal instrumentation is likely responsible for the internal anal sphincter injury subsequently noted on imaging and likely to have impacted the functional result from surgery. …
The Pratt rectal speculum measures 8.5cm by 2.5cm and reaches to 4.4cm in diameter when opened although may reach this diameter after gentle stretching of the anus.”
Finding as to whether injury to internal anal sphincter caused by TaTME
Likely outcome if Claimant had undergone laparoscopic TME
“88.1 On the balance of probabilities, this would have been avoided if conventional laparoscopic or open TME were performed rather than taTME.”
“Mr Jenkins: The morphology of the injury specific to Mr Snow is more consistent with a Lord's procedure … as in the fragmentation, and were he to have had a standard TME the transanal stapler might have produced a sphincter injury, but that would have been of a different character.”
“The stapler [used in TME] is also significantly smaller in diameter [~3cm] than the anal Gelport or Pratts anal speculum [4+cm]. Moreover, the period of anal distraction would be short and certainly much shorter than that required with taTME.”
“So internal sphincter fragmentation is a relatively uncommon finding in anal ultrasound examinations. …
So of the many thousand I've done there will be only a small proportion will have fragmentation, certainly less than 100 and probably more like tens, tens of cases.
Finding as to whether on balance of probabilities Claimant would have suffered injury to internal anal sphincter if he had undergone laparoscopic TME
i) The stapler used in a TME has a diameter of about 3cm, whereas the anal Gelport or Pratts anal speculum has a diameter of more than 4 cm;
ii) The period of anal distraction would have been much shorter than that required with a TaTM;
iii) I accept the evidence of Dr Burling that internal sphincter fragmentation is relatively uncommon.
Has injury to internal anal sphincter caused faecal urgency and incontinence, in whole or in part?
“91.1 On the balance of probabilities, the internal anal sphincter injury has significantly contributed to Mr Snow’s LARS.
91.2 And will have materially contributed to the severity and hence greater degree of LARS Mr Snow has experienced.
91.3 In my opinion and on the balance of probabilities, the prolonged anal stretching will have materially contributed most to the disruption and fragmentation of the sphincter although the initial insertion technique likely commenced disruption that was propagated and confounded mostly by the duration of the dilatation”
“6.23 Therefore, the presence of anatomical abnormalities in the internal anal sphincter have not been shown to correlate with functional abnormalities and in particular with more severe LARS symptoms or incontinence.”
“Whilst LARS is multifactorial, as per the MANUEL project article, anal sphincter function offers significant contribution to the pathophysiology of LARS although sphincter dysfunction in isolation correlates poorly with LARS;”
Mr Feeny: Can I suggest that’s a highly speculative piece of evidence. You can’t say on the balance of probabilities it wouldn’t have happened in a TME.
Mr Jenkins: I think I can.
…
Mr Feeny: Now, the second general point is that when people have looked at it they found no correlation between this injury and bowel symptoms and in particular they found no correlation between this fragmentation of the internal anal sphincter and the level of LARS, and that’s where I was taking you to –
Mr Jenkins: There is faecal incontinence. That is a strong association.
Judge Roberts: There is a strong?
Mr Jenkins: Association with faecal incontinence although no association with LARS.
…
Mr Feeny: Because incontinence is a symptom of LARS, isn't it?
Mr Jenkins: But it's a symptom on its own, as well.”
Finding as to whether Claimant has suffered faecal urgency and incontinence by reason of injury
“Damage to the sphincteric apparatus also contributes to the development of LARS. In LAR and UAR the sphincter muscles and/or the intrinsic rectal innervation may be compromised leading to disruption of the recto-sphincteric reflexes which causes decreased anal pressures. In addition mechanical lesions to the internal sphincter may occur during the transanal introduction of the circular stapler.”
“Impaired internal anal sphincter function is more clearly associated with passive faecal leakage.”
i) The Consultant Radiologists agree that the Claimant has suffered trauma to his internal anal sphincter in the form of fragmentation during the TaTME.
ii) The examination by Mr Moran on 7 June 2017 [390] was a digital examination [391] and therefore he would not have examined the internal anal sphincter [392].
iii) No inference can be drawn, positive or negative, from the fact that the Claimant has not had anal manometry or endoanal ultrasound studies.
Quantum of damages
Injuries
Erectile dysfunction
i) Total impotence;
ii) Loss of ejaculatory function;
iii) Anorgasmia.
“85. Losing my manhood would be hard to accept at any time, but without any warning, I am really struggling to come to terms with it.
I have since consulted a number of private urologists who specialise in erectile dysfunction. I have been prescribed Viagra and Caverject injections and have tried the pump device which is pretty uncomfortable to use with minimal effects. Caverject helps a little bit with erection but it is a long way from a full erection, which I always had had before the operation, and it is not sufficient for proper intercourse and extremely painful. I do not have orgasms. My injuries caused a devastating impact on the quality of my life and lifestyle, my career, and my relationship with my wife and our sex life.”
“40. Losing his whole masculinity affects Malcolm hugely, it has absolutely devastated him and he feels very angry about not being able to have an erection or an orgasm… He has tried all sorts of treatment, from vacuum pump to tablets and injections but he cannot achieve an erection enough to have sexual intercourse - even with a semi erection he is in pain.
41. We are relatively young and as a couple, sex life is still an important element in our relationship even though we have been married for over 30 years. Before Malcolm’s operation in 2015, we had a fulfilled and enjoyable sex life. I am thankful that we are still feel (sic) passionate about each other but I would say that the past 5+ years have been really a testing time to our marriage and Malcolm’s injuries have ruined our sex life totally - it ended the day of his surgery.”
Urinary urgency and incontinence
“7.2 Bladder Function - current and future function
I feel that it is highly unlikely this his urinary bladder function will improve. He links this to a significant deterioration in his quality of life. …”
“We agree his urological symptoms include spontaneous voiding of urine by straining to a degree to initiate a void and maintain the flow of urine. He told JR that he has calculated that approximately 1 hour a day is spent voiding urine because (a) the flow is slower (b) he waits after an initial void and there is always an additional volume of urine to be voided. He experiences urinary urgency several times every day and urge incontinence on a daily basis. He wears pads for this leakage. He wears 3 pads per day. He has tried trospium and solifenacin with no effect and the same applies to Mirabegron. A urodynamic study on 10.10.19 showed a pre-test post-void residual of 230 ml. Bladder overactivity was identified. On voiding there was no evidence of prostate obstruction. When seen by JR on 16.10.20 a free flow study he voided 225 ml of urine with a maximum flow rate of 11.7 ml/s (low) and a voiding time of 86.1 seconds. Following this he then did a second flow of 12 ml of urine over 117 seconds. His post-void residual urine volume was 131 ml i.e. he retained about one third of his bladder volume.”
Faecal incontinence
Prolonged adjustment disorder of moderate severity and depression
i) Dr Turner, Consultant Psychiatrist, says in his report [398],
“29. There is no evidence prior to the index event, namely Mr Snow undergoing a taTME operation for removal of a rectal carcinoma on 8.12.15, that he has suffered from any formal psychiatric disorder or had required any formal psychiatric treatment.”
ii) Dr Amin, Consultant Psychiatrist, says under ‘Summary of Opinion’ [399],
“There is no evidence that Mr Snow had any psychiatric problems prior to the diagnosis of his rectal tumour in November 2015.”
“27. From my examination of Mr Snow, and reviewing his extensive notes and complex physical details, I consider he shows evidence of having suffered a significant Stress Reaction, best described as a prolonged Adjustment Disorder with Depression, as outlined in section F43.21 in ICD-10. This has been characterised by enhanced anxiety, social withdrawal, angry feelings about what has happened to him, suicidal ideation at times, a loss of general wellbeing, and depressive ideation.”
“1) Are the experts able to agree the Claimant’s
a) current psychiatric condition, including symptoms, quality of life, and functional capacity, including fitness to work, and to undertake domestic duties and recreations?
We agree that Mr Snow‘s current condition reflects an adjustment disorder of moderate severity, characterised by enhanced anxiety, depression, considerable anger and frustration, and distress from the range of physical symptoms that he is experiencing, particularly bowel and bladder difficulties and sexual dysfunction. We agree that these symptoms affect his quality of life, and the limitations in terms of his marital relationship.
…
1c) psychiatric prognosis, with regard to symptoms, quality of life, and functional capacity, including fitness to work to normal retirement age, and to undertake domestic duties and recreations?
We agree that the psychiatric prognosis is the gradual improvement in his Adjustment Disorder with the passage of time and any improvements that can be obtained in his physical state (and in this regard we defer to surgical expertise). We agree that the main impairments in terms of the Claimant’s quality of life and functional capacity are his physical limitations, and from the psychiatric perspective there is no indication that he would not be fit to work until normal retirement age, or undertake domestic duties and recreational activities.
2. Are the experts able to agree the cause of the Claimant’s psychiatric condition?
We agree that the development of a substantial Adjustment Disorder was caused by the complex pattern of physical symptoms that the Claimant experienced after the index operation, these including bowel dysfunction, urinary dysfunction, loss of sexual function, and persisting pain. We agree that but for the index event and the physical difficulties generated thereby, on balance he would not have developed an Adjustment Disorder.
4) If the Court finds that the Claimant would have developed similar physical complications in any event, but that he would have been warned of the risks of such complications pre-operatively, would he have avoided any psychiatric injury?
We agree that the development of similar physical complications in this scenario would in itself still have generated a significant Adjustment Disorder, but had he been appropriately counselled and warned of the risks of such complications, this would have resulted in an absence or reduction in his degree of anger and frustration. In this regard therefore his pattern of physical symptoms in themselves would still have generated a significant Adjustment Disorder, but of mild severity. He would thus not have avoided any psychiatric injury.
5) If the answer to question 4) is no, what would the nature, severity and duration of the psychiatric injury have been?
We agree that given the nature of the symptoms he would have experienced, on balance Mr Snow would have developed an Adjustment Disorder of mild (i.e. lesser) severity, and not characterised by the intense anger and anxiety that he has developed. The duration of this condition would have been slightly less than that which has occurred.”
Impact of injuries on Claimant’s social life
Discussion
i) Permanent total impotence, loss of ejaculation and anorgasmia £100,000
ii) Faecal urgency and passive incontinence £85,000
iii) Serious impairment of bladder control with urinary urge incontinence
£65,000
iv) Prolonged adjustment disorder with moderately severe depression
£25,000
v) Moderate rectal pain, bleeding and tenesmus £21,070
£296,070
Less 20% deduction for overlap of PSLA £236,856
Findings as to general damages for PSLA
“34. It is in my judgment always necessary to stand back from the compilation of individual figures, whether assistance has been derived from comparable cases or from the [Judicial College] guideline advice, to consider whether the award for pain, suffering and loss of amenity should be greater than the sum of the parts in order properly to reflect the combined effect of all the injuries upon the injured person's recovering quality of life or, on the contrary, should be smaller than the sum of the parts in order to remove an element of double counting. In some cases, no doubt a minority, no adjustment will be necessary because the total will properly reflect the overall pain, suffering and loss of amenity endured. In others, and probably the majority, an adjustment and occasionally a significant adjustment may be necessary.”
6 Injuries to Internal Organs
(E) Reproductive System: Male
The level of awards in this area will typically depend on:
(i) effect on fertility;
(ii) pain and sexual dysfunction;
(iii) hormonal effects;
(iv) whether or not the affected person already has children and/or whether the intended family was complete;
(v) scarring;
(vi) psychological reaction;
(vii) medical complications.
(b) Total impotence and loss of sexual function and sterility in the case of a young person.
The level of the award will depend on:
(1) age
(2) whether the person already has children;
(3) pain or scarring
(4) hormonal effects
(5) psychological reaction and the effect on social and domestic life.
The bracket is £114,900 to £148,320.
(c) Impotence or significant sexual dysfunction which is likely to be permanent, in the case of a person with children or who would not have had children in any event.
The bracket is £43,010 to £88,750.
“11) In relation to the sexual dysfunction, it is important to note that JCG 6Ec relates to ‘Impotence or significant sexual dysfunction which is likely to be permanent, in the case of a person with children or who would not have had children in any event’.
12) In this case the bracket is not adequate as the Claimant has total erectile dysfunction, he is at the end of the road with medications and may undergo surgery, and he also has ejaculatory loss and anorgasmia due to the multiple nerve injuries. Hence the higher award contended for.”
(J) Bladder
(c) Serious impairment of control with some pain and incontinence.
The bracket is £63,980 to £79,930.
6 Injuries to Internal Organs
(I) Bowels
(c) Faecal urgency and passive incontinence persisting after surgery and causing embarrassment and distress, typically following injury giving birth.
In the region of £79,920.
4. Psychiatric and Psychological damage
(A) Psychiatric Damage Generally
The factors to be taken into account in valuing claims of this nature are as follows:
(i) the injured person’s ability to cope with life, education and work;
(ii) the effect on the injured person's relationships with family, friends, and those with whom he or she comes into contact;
(iii) the extent to which treatment would be successful;
(iv) future vulnerability;
(v) prognosis;
(vi) whether medical help has been sought.
(b) Moderately severe £19,070 to £54,830
In these cases there will be significant problems associated with factors (i) to (iv) above but the prognosis will be much more optimistic than in (a) above. While there are awards which support both extremes of this bracket, the majority are somewhere near the middle of the bracket.”
Pain and discomfort
“Repeat morphine for abdo and tenesmus pain due to anterior resection syndrome as per recent letters.”
i) Total impotence, loss of ejaculatory function and anorgasmia £88,750
ii) Urinary urgency, incontinence £70,000
iii) Faecal urgency and incontinence £30,000
iv) Prolonged adjustment disorder with moderately severe depression £25,000
£213,750
Interest on general damages for PSLA
Past and future financial losses
Past loss of net earnings and loss of employer’s pension contributions
“62. … I had to decline the offer of work at Rolls Royce, as I could not fulfil the travel requirements due to the severe LARS. … I had to wind up my own company and quit Rolls Royce as I was not able to keep my business running with my unbearable bowel issues. I have lost a lot of contracts.
…
69. The severe symptoms of LARS wreak havoc on my life.”
Gratuitous care and assistance
“The Claimant required assistance from his wife Helen Snow who provided past gratuitous care from 8 February 2016 to the present days. He was/is reliant on his wife Helen Snow to carry out the chores he used to do pre-index injury. Helen Snow transported/accompanied the Claimant to various medical appointments, sorted out his prescriptions and collected his medications from their local chemist; purchased personal/ hygiene and incontinence products; washed and replenished his clothes and underwear, prepared meals for him; carried out weekly shop; took out rubbish bins; cleared garden waste; cut one of the hedges and lawn; gardening; cleaned and maintained home etc.”
“7. I liaised with the GP surgery, I sorted out Malcolm’s appointments and prescriptions, and then collected his medicines from a local chemist. I provided many additional domestic services and personal care to Malcolm which included washing and replenishing his clothes, changing and washing soiled bedlinen and underwear. I bought continence pads and hygiene products for Malcolm, prepared special meals for him as he lost a lot of weight following his operation in December 2015. I also took over the chores which Malcolm used to do: I did the weekly shop, took out rubbish bins, tended the garden and cut the lawn and front hedges (not the laundry hedge which is 2.5 - 3m high) etc. The hours I spent in assisting Malcolm were tapered as time went by.”
i) 8 February 2016 - 31 March 2016: 10 hours a week @ £8.73 per hour, less 25% £495.84
ii) 1 April 2016 - 31 March 2017: 10 hours a week @ £9.30 per hour, less 25% £3,639.37
iii) 1 April 2017 - 31 March 2018: 7 hours a week @ £9.59 per hour, less 25% £2,624.41
iv) 1 April 2018 - 31 March 2019: 7 hours a week @ £10.47 per hour, less 25% £2,865.09
v) 1 April 2019 - 31 March 2020: 5 hours a week @ £11.15 per hour, less 25% £2,185.72
vi) 1 April 2020 - 31 March 2021: 5 hours a week @ £11.45 per hour, less 25% £2,239.41
vii) 1 April 2021 - 20 October 2022: 4 hours a week @ £11.45 per hour, less 25% £2,787.97
Incontinence and hygiene products
“Ever since the Claimant underwent a stoma reversal in February 2016, he suffered/suffers severe LARS and urinary leakage.”
Additional laundry and electricity
Replacement clothing and underwear
Installation of an en-suite toilet in 2017
“Due to the Claimant’s severe LARS, tenemus and faecal and urinary incontinence, he spent/spends a lengthy amount of time in the toilet which causes a great deal of inconvenience to his family. In 2017, their upstairs family bathroom was modified to create an en suite toilet for him, hence work for the family bathroom was also required.
The Claimant incurred £22,117.97 (cost of material £7,157.40 + cost of labour £14,960.57)”
“Malcolm is on the toilet a lot of times so our upstairs family bathroom was modified in 2017 to create an en-suite toilet for him.”
“68. Toilet visits take on average 20 minutes but are often 30 – 60 minutes - I cannot predict when the next bowel movement is coming and have no way of knowing how long a toilet visit will be, even if I have had a recent bowel movement. If and when I have discomfort, stools would be ready to come out so my external sphincter literally can hold on to my stools for a few seconds. Cleaning my bottom takes 5-15 minutes, I literally have to clean faeces from behind my external sphincter, it takes many wipes to remove all that is accessible. This is why I need to get up 2 hours before I leave my house, to get the best chance of emptying my bowel before I set off for work.
…
71. I empty my bladder 8-9 times daily and have to get up at least twice during the night to pass urine. … I always have to sit on the toilet when I pass urine as faeces will often appear.
…
75. We had two toilets in our home but one was marked out for my use because I spent hours on the toilet, defecating and cleaning myself, leaving only one toilet to be shared between Hannah and Helen, which was very inconvenient. It was very difficult for Hannah to bring friends home for obvious reasons. Eventually we installed a 3rd toilet, which meant a complete re modelling and fitting of the bathroom (we created an en suite toilet by using some of the family bathroom), again at our own expense.”
Gardening
Boarding school fees for Hannah Snow
Travel expenses
Cost of winding up AMS 1911 Limited
Summary of past financial losses
i) Past gratuitous care £8,418.81
ii) Incontinence and hygiene products £5,500.38
iii) Additional laundry and electricity £750.00
iv) Replacement clothing and underwear £1,162.00
v) Gardening £945.00
vi) Boarding school fees for Hannah Snow £4,508.00
vii) Transport and travel costs, and sustenance £857.70
£22,141.89
Interest on past financial losses
Future losses
Loss of net earnings
Handicap on the labour market
Treatment costs - Biofeedback
Treatment costs - Botox injections
“This would be a life-long treatment.”
“The risk of requiring intermittent self-catheterisation is probably in the order of 30-40%. The frequency of ISC could be up to x 6 daily. The cost of ISC is that involved in purchasing the catheters which cost between £40 and £70 per month depending on manufacturer.”
Treatment costs - implantation of Sacral Neuromodulation
“144. An alternative option to bladder botox injections is so-called SNS, sacral neuromodulation (using the Interstim). Chronic stimulation of the third sacral nerve root leads to improvement in overactive bladder in something like 60-70% of cases.
145. … Battery replacement is required every 3-7 years or so …
147. Insertion of an SNS would cost about £20000. Battery replacement would probably cost in the order of £8500.”
Treatment costs - implantation of penile prosthesis
“I have still not decided on whether or not to go for the penile implants. It’s a one-way operation. You can’t go back if you have that.”
Cognitive behavioural therapy
“We agree that he would benefit from therapeutic counselling, of between 5 to 10 sessions, and agree that costs would be £80-£200 an hour depending on the experience and qualifications of the therapist. We agreed that he and his wife would also benefit from couple psychosexual counselling, between 10 to 15 sessions, at similar costs.”
“Booster courses of CBT (between 2 to 4 sessions per booster course) may be required 2 or 3 times in the next 2 to 3 years, depending on his initial response to treatment and his physical and psychological state.”
Psychosexual counselling
“We agree that he and his wife would also benefit from couple psychosexual counselling, between 10 to 15 sessions, at similar costs.”
Travelling expenses for medical treatment
Cost of incontinence and hygiene products
Cost of additional laundry
Holiday costs and assistance
“With LARS, travelling long haul is out of the question for me.”
Costs of replacement clothing and underwear
Gardening costs
Summary of future losses
i) Treatment costs - Botox injections £38,371.81
ii) Treatment costs - CBT £3,800.00
iii) Treatment costs - Psychosexual counselling £3,000.00
iv) Travelling for medical treatment £1,103.49
v) Incontinence and hygiene products £26,356.08
vi) Additional laundry £2,845.00
vii) Replacement clothing and underwear £3,983.00
viii) Gardening costs £1,849.40
£81,308.78
Summary of damages
i) General damages for PSLA £180,000.00
ii) Interest on general damages for PSLA £14,764.93
iii) Past financial losses £22,141.89
iv) Interest on past financial losses £401.13
v) Future losses £81,308.78
£298,616.73
[1] Supplemental bundle, 458-474
[2] Supplemental bundle, 566-577
[3] 124-136
[4] 137-146
[5] 147-150
[6] 151-161
[7] 162-163
[8] 164-166
[9] 173-178
[10] Core medical records bundle, 40
[11] Core medical records bundle, 39-40
[12] Core medical records bundle, 41
[13] Core medical records bundle, 38-39
[14] Core medical records bundle, 45
[15] Core medical records bundle, 49
[16] Core medical records bundle, 51
[17] Core medical records bundle, 58
[18] Core medical records bundle, 59-60
[19] Core medical records bundle, 61-63
[20] 126
[21] Core medical records bundle, 59-60
[22] Core medical records bundle, 64-65
[23] Core medical records bundle, 66-67
[24] Core medical records bundle, 75
[25] Core medical records bundle, 72-74
[26] Core medical records bundle, 76-84
[27] Core medical records bundle, 85-86
[28] Core medical records bundle, 110
[29] 157-160
[30] Core medical records bundle, 151-152
[31] Core medical records bundle, 122-126
[32] Core medical records bundle, 155
[33] Core medical records bundle, 178-179
[34] Core medical records bundle, 178-179
[35] Core medical records bundle, 182-183
[36] Core medical records bundle, 194-197
[37] Core medical records bundle, 199-120
[38] Core medical records bundle, 31
[39] Core medical records bundle, 210-211, 215
[40] Core medical records bundle, 259
[41] Core medical records bundle, 268
[42] Core medical records bundle, 276-277
[43] Core medical records bundle, 26
[44] Core medical records bundle, 293-294
[45] Core medical records bundle, 299-30
[46] Core medical records bundle, 311-312
[47] Core medical records bundle, 317-318
[48] Core medical records bundle, 179
[49] Core medical records bundle, 19
[50] Core medical records bundle, 18
[51] Core medical records bundle, 349
[52] Core medical records bundle, 360
[53] Core medical records bundle, 362
[54] Core medical records bundle, 391
[55] Core medical records bundle, 395-396 and 399-400
[56] Core medical records bundle, 407
[57] “Transanal total mesorectal excision: a systematic review of the experimental and clinical evidence” (Araujo et al 2015), supplemental bundle, p. 86-99 at p. 86
[58] 608
[59] Anastomosis is the connection of two e.g. passageways, in this case the colon and the anus.
[60] Supplemental bundle, 125-131 at 126
[61] Supplemental bundle, 587
[62] 606-607
[63] 615
[64] 615
[65] 616-617
[66] 788-791 at 788
[67] 788-791 at 790
[68] Supplemental bundle, 325
[69] Supplemental bundle, 327-330
[70] 52
[71] 1832
[72] 616
[73] 606-607
[74] 1769-1786
[75] 1770
[76] 1772
[77] 1813-1818
[78] 737
[79] Transcript, 25 October 2022, p. 100
[80] 628
[81] Transcript, 25 October 2022, p. 107, lines 10-12
[82] Transcript, 25 October 2022, p. 100
[83] Transcript, 21 October 2022, p. 136
[84] 628
[85] Transcript, 21 October 2022, p. 136
[86] 607
[87] Transcript, 21 October 2022, p. 104
[88] Transcript, 21 October 2022, p. 102
[89] 606
[90] Supplemental bundle, 586
[91] Core medical records bundle, 75
[92] Supplemental bundle, 7-8
[93] 157
[94] Transcript, 21 October 2022, p. 94
[95] Transcript, 25 October 2022, p. 133
[96] Transcript, 24 October 2022, p. 82-83
[97] 610-612
[98] 157
[99] Transcript, 21 October 2022, p. 126, lines 20-25 and p. 127, lines 1-2
[100] Transcript, 21 October 2022, p. 127, lines 8-12
[101] Transcript, 21 October 2022, p. 127, lines 13-18
[102] Transcript, 21 October 2022, p. 127, lines 19-21
[103] Transcript, 21 October 2022, p. 127, lines 22-24
[104] Transcript, 21 October 2022, p. 127, line 25 and p.128, line 1
[105] Transcript, 21 October 2022, p. 128, lines 13-16
[106] 299
[107] 189
[108] 616
[109] Transcript, 25 October 2022, p. 76
[110] 1832
[111] Transcript, 25 October 2022, p. 76, lines 4-9
[112] 588
[113] Transcript, 25 October 2022, p. 76, lines 4-9
[114] Supplemental bundle, 592
[115] 194
[116] 332
[117] 153
[118] 615
[119] 153
[120] Core medical records bundle, 91-93
[121] Transcript, 21 October 2022, p. 137-138
[122] 197
[123] 356
[124] Transcript, 27 October 2022, p.30-31
[125] 130
[126] 142
[127] 194
[128] Supplemental bundle, 573
[129] 348
[130] Supplemental bundle, 568
[131] 606-614
[132] 607
[133] 153
[134] Transcript, 25 October 2022, p. 76, lines 4-9
[135] 1825-1831
[136] 607
[137] 153
[138] 163
[139] 788-791
[140] Supplemental bundle, 327-330
[141] Supplemental trial bundle, 568-569
[142] 152
[143] Core medical records bundle, 59
[144] Transcript, 21 October 2022, p. 113 and 115
[145] 126
[146] 1550
[147] Transcript, 20 October 2022, p. 62
[148] Transcript, 21 October 2022, p. 30-31
[149] Transcript, 20 October 2022, p. 92
[150] 125
[151] 127
[152] 152
[153] 165
[154] 126
[155] 1527
[156] Transcript, 20 October 2022, p. 91-92
[157] 152
[158] 162-163
[159] Transcript, 21October 2022, p. 115
[160] 41
[161] Core medical records bundle, 59-60
[162] Core medical records bundle, 59-60
[163] 59
[164] 1832
[165] 53
[166] Core medical records bundle, 43
[167] Core medical records bundle, 54
[168] Transcript, 24 October 2022, 76-78
[169] Transcript, 25 October 2022, p. 54 lines 18-25 and p. 55 lines 1-2
[170] 153
[171] 179-216
[172] 217-218
[173] 391-432
[174] 491-499
[175] 516-526
[176] 329-349
[177] 350-378
[178] 453-462
[179] 463-472
[180] 503-511
[181] 530-592
[182] Supplemental bundle, 1-50
[183] Supplemental bundle, 579-632
[184] 481-490
[185] 513-515
[186] Supplemental bundle, 633-638
[187] Supplemental bundle, 695-696
[188] 602-605
[189] Transcript, 25 October 2022, p.22-23
[190] 334
[191] Transcript, 21 October 2022, 124, lines 9-11
[192] Experts’ duties provide (See Ministry of Justice website: https://www.justice.gov.uk/courts/procedure-rules/civil/standard-directions/general/experts),
“Any unpublished literature upon which any expert witness proposes to rely must be served at the same time as service of his report, together with a list of published literature.”
[193] 213
[194] Transcript, 26 October 2022, p. 12-13
[195] Transcript, 26 October 2022, p. 31
[196] Supplemental bundle, 580
[197] Transcript, 25 October 2022, p. 109
[198] 187
[199] Supplemental bundle, 581 and 593
[200] Transcript, 25 October 2022, p. 91
[201] 343
[202] Core medical records bundle, 49
[203] Core medical records bundle, 58
[204] Core medical records bundle, 59-60
[205] 153
[206] 514
[207] Supplemental bundle, 635 and 638
[208] Supplemental bundle, 580
[209] Supplemental bundle, 580-581 and 624
[210] Transcript, 25 October 2022, p. 89-91
[211] Transcript, 25 October 2022, p. 91
[212] Transcript, 25 October 2022, p. 24
[213] 54
[214] 189-190
[215] Supplemental bundle, 620 and 624
[216] 343 and 345
[217] Transcript, 26 October 2022, p. 17
[218] Transcript, 21 October 2022, p. 122
[219] Transcript, 21 October 2022, p. 123-124
[220] Supplemental bundle, 695
[221] 191-192
[222] Supplemental bundle, 14
[223] 624 and 628
[224] 848
[225] 103-112 at 103, 109 and 111
[226] 329-349
[227] Transcript, 25 October 2022 at p. 115
[228] Transcript, 25 October 2022 at p. 121
[229] 334
[230] Transcript, 25 October 2022 at p. 120
[231] 191-192
[232] See paragraph 213 above.
[233] See paragraph 214above.
[234] 208
[235] 486
[236] 487
[237] 129
[238] 141
[239] 455
[240] 224
[241] 486
[242] Transcript, 21 October 2022, p. 137-138
[243] Transcript, 24 October 2022, 92
[244] 1045-1047
[245] 1047-1050
[246] Supplemental bundle, 669-678
[247] Supplemental bundle, 670
[248] Supplemental bundle, 671
[249] Transcript, 24 October 2022, p. 36
[250] Transcript, 24 October 2022, p. 37-38
[251] Transcript, 24 October 2022, p. 64, lines 23-24
[252] Transcript, 24 October 2022, p. 65, lines 11-13
[253] Transcript, 24 October 2022, p. 65
[254] Transcript, 24 October 2022, p. 66
[255] Transcript, 24 October 2022, p. 67
[256] Transcript, 26 October 2022, p. 57, 59, 60 and 61
[257] Transcript, 25 October 2022, p. 63
[258] Transcript, 25 October 2022, p. 64
[259] 1045-1058
[260] 1050
[261] 812
[262] 1068
[263] 1026
[264] 1032-1033
[265] Transcript, 26 October 2022, p. 62
[266] 1050
[267] Transcript, 24 October 2022, p. 64, lines 23-24
[268] Transcript, 24 October 2022, p. 65, lines 11-13
[269] Transcript, 21 October 2022, p. 138
[270] 197
[271] Supplemental bundle, 585
[272] Transcript, 24 October 2022, p. 98-100
[273] Transcript, 25 October 2022, p. 122
[274] Supplemental bundle, 585
[275] Transcript, 24 October 2022, 92-94
[276] 1704-1706
[277] 198
[278] Transcript, 24 October 2022, p. 96, lines 22-25
[279] Transcript, 24 October 2022, p. 98, line 16
[280] Transcript, 26 October 2022, p. 128-130
[281] 420
[282] Transcript, 21 October 2022, p. 140
[283] 344
[284] Transcript, 25 October 2022, p. 68
[285] Transcript, 25 October 2022, p. 69
[286] Core medical records bundle, 64-65 at 65
[287] 619-631
[288] 624 and 628
[289] Transcript, 24 October 2022, p. 38 and 93
[290] Transcript, 26 October 2022, p. 93
[291] Transcript, 26 October 2022, p. 129
[292] Transcript, 26 October 2022 p.63
[293] Transcript, 26 October 2022, p. 26
[294] Supplementary bundle, 671
[295] 1006
[296] 65
[297] Transcript, 25 October 2022, p. 57
[298] 992
[299] 1020-1025
[300] 1037-1042
[301] 1005-1006
[302] 1006
[303] 1032-1036
[304] Supplemental bundle, 584
[305] 1067-1077
[306] Transcript, 26 October 2022, p. 115
[307] 425
[308] 1067-1068
[309] 1069
[310] 460
[311] See Mr Courtney’s witness statement at paragraph 3, p. 165
[313] 467-468
[314] 403-404
[315] 468
[316] 223
[317] 486
[318] 486
[319] 486
[320] 198
[321] 54-55
[322] 335-336
[323] 425
[324] 387
[325] 992
[326] 1037-1042
[327] 1032-1036
[328] 611
[329] 485
[330] 459
[331] 335-336
[332] Transcript, 25 October 2022 p.147-148
[333] Supplemental bundle, 196
[334] Supplemental bundle, 652
[335] 793-802 at 793 and 797
[336] Supplemental bundle, 594
[337] 205
[338] 208
[339] 370
[340] Not included in the trial bundles
[341] 212
[342] Supplemental bundle, 101-102 at 101
[343] 812
[344] 829
[345] 838
[346] Supplemental bundle, 177-183 at 182
[347] Transcript, 25 October 2022, p. 16, 18 and 24
[348] Supplemental bundle, 658
[349] Transcript, 25 October 2022, p. 13
[350] 373
[351] Transcript, 25 October 2022, p. 71
[352] Supplemental bundle, 583
[353] Supplemental bundle, 602
[354] Supplemental bundle, 609
[355] Supplemental bundle, 612-613
[356] Supplemental bundle, 613
[357] Supplemental bundle, 614
[358] Supplemental bundle, 617
[359] Supplemental bundle, 651
[360] Supplemental bundle, 652 and 654-655
[361] Supplemental bundle, 199
[362] Supplemental bundle, 199
[363] Supplemental bundle, 658-668
[364] Supplemental bundle, 613
[365] See Dr Burling at p. 497 (“From a radiology perspective alone, the decision to surgically excise the entire rectum and its surrounding mesorectum was appropriate”) and Dr Scullion at p. 509 (“Excision of the tumour and total mesorectum seemed appropriate”).
[366] Core medical records bundle, 372
[367] Transcript 25 October 2022, p. 19, lines 20-21
[368] Transcript, 25 October 2022, p.22-23
[369] 370 and 373
[370] 46
[371] 509
[372] 497
[373] Transcript, 24 October 2022, 19-21
[374] 513-514
[375] 346
[376] 598
[377] 603
[378] 199-200
[379] Transcript, 25 October 2022, p. 37-39
[380] Supplemental bundle, 621-622
[381] Transcript, 24 October 2022, 19-21
[382] 200-201
[383] 212
[384] 373
[385] Supplemental bundle, 45
[386] Transcript, 25 October 2022, p. 37-39
[387] Supplemental bundle, 618
[388] 812
[389] Supplemental bundle, 627
[390] Mr Moran’s letter to the Claimant’s GP is in the medical records bundle, p. 197-198
[391] See Mr Meleagros’ report dated 22 June 2022 at paragraph 6.16 (p. 371)
[392] 371
[393] 145
[394] 145
[395] 224
[396] 488
[397] 222-223
[398] 524
[399] 531
[400] 523
[401] 602
[402] 1207
[403] Medical records bundle
[404] 133
[405] Supplemental bundle, 445-448
[406] Supplemental bundle, 448
[407]134
[408] 134
[409] 135
[410] 427
[411] 488
[412] 427
[413] Transcript, 21 October, p. 61
[414] 603
[415] 525
[416] 603
[417] See paragraph 454 above for calculation of multiplier
[418] 135