Freely Available British and Irish Public Legal Information
[Home] [Databases] [World Law] [Multidatabase Search] [Help] [Feedback]
England and Wales High Court (Administrative Court) Decisions
You are here: BAILII >> Databases >> England and Wales High Court (Administrative Court) Decisions >> Hexpress Healthcare Ltd, R (On the Application Of) v Care Quality Commission [2022] EWHC 2943 (Admin) (25 November 2022)
URL: http://www.bailii.org/ew/cases/EWHC/Admin/2022/2943.html
Cite as: [2022] EWHC 2943 (Admin)
[New search] [Printable PDF version] [Help]
Neutral Citation Number: [2022] EWHC 2943 (Admin)
Case No: CO/3901/2022
IN THE HIGH COURT OF JUSTICE
KING'S BENCH DIVISION
ADMINISTRATIVE COURT
Royal Courts of Justice
Strand, London, WC2A 2LL
Date: 25/11/2022
Before :
MR JUSTICE MOSTYN
- - - - - - - - - - - - - - - - - - - - -
Between :
|
|
THE KING (on the application of HEXPRESS HEALTHCARE LIMITED) |
Claimant |
|
|
- and – |
|
|
|
CARE QUALITY COMMISSION |
Defendant |
- - - - - - - - - - - - - - - - - - - - -
- - - - - - - - - - - - - - - - - - - - -
Philip Havers KC and Lucy McCann (instructed by Ridouts) for the Claimant
Daniel Stilitz KC and Stephanie David (instructed by CQC) for the Defendant
Hearing date: 15 November 2022
- - - - - - - - - - - - - - - - - - - - -
Approved Judgment
Mr Justice Mostyn:
1. This is my judgment on the claimant’s application for:
i) permission to apply for judicial review of the defendant’s decision to publish its report dated 20 October 2022 of its inspection of the claimant’s services on 17 May 2022; and
ii) if permission is granted, an injunction prohibiting the publication of the report until the hearing of the substantive judicial review application.
I have had the benefit of extensive written and oral submissions of high quality from Leading Counsel for each party, and I have considered a considerable quantity of written material (the bundles contain 921 pages). I therefore consider that I am in a position to give a fully reasoned judgment.
2. The claimant (“the provider”) is an online medication prescribing service available to patients aged 18 or over, which is registered with the defendant (“the CQC”).
The legislative scheme
3. The CQC is the statutory body entrusted by Parliament under the Health and Social Care Act 2008 (“the Act”) with the responsibility for registering and reviewing the providers of health and social care services in England.
4. Under s. 3(1) of the Act the main objective of the CQC is stated to be to protect the health, safety and welfare of people who use health and social care services.
5. Under s. 4(1) in performing its functions the CQC must have regard, among other things, to:
“(e) the need to ensure that action by the Commission in relation to health and social care services is proportionate to the risks against which it would afford safeguards and is targeted only where it is needed
…
(g) best practice among persons performing functions comparable to those of the Commission
(including the principles under which regulatory action should be transparent, accountable and consistent).”
6. Under s. 10 it is an offence to carry on a regulated activity without being registered. Under s. 8 “regulated activity” means an activity of a prescribed kind. Under Paragraph 4(1) of Schedule 1 to the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014 (SI 2014/2936) (“the Regulations”) the provision of treatment for a disease, disorder or injury by a health care professional is a prescribed regulated activity.
7. Under s. 29, if it appears to the CQC that a registered person has failed to comply with requirements imposed by it, the CQC may give that person a warning notice. Under s. 33 failure to comply with the warning is an offence.
8. Under s. 46(1) the CQC must (i) conduct reviews of the carrying on of regulated activities by service providers; (ii) assess their performance following each such review; and (iii) publish the reports of its assessments.
9. Under s. 46(4) and (5) the CQC must publish a statement which (i) sets out the frequency with which reviews are to be conducted; and (ii) contains a description of the method that it proposes to use in assessing and evaluating the performance of a provider.
10. Under s. 60(1)(a) of the Act the CQC may for the purposes of its regulatory functions carry out inspections of the carrying on of a regulated activity. Under s.61, where such an inspection is carried out, the CQC must (i) prepare a report on the matters inspected; (ii) without delay send a copy of the report to the person who carries on the regulated activity in question; and (iii) publish the report.
11. Under Regulation 20A of the Regulations, where a report gives a rating, the service provider must display that rating conspicuously and legibly in each and every place where the regulated activity is delivered, and on its website, where people will be sure to see it.
12. The Regulations specify the fundamental standards to be applied in the care and treatment of service users. Regulation 9 states that the care and treatment of service users must be appropriate, meet their needs, and reflect their preferences. Regulation 10 says that service users must be treated with dignity and respect. Regulation 12 states that care and treatment must be provided safely. Regulation 17 requires good governance.
13. Pursuant to s 46(4) & (5) of the Act the CQC has published a Provider Handbook in which it explains that it will give ratings of services in five “domains”:
i) Are services safe?
ii) Are services effective?
iii) Are services caring?
iv) Are services responsive to people’s needs?
v) Are services well-led?
14. For which the possible ratings (with colour coding) are
i) Outstanding ☆
ii) Good ●
iii) Requires Improvement ●
iv) Inadequate ●
15. Obviously, the publication of a report with poor ratings on the websites of both of the CQC and the provider, has the potential to wreak serious economic and reputational damage. Yet, neither the Act nor the Regulations grant any form of redress by way of appeal, or other form of challenge, to a provider who is aggrieved by a report proposed to be published under s. 46 or s. 61. The statutory silence leaves the only forms of redress to judicial review proceedings or a complaint to the Parliamentary and Health Services Ombudsman.
Correction of factual errors
16. The CQC recognised the potential unfairness of it publishing a report without affording even the most limited “Maxwellisation” process (i.e. giving a person criticised in the report the opportunity prior to publication to identify factual errors and to seek their correction).
17. Therefore, its Handbook as originally published provided for a procedure to challenge factual findings made and ratings awarded. In R (On the Application of SSP Health Ltd,) v Care Quality Commission [2016] EWHC 2086 (Admin) at [11] Andrews J described the procedure:
“i) prior to publication, service providers can challenge the factual accuracy and completeness of the evidence and findings on which the ratings are based, as well as the proposed ratings themselves. The service provider has 10 working days in which to review draft reports and submit its comments to the CQC. There is no express provision for the submission of evidence that was not produced at the time of the inspection.
ii) after publication, service providers can seek a review of ratings. The Handbook makes it plain that the only grounds for requesting such a review is that CQC did not follow the process of making ratings decisions and aggregating them (i.e. the process set out in the Handbook). Service providers cannot request reviews on the basis that they disagree with the judgments made by CQC, "as such disagreements would have been dealt with through the factual accuracy checks…".”
18. The case before me is about the first scenario: the correction of factual errors before publication.
19. In SSP at [52] Andrews J identified the key issue before her:
20. To which her answer at [69] was:
21. Andrews J makes clear in her judgment that the factual accuracy check (FAC) process only applies to primary concrete facts which can be objectively shown by reference to documents or other hard evidence to be “demonstrably ill-founded” ([45] or “inaccurate, untrue or misleading” ([48]). Therefore, the process does not extend to a finding about an abstract fact (e.g. a person’s state of mind) or to a decision which results from an evaluation of the primary concrete (or abstract) facts [1]. Such findings and decisions require a subjective judgment by the fact-finder, about which views may differ without any being wrong. In contrast, a primary concrete fact either happened or it did not.
“51. Therefore, if and to the extent that complaint is made by the Claimant that the CQC refused a review of the report after publication on a basis which had not been raised at the appropriate time, i.e. in the factual accuracy comments log, the complaint is not well-founded. Procedural fairness in this context does not require the regulator to give a regulated body two bites of the same cherry. On the other hand, if fairness required an amendment and the amendment was not made, there is no reason to shut out the complainant from elaborating on its objections if they were raised at the appropriate stage.
…
59 … an independent person within the CQC itself, applying common sense as well as his or her professional expertise, ought to be able to tell fairly swiftly whether there is or is not a legitimate grievance about the Lead Inspector's failure to correct the report. Such a person should be much better placed to resolve that grievance than this court is. A review process is unlikely to occupy as much valuable time of senior personnel as litigation and it certainly will not cost as much. It need not hold up the publication of the report, though there may be cases in which fairness would require a short delay because otherwise irreversible damage might be done to the reputation of the practice concerned. …
23. This has been interpreted to mean that the sequence should be as follows:
i) the CQC inspection team sends the draft report to the provider;
ii) the provider sends to the CQC its list of alleged factual inaccuracies with reasons (“the FAC list”);
iii) the CQC inspection team prepares its response to the FAC list (“the CQC response”);
iv) the CQC then sends its response to the provider;
v) if the CQC response is not accepted by the provider then it spells out its reasons in a reply (“the reply”) and at the same time seeks an independent internal review of the CQC inspection team’s response in the light of the reply;
vi) an independent reviewer considers the draft report, the FAC list, the CQC response, and the reply and makes a recommendation;
vii) in the light of the recommendation the CQC inspection team then makes a final decision; and
viii) the report is then finalised and published.
24. This interpretation was approved by Holgate J in R (Babylon Healthcare Ltd) v Care Quality Commission [2017] EWHC 3436 (Admin), where he held at [82]-[83]:
“The Defendant says that it is sufficient that an independent reviewer should contribute to the document responding to the service provider's comments before that document is issued, together with the final s.61 report for publication, and before those documents are given to the service provider. On the other hand, the Claimant says that that does not go far enough. They say that, according to the judgment of Andrews J, it is necessary that the service provider should see the response of the inspection team. It can then ask for an independent review, and that review will separately indicate whether any additional changes should or should not be made. In other words, they say, the two responses should not be conflated.
I agree with the Claimant that that was what was intended by Andrews J…”
I am not so sure.
25. It seems to me that this elaborate, and time-consuming, exercise is likely to be a work of supererogation. In this case, after the provider submitted the FAC list, the CQC inspection team formulated its response and accepted some of the proposed corrections. The CQC response was then independently reviewed internally. That review found no reasons to change the CQC response. Accordingly on 20 October 2022 the CQC sent the provider a composite document containing the CQC response and the record of the review, along with the finalised report.
26. Mr Stilitz KC informed me that the CQC now routinely has the response to every FAC request checked by an independent reviewer.
27. The CQC therefore has condensed the process as follows:
i) the CQC inspection team sends the draft report to the provider;
ii) the provider sends to the CQC its FAC list;
iii) the CQC inspection team prepares its response to the FAC list;
iv) an independent reviewer considers the draft report, the FAC list, and the CQC response, and makes a recommendation;
v) in the light of the recommendation the CQC inspection team then makes a final decision; and
vi) the report is then finalised and published.
28. It can be seen that this process is considerably shorter than that set out at [23] above.
29. I do not consider that this process is at odds with the judgment of Andrews J. I do not read it as saying that the independent reviewer must see the reply of the provider before embarking on the review, although it is true that Holgate J has read it that way.
30. If I am wrong about the meaning of Andrews J’s judgment, I must find a powerful reason for not following it (see Willers v Joyce (No 2) [2016] UKSC 44 at [9]). The avoidance of a time-wasting work of supererogation is in my judgment a powerful reason for not following it.
31. What has the provider lost if the process is thus condensed? All that has been lost is that the reviewer will not see the “reply” of the provider at stage (v) of [23] above. Frankly, I cannot see that as a great loss which justifies such a prolongation of the procedure. I remind myself that we are talking here about errors of primary concrete fact, and not about value judgments on those primary facts. Those errors will have been clearly pointed out in the initial FAC request by the provider. They will either be right or wrong. If the alleged errors are rejected by the inspection team they will have had to have done so for good reasons, referable to hard objective evidence. It is hard to see what the reply can contribute further to the debate.
32. Mr Stilitz KC has pointed out to me that when an inspection has taken place, time is of the essence when preparing the consequential report. Given the nature of the main objective of the CQC, namely to protect the public, I can readily understand that. This key factor strongly militates in favour of the condensed process.
33. I therefore do not accept the argument by Mr Havers KC (and must respectfully disagree with my colleague) as to the point when the independent reviewer is introduced into the process. In my opinion the factual correction procedure adopted by the CQC in [27] above is fair and therefore lawful.
The facts of this case
34. The provider’s service does not involve face-to-face interactions between the patient and the clinician. The provider prescribes medication for over 60 conditions. Patients who wish to obtain treatment for a certain condition are required to fill in an online set of medical questions specific to that condition in order to provide information on whether the medication is suitable for the patient’s needs in light of their presenting symptoms and their past medical history.
35. If the answers comply with indications for that condition, the form is reviewed by a doctor who uses professional judgement to write a prescription. The prescription is then dispensed either by the provider’s pharmacy team through the post or by a pharmacy of the patient’s choice. This is, as understood by the CQC, a different service model from General Practice but nonetheless one that requires a high degree of care and caution.
36. Shortly after the provider had registered, the CQC carried out an inspection of the provider’s service on 22 August 2018. The CQC did not rate the provider following this inspection. There was a further inspection on 9 May 2019. The service achieved a ranking of “Good” overall.
37. On 12 July 2021, the CQC carried out a remote review of the provider’s service and was satisfied that no further inspection was required. A further remote review took place on 13 September 2021 with the same outcome. However, at this time, between 28 April 2021 and 14 August 2021, five concerning incidents took place. One patient suffered from a non-fatal overuse of Saxenda, a weight loss injection pen. Two suffered from non-fatal overdoses, and two from fatal overdoses, of the beta-blocker propranolol. The claimant in response changed its systems before suspending propranolol prescriptions entirely.
38. These five incidents were brought to the CQC’s attention. As it happens, a decision to inspect the service was already in train following receipt of three unconnected notifications by the CQC: two from GPs and one from the General Pharmaceutical Council, which also regulates the provider. One notification concerned the safe prescribing of Bendroflumethiazide (a diuretic used to treat hypertension), the second concerned propranolol and the third related to antibiotic prescribing.
39. On 17 May 2022 an announced, fully comprehensive inspection took place. Its remit was the fundamental standards of care and the safety of the service of the provider as a whole.
40. The inspection team was headed by a lead inspector of the CQC and included a second CQC inspector, a GP specialist adviser, and a member of the CQC medicines team.
41. It is only practically possible for the inspection team to examine a sample of medical records. The sample is randomly selected and its size is advised by a healthcare specialist in the CQC. That adviser is not a statistician.
42. Out of 60,000 medical records available, the CQC randomly selected 9 to review. However, 3 of those were for technical reasons unreviewable, producing no evidence. Therefore the sample size was 6, representing 0.01% of all patient records. Out of these 6 records, 5 raised concerns.
43. The evidence generated by the inspection included, crucially, conclusions that were drawn from the review of the sample. In addition, the evidence included two interviews with the provider’s doctors, and a review of the various policies of the provider.
44. On 30 June 2022, the CQC supplied the provider with its draft report resulting from their inspection of 17 May 2022. The ratings were as follows:
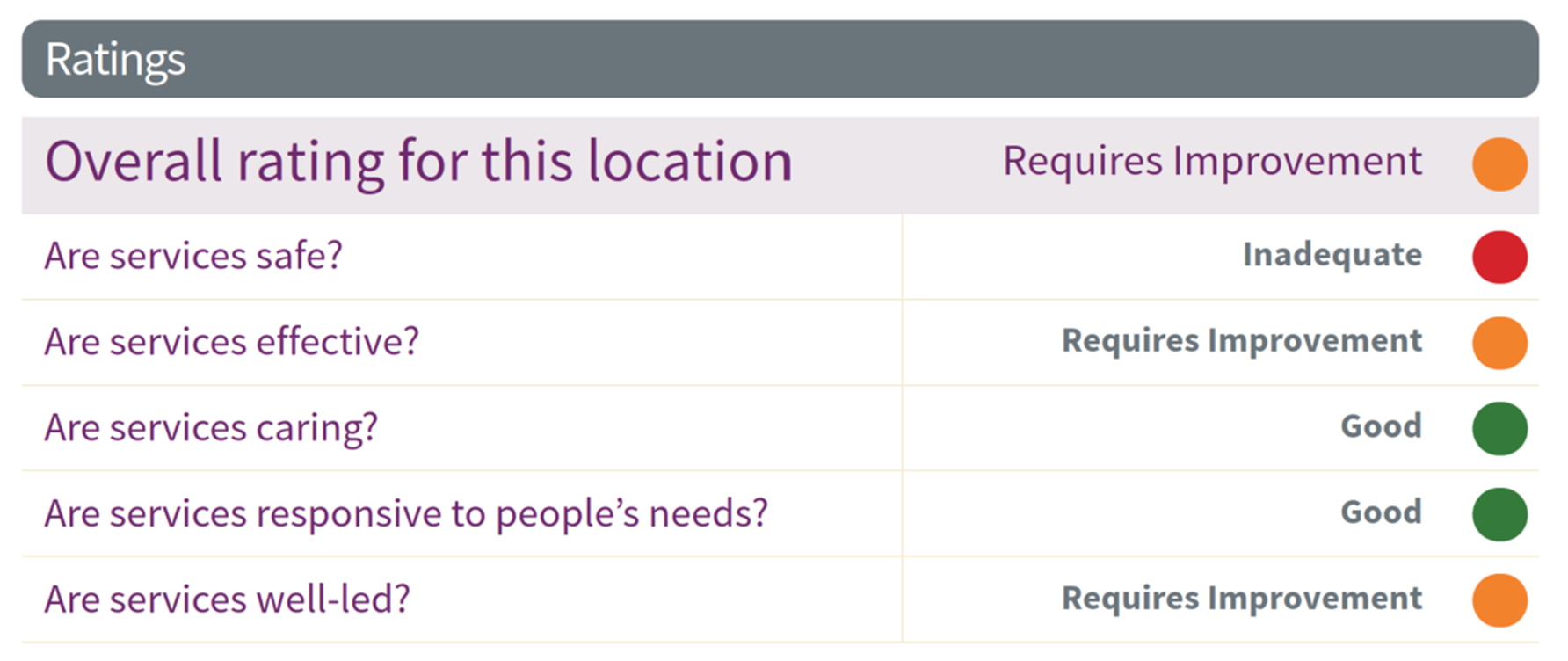
45. The provider submitted its FAC list to the CQC on 14 July 2022.
46. The draft report also contained a Requirement Notice under Regulation 17 and an Enforcement Notice under Regulation 12. On 5 July 2022, the CQC issued the provider with a Warning Notice under s. 29 of the Act for an alleged breach of Regulation 12. Representations were made by the provider’s solicitors to the CQC regarding the notice. On 30 August 2022, the CQC agreed with the provider’s representations, and withdrew it. In its letter of that day the CQC stated that having considered the provider’s representations, they considered that “the threshold for the assessed level of risk may not have been reached … for the serving of a warning notice.”
47. On 20 October 2022, the CQC provided the provider with the final inspection report together with confirmation that the report and its response to the factual accuracy comments would be published on 25 October 2022. The ratings remained unchanged; the Requirement Notice in respect of Regulation 17 remained in place; and a Requirement Notice was issued in respect of Regulation 12.
The judicial review challenge
48. On 24 October 2022, the provider issued an application for permission to seek judicial review and further applied for an interim injunction restraining the CQC from publishing the report pending further order. On 25 October 2022, Ritchie J considered the provider’s urgent injunction application and listed the application to be heard. At the consequential hearing on 26 October 2022, Holgate J directed that the publication of the report was to be restrained until the permission application was determined, and directed the permission and interim relief hearing which is before me.
49. There are five grounds of challenge:
i) Ground 1: The CQC failed to give reasons for departing significantly from its findings in earlier inspection reports.
ii) Ground 2: The CQC acted disproportionately, and thereby breached s.4(1)(e) of the 2008 Act, by using only six medical records as its sample.
iii) Ground 3: The CQC failed to independently review the FAC response, which was procedurally unfair.
iv) Ground 4: The CQC irrationally assessed the safety of the provider’s services as inadequate.
v) Ground 5: The final report contained errors of fact or else gives undue weight to irrelevant factors.
Ground 1
50. The reason that the provider was given a clean bill of health on each of the previous inspections was because nothing of concern was revealed in the records that were sampled. This illustrates the perils of using statistically insignificant samples. However, it is not a valid criticism to say that the CQC failed to give reason for departing from its earlier findings. It did not need to give reasons because it must have been apparent from reading the report that its conclusions were based on problems revealed in a tiny sample, which problems were not revealed in equally small samples on the previous occasions.
51. As framed, Ground 1 is not arguable.
Ground 2
52. The CQC has consistently maintained that for such a “high proportion” of issues to emerge from the sample was very worrying. For example, in its Grounds of Defence it stated:
“…while the sample was relatively small, a very worryingly high proportion of the records examined contained issues”.
53. There is no doubt that the worrying revelations in the sample of six records played a major role in the evidence cited in the report, in the conclusions that were reached, and in the ratings that were given.
54. So, in the section “Are services safe?” the report states:
“The service stated that they did not prescribe certain medicines and for some long-term conditions without receiving adequate documentation from the individual’s doctor. However, we found that the service had continued to issue medicines for a particular patient without receiving any clearance from the patient’s own GP or ensuring they had received kidney function tests. We saw no evidence that any information had been requested.”
…
“We found instances where patients requesting antibiotics for a urinary tract infection, were prescribed antibiotics without a record of the presenting symptoms or past medical history. For example, in one patient record we reviewed, there was no record of any history of past urine infections or if the patient had a recent urine sample tested. However, a prescription was generated for antibiotics for this patient without a record of the clinical decision to prescribe.”
55. In the section “Are services effective?” it states:
“We reviewed six anonymised medical records which were complete records. We saw that notes were recorded, and the GPs working for the provider had access to all previous notes. However, we saw examples where patient records lacked adequate documentation to support prescribing. Some records lacked a detailed assessment of the patient’s presenting symptoms for example, when prescribing antibiotics. We were told that each clinician was required to complete 25 prescriptions per hour. However, we found in most cases, prescriptions were generated in under 30 seconds and in some instances in 15 seconds. Resulting in instances where prescribing was not in line with the services policy.”
…
“Before providing treatment, doctors at the service ensured the policy was to ensure there was adequate knowledge of the patient’s health, any relevant test results and their medicines history. We saw examples of patients being signposted to more suitable sources of treatment where this information was not available to ensure safe care and treatment. However, the process relied on the patient providing that information with no further systems in place to verify this with the patients’ own GP.”
…
“The service identified patients who may need extra support and had a range of information available on the website (or links to NHS websites or blogs). For example, in consultation records, we found patients were given advice on healthy living as appropriate. However, we found that in some instances patients were not sent vital information with their medicines. For example, the information leaflets were missing vital information on safety netting such as depression/suicide risk associated with some medicines used to treat depression. Following our inspection, the provider wrote to us stating they had taken action to correct this.”
56. Under “Are services well-led?” it states:
“There was evidence of continued issuing of prescriptions for some patients with chronic conditions without assurance that these patients had received adequate monitoring from their own GPs. There were also instances where antibiotics had been prescribed despite a lack of sufficient history. The leaders were not aware of these gaps within their systems and had not undertaken a robust risk assessment to minimise risk for patients whose health required monitoring prior to receiving repeat medicines.”
57. This evidence was a major element in the conclusions that were reached. Those conclusions were reflected in the ratings to which I have referred. They led to the Notices being issued under Regulations 12 (Safety) and 17 (Good Governance). These notices require the provider to send to the CQC a report saying what action is going to be taken to meet the requirements.
58. In its Grounds of Defence, the CQC says:
“The CQC has to operate through taking a sample of cases, given the length of the inspection and the number of other registered providers. The inspection took place over one day and the records were not easy to access through the system. Whilst the sample was relatively small, a very worryingly high proportion of the records examined contained issues: six records were examined in full; and the inspectors had concerns in respect of five of them.
As set out above, the CQC was initially minded to issue a warning notice, but, following consideration of the Claimant’s representations, it declined to do so. This bears out the CQC’s balanced and proportionate approach, taking into account the risks presented. Given the CQC’s principal statutory objective to protect the health and welfare of its service-users and its findings in respect of safe prescribing, it is not arguable that the CQC breached s 4(1)(e) of the 2008 Act. ”
59. The provider’s position has consistently been that the size of the sample was so small that no reliable conclusions about anything could be drawn from it. I refer to the following statements by the provider:
i) In its FAC list:
“The judgement made cannot possibly be reflective or representative of the Provider as a whole because, at best, it is 0.01% of the records. No reasonable or rational regulator would draw such an overarching conclusion based on such a small sample.”
ii) In the witness statement of its clinical lead:
“One in ten NHS prescriptions are classified as a prescribing error. It has been estimated that that is nearly 237 million a year at a cost to the NHS of £98 million. We had one out of a possible 60,000 prescriptions from the medical record cohort selected by the inspection team: to rate the service as inadequate based on this one error is a grossly disproportionate response. If this were the case in all inspections then all Service Providers registered with the CQC would be classified as inadequate.”
iii) In its amended Statement of Facts and Grounds:
“As such, the Defendant’s approach cannot be characterised as proportionate, as the balancing exercise that the Defendant must conduct under s.4(1)(e) used just 6 cases to effectively impose a serious sanction against the Claimant.”
iv) In the skeleton argument of Mr Havers KC and Ms McCann:
“The Defendant acted disproportionately because it only selected nine records and only reviewed six records as a sample of cases. ….The Defendant’s case is that this approach to the records was reasonable firstly because it only had one day to inspect and did not have easy access through the system and secondly because “while the sample was relatively small, a very worryingly high proportion of the records examined contained issues” … It is submitted that both justifications further evidence the Defendant’s unfair, disproportionate approach. In the context of previous “Good” ratings in 2019, five out of six cases causing concern should have been seen as unrepresentative, warranting wider review and closer scrutiny as the Defendant acknowledged in its FAC response “…we are not saying that six records is representative of the quality of all records but may indicate whether there may be concerns or need to explore further” In fact, no further records have been reviewed and no further exploration was undertaken. Accordingly, none of the Defendant’s findings or actions can be characterised as proportionate to achieving its primary statutory objective when such an assessment was fundamentally limited and flawed.”
60. The gravamen of the CQC’s defence is that such a high proportion of worrying issues leads to the reasonable conclusion that there is, at the very least, a significant risk of a high rate of issues across the board, and that such a conclusion, among other reasons, justifies a finding that the safety standards are inadequate. I readily accept that this would be the instinctive response of a lay person on learning that 5 out of 6 randomly selected records revealed worrying issues. Such an instinctive reaction is demonstrated by the CQC’s response to the FAC list:
“Our records review is a sample size, we are not saying that six records is representative of the quality of all records but may indicate whether there may be concerns or a need to explore further. The report is factually correct in that the six records reviewed had concerns in relation to them and improvements are required to be made. The evidence collected during our inspection process supports the statement in the report you refer to. Therefore, no changes will be made to the final report in relation to your comments in this section.”
61. In her witness statement the lead inspector stated to similar effect:
“At paragraph 41 of the ASFG, the Claimant suggests that the sample size of records was insufficient. However, even though relatively small sample was taken, we still found problems with over 50% of those records which is a high proportion. It is not unusual on inspection for us not to move on to further records where the initial set of records show this level of concerns.”
62. The approach of the CQC gives rise to a number of questions. Are such responses entirely consistent with the laws of probability? Would a sample size of 6 out of 60,000 be regarded as statistically significant? In using such a small sample did the CQC conduct a fair analysis? If not, has that principle been sacrificed on the altar of CQC’s limited resources?
63. It seems to me that the key question is this: whether adopting a common-sense point of view or a legal point of view, can a generalised criticism that the provider’s standard of safety is “inadequate”, or that its standards of effectiveness and leadership “require improvement”, logically and fairly be extrapolated from six medical records out of 60,000?
64. I do not doubt that there would be resource implications if the CQC’s inspection teams had to review hundreds of medical records on every inspection such as this. The answer to the questions might be, therefore, that given the resources available to the CQC, and the duty imposed on it to protect the public, there is no other way of forming an evidence base from which to extrapolate conclusions, notwithstanding that the result of the ratings and of the report could have very serious implications for the provider. Further, for all I know, it may be commonly accepted that where, as here, a regulator is concerned with safety, a statistical approach is not appropriate. I read no evidence and heard no argument about the accepted alternative modes of proof used by such regulators when identifying systemic issues of concern.
66. I will give permission to both parties to adduce expert statistical evidence at the substantive hearing and to the CQC to adduce evidence as to the resource implications of having to use significantly larger samples on inspections or assessments.
Ground 3
67. I have already dealt with this issue at [22] - [33] above. I am not satisfied that the procedure adopted by the CQC was unfair, or in conflict with the judgment of Andrews J. If it was in conflict with the judgment of Andrews J then I respectfully disagree with her. As framed, Ground 3 is unarguable
Ground 4
68. So far as the report makes criticisms, applies ratings, and stipulates requirements, it is written largely in the present tense suggesting that immediate remediation needs to be taken now. That is how I read it initially. However, on very careful repeated further readings, and with the assistance of Mr Stilitz KC, I now realise that the report asks the reader to travel back in time to 17 May 2022 and to be educated about the inadequacies of the provider at that time. The problem with this journey back in time is that it is not a consistent one because there are some references to subsequent events in the report. For example, under “Are services safe?” it is stated:
“During the factual accuracy period, the provider told us that following our inspection feedback they had on 18 May 2022 ceased the prescribing of ramipril, lisinopril and angiotensin-converting enzyme (ACE) inhibitors that require renal and kidney blood tests and Terbinafine which requires a liver blood test.”
…
“Following our inspection, the provider wrote to us stating they would review the process of antibiotics prescribing to ensure it includes the necessary details prior to prescribing.”
69. I have found the language of the report jumping between different time zones, less than completely clear. I think that there is some force in the criticism that the finding of inadequate safety standards does not appear to pay much regard to the remediation steps taken by the provider since the inspection.
70. Inasmuch as the verdict of inadequate safety was based on the very limited sample then I consider this ground to be arguable although it does not need to attract separate permission as it is covered by the permission already granted under Ground 2. I do not consider that the linguistic confusion to which I have referred justifies any additional grant of permission under this ground, now that I understand that the finding of inadequate safety standards strictly refers to the position as at 20 May 2022 and not to any later date. However, I think that the various rubrics in the form ought to make it clear that all of the findings, recommendations and requirements relate to the position as at the date of inspection. Further, all comments relating to subsequent events ought be put in a separate section with a heading such as “events after the inspection”.
71. I therefore do not grant permission under Ground 4.
Ground 5
72. To the extent that it is said that ill-founded and erroneous conclusions were drawn from a statistically insignificant sample, this complaint is covered by Ground 2 and requires no separate permission here. Otherwise, factual errors are dealt with by the FAC process, and are essentially immune from further challenge absent proof of error of law or abuse of power. The provider’s case does not come close to showing prima facie that the findings are so blatantly wrong that it can be inferred that the CQC’s inspection team has taken leave of its collective senses or that the findings were the product of an abuse of power or bad faith.
73. I therefore do not grant permission under Ground 5.
Injunction
74. Interim relief in a case such as this is not governed exclusively by the balance of harm test in American Cyanamid v Ethicon [1975] AC 396. Where an injunction is sought to prevent a public body from publishing a report it is under a statutory duty to publish, the test is much more stringent. The principles were set out by Burton J in R (City College Birmingham) v Ofsted [2009] EWHC 2373 (Admin). He stated:
“25. There is a clear and identifiable line of authority in relation to the grant of injunctions to restrain public bodies from publishing decisions or reports, which makes it clear that there are separate public law questions which fall to be considered alongside the ordinary principles of private law injunctions. So far as private law injunctions are concerned, the ordinary test, by reference to American Cyanamid, is whether there is an arguable case for the claimant, and if so, where the balance of convenience lies. In defamation cases, injunctions will rarely be given because of the obligations of freedom of speech, but certainly so where the defendant asserts that he or she intends to justify the truth of what it asserts. However, in the public law field there are additional considerations, as is clear from the authorities which have been put before me.
…
28. In the Debt Free Direct Ltd decision, Sullivan J said … in paragraph 24, that there would have, in his judgment, to be "the most compelling reasons to prohibit a public body which is embarked on a quasi-judicial task … from publishing its decision".
29. It is not simply, therefore, that there are all these additional words: "exceptional circumstances", "most compelling reasons", "pressing grounds", "exceptionally strong grounds", which require to be satisfied, but such that it will not be in every circumstance - far from it, that a good arguable case is entitled to be protected by an injunction.
30. Sullivan J gave examples of where there might be extreme circumstances - as he put it, in paragraph 24, "most compelling reasons to prohibit the public body": if for example the public body had engaged in a vendetta against the person the subject of the adjudication or if the adjudication was prompted by a deliberate desire to inflict damage on the reputation of the person criticised. One can think of other examples involving fraud or corruption, or perhaps involving the intention to proceed with a Report which is, and can be shown to be, as on a justification injunction, manifestly untrue or riddled with error. It is never helpful to come up with examples, except suffice it to say that the test of the judge's thermometer, in terms of response to an injunction, will be set and calibrated several degrees higher, so far as looking at the arguability of a case, than it is in this case.
31. Assuming, as I do for the purpose of the injunction, that there is an arguable case on the part of the claimant, and even filtering in the damage which the claimant says it will suffer, which is no different from, and perhaps less serious than, that suffered by the victims of other alleged statements which they seek to restrain, I am entirely satisfied that there are not, in this case "most compelling reasons", "exceptional circumstances", "pressing grounds", or "extreme circumstances", which justify the grant of an injunction.”
75. The principles have been followed in subsequent cases, including by Holgate J in the Babylon case, where he granted limited permission on one ground but refused the application for an injunction to prevent publication, stating at [87] that:
“…the case put forward by the Claimant comes nowhere near the threshold required to justify the continuation of the injunction to restrain the publication of the report as it now stands, in accordance with the Commission's statutory duty.”
76. So here. I cannot say that the facts of this case, even taken at their highest, come close to demonstrating the exceptionally strong grounds needed to prevent a public body from publishing a report that Parliament has required it to publish. However, the provider will no doubt be able to point to the terms of this judgment to demonstrate that the application to quash the report is going ahead, the court having found that there was an arguable case to take to trial.
Conclusion
77. Permission to apply for judicial review is granted under Ground 2. It is refused under Grounds 1, 3, 4 and 5.
78. The application for an injunction is refused.
79. I expect counsel to agree the necessary directions for the substantive hearing of Ground 2, to include expert and other evidence as referred to in [66] above. I will rule on any disputes on paper without a hearing. If the issue of costs cannot be agreed I will rule on it on paper without a hearing.
_________________________________
[1] As explained by Lord Neuberger PSC in Re B (a Child) [2013] UKSC 33, [2013] 1 WLR 1911 at [57] - [58]
