Freely Available British and Irish Public Legal Information
[Home] [Databases] [World Law] [Multidatabase Search] [Help] [Feedback]
England and Wales Family Court Decisions (other Judges)
You are here: BAILII >> Databases >> England and Wales Family Court Decisions (other Judges) >> CC, Re (Fact Finding: Head Injury) [2024] EWFC 317 (B) (04 November 2024)
URL: http://www.bailii.org/ew/cases/EWFC/OJ/2024/317.html
Cite as: [2024] EWFC 317 (B)
[New search] [Printable PDF version] [Help]
This judgment was delivered in private. The judge has given permission for this version of the judgment to be published on condition that (irrespective of what is contained in the judgment) in any published version of the judgment the anonymity of the children and members of their family must be strictly preserved. All persons, including representatives of the media and legal bloggers, must ensure that this condition is strictly complied with. Failure to do so may be a contempt of court.
Neutral Citation Number: [2024] EWFC 317 (B)
Case Number: RG24C50047
IN THE FAMILY COURT AT SLOUGH
The Law Courts
Windsor Road
Slough
SL1 2HE
Date: 4 November 2024
Before
HIS HONOUR JUDGE RICHARD CASE
- - - - - - - - - - - - - - - - - - - - -
Re CC (Fact Finding: Head Injury)
Between
ROYAL BOROUGH OF WINDSOR AND MAIDENHEAD
Applicant
and
MOTHER (1)
FATHER OF CA AND CB (2)
FATHER OF CC (3)
CA, CB AND CC, THE CHILDREN (4-6)
Respondents
- - - - - - - - - - - - - - - - - - - - -
- - - - - - - - - - - - - - - - - - - - -
Representation
For the Applicant:
Elizabeth Isaacs KC and Lucinda Wicks, counsel instructed by the Applicant Council
For the Respondents:
Penny Howe KC and Jayne Harrill, counsel instructed by the First Respondent Mother
Second Respondent Father excused attendance
Nick Goodwin KC and Elizabeth Wickham, counsel instructed by the Third Respondent Father
Roma Whelan, counsel instructed by the Fourth to Fifth Respondent children by their Children’s Guardian, Nandi Sutherland
Hearing dates: 14-15, 17, 21-24 October 2024
- - - - - - - - - - - - - - - - - - - - -
APPROVED JUDGMENT
This judgment was handed down remotely at 10am on 4 November 2024 by circulation to the parties’ representatives by email.
Contents
Disputed or not agreed facts. 25
Group 1: Subdural collections. 34
Group 3: Skull fracture dating. 36
Group 4: Subdural collections dating. 39
Group 5: Skull fracture mechanism.. 43
Group 6: Subdural collections mechanism.. 45
General Observations CA and CB. 54
Summary
1. CC suffered multi-compartmental bilateral subdural collections containing haemorrhage surrounding the brain.
2. The likely date of this intracranial injury was between 16 February 2024 and 1 March 2024.
3. CC suffered 2 fractures to the right parietal bone.
4. The likely date of the fractures was between 26 January 2024 and 27 February 2024.
5. The injuries were sustained whilst in the care of FC on 27 February 2024. There was either a single impact with greater force than would be occasioned by an accidental fall from a carer’s arms or 2 separate incidents of shaking and impact. On the evidence I cannot say one is more likely than the other. If it were a single impact that was a deliberate act, it required greater force than an accidental drop from a carer’s arms. If it were a combination of shaking and an impact the impact may have been accidental (such as by dropping CC) but the shaking could not have been, it was deliberate.
6. FC has inflicted significant harm on CC: through physical injury and emotionally through persisting in denying responsibility for his actions which has led to CC’s separation from M. And all this when his ultimate position was that he admitted causing the physical injuries through culpable accident albeit I have gone further to find he inflicted them. FC has engaged in a deliberate and cynical attempt to conceal the true facts and has, at almost every turn, sought to evade and minimise his responsibility.
7. The section 31(2) Children Act 1989 is crossed on these findings.
Parties
8. I am concerned with 3 children. For anonymity I will refer to them as CA (aged early teens), CB (pre-teenager) and CC (infant). For the purposes of this fact finding hearing I am principally concerned with CC. Similarly, for anonymity I will refer to the Mother of all three children as M, the Father of CA and CB as FA and the Father of CC as FC; I mean no discourtesy to the parents. I excused FA’s attendance at this fact finding hearing as it concerns injuries sustained by CC in the care of M and FC.
Background
Chronology
9. CC was born in November 2023. He was admitted to Hospital A on 8 March 2024 and found to be suffering multiple injuries. These are summarised in the Local Authority case summary:
The clinical evidence
24. On presentation to hospital CC was found to have a bulging anterior fontanelle with prominent scalp veins E135. His head circumference was noted to have increased to between the 75th and 98th centiles E119, having formerly been noted to be at the 25th centile at birth E119 and at the 50th centile at his 8-week developmental check… K24.
25. A CT scan was carried out on 8 March 2024 at Hospital A. Later that day CC was transferred to Hospital B and further scans were carried out as follows -
• 9 March 2024 - MRI brain and spine scan
• 11 March 2024 - skeletal survey (Part 1)
• 20 March 2024 - CT head scan
• 26 March 2024 - cranial ultrasound scan
• 27 March 2024 - skeletal survey (Part 2)
• 27 March 2024 - CT head scan
• 8 April 2024 - CT head scan
• 15 April 2024 - CT head scan
26. The imaging confirmed that CC had sustained the following injuries -
• Multi-compartmental bilateral subdural collections containing haemorrhage surrounding the brain E167, E121; and
• Two lucencies (linear discontinuities in bone) of the R parietal bone of the skull with no associated scalp swelling E132
27. There was no underlying medical cause identified for these injuries, there was no history of any accidental injury provided by either M or FC, and these injuries were not considered by treating clinicians to have been caused by accidental injury.
10. Mr Jalloh, paediatric neurosurgeon, has summarised the medical chronology in this way [E112]:
3.1 CC was born on [] November 2023 via emergency caesarean section at 38 weeks’ gestation. Apgar scores were 10 at 1 minute after birth indicating that he was born in good condition. Head circumference measured 34 cm at birth. He was discharged home…
…
3.3 On 08 December 2023, CC was seen by the Health Visitor in a routine home visit. No concerns were noted.
3.4 On 03 January 2024, CC was seen by the GP with both parents because of a rash on his lower abdomen. Advice and guidance were given.
3.5 On 18 January 2024, CC was seen for a routine review by the Health Visitor where no concerns were raised.
3.6 On 23 January 2024, CC was seen for his routine…check at the GP. There were no concerns on examination. Head circumference measured 39 cm.
3.7 On 05 February 2024, CC was seen by the GP and diagnosed with a viral upper respiratory tract infection after presenting with a cough, an episode of vomiting after coughing, and being more sleepy than usual.
3.8 CC received routine immunisations on 23 January and 20 February 2024.
3.9 On 29 February 2024, CC’s dad called NHS 111 with concerns about diarrhoea for 2 days and vomiting that day.
3.10 On 01 March 2024, CC was taken by his mum to the GP with a 4-day history of vomiting, refusing food, and loose stools. On examination, the anterior fontanelle was described as ‘normotensive’. The anterior fontanelle is the gap between skull bones used to assess intracranial pressure.
3.11 Later that day on 01 March 2024, CC was brought to A&E at Hospital A by his mother with a similar history of vomiting. The Paediatric Assessment Unit (PAU) clerking by the paediatric junior doctor noted a 2-day history vomiting which started after he received Calpol for teething. Additionally, a history of loose stool and being a bit sleepier was recorded. CC was able to take 5 oz of feed without vomiting whilst observed in PAU. On examination a normal fontanelle was noted. A viral infection was suspected and advice given. Senior review by the paediatric registrar also noted a soft anterior fontanelle and agreed with the diagnosis of a likely viral illness.
3.12 On 04 March 2024, CC was taken by his mum to the GP with persistent vomiting. The GP recorded a history of lethargy and reduced feeding. The GP made a referral to paediatrics. CC was seen later that day in PAU where he was observed, noted to be passing urine well and tolerating feeds. The suspected diagnosis of an upper respiratory tract infection was given, and he was discharged.
…
3.14 CC was brought back to PAU on 08 March 2024 with persistent vomiting after being reviewed by the GP. The PAU clerking by the junior doctor noted vomiting after feeds 5 or 6 times per day, and that he had not been himself described as irritable and sleepy. CC’s mum had also noted a blotchy red dry skin on his forehead that had resolved. On examination he was noted to be alert and settled. His fontanelle was noted to feel full (suggestive of raised intracranial pressure). Head circumference measured 42 cm. This was noted to be on the 98th centile representing an increase from the 25th centile at birth and the 50th centile during the…baby check. Senior review by the paediatric registrar…noted a similar history of vomiting for 10 days and that he was otherwise well in himself. He was described as looking macrocephalic (having an enlarged head).
3.15 A CT scan was performed on 08 March 2024 and reported as showing fractures of the right parietal bone and small volume hyperdense haemorrhage overlying the frontal lobe. This was discussed with the regional neurosurgery team in Hospital B who advised urgent transfer for specialist care.
3.16 C was transferred to Hospital B on 09 March 2024 [in fact it was late on 8 March 2024 - see Dr Cartlidge [E181]]. Initial paediatric assessment noted a history from mum that CC had head-butted dad a few days ago, after he had already started vomiting, and that there was no other history of trauma. Mum noted that CC was sleepier than normal.
3.17 CC was assessed by the Paediatric Registrar…who on examination found that CC was sleepy but rousable, had dilated scalp veins and a bulging, pulsatile, and tense anterior fontanelle. Head circumference measured 43 cm. He was described as having good head control but unable to fix and follow with his eyes. No other abnormal findings were noted on examination and there were no external signs of injury.
3.18 Soon after arriving, he underwent a trans-fontanelle tap of the subdural collection, which is a procedure performed at the bedside where a needle is inserted via the gap between skull bones to drain the subdural collection. 21 ml of blood-stained cerebrospinal fluid (CSF) was drained. This was tested for infection and no evidence of infection was found.
3.19 During the review by the Paediatric Neurosurgery Team on 09 March ...further history was obtained from mum including that CC had been vomiting since mum was admitted to Hospital A for treatment of a chest infection on 27 to 28 February. Prior to this he was not
vomiting, was feeding well, and not distressed. Mum denied that there have been any problems with CC’s eyes such as a squint or difficulty looking up, nor problems with moving his limbs. She reported that the scalp veins were prominent but was not sure when that started.
3.20 MRI on 09 March 2024 was reported as showing large bilateral subdural fluid collections with evidence of haemorrhage, shallow right-sided posterior fossa subdural collection, and no evidence of injury to the brain substance. The spine MRI was reported as normal.
3.21 Ophthalmology review on 09 March 2024 found a normal examination with no evidence of retinal haemorrhages or disc swelling.
3.22 On 10 March 2024, CC was described as much brighter and to be feeding well although he still continued to vomit.
3.23 Head circumference measured 43.6 cm on 12 March 2024.
3.24 CC was reviewed by Consultant Neurosurgeon…on 12 March 2024 who noted that CC had responded to a single fontanelle tap and that although his fontanelle remained full, he was not showing clinical signs of raised intracranial pressure. He provided an opinion on the presenting CT scan describing lucencies in the parietal bone that might be fractures or possibly accessory sutures.
3.25 CC was repatriated from Hospital B to Hospital A on 13 March 2024. He remained well during the rest of his inpatient stay and was discharged into foster care on 19 March.
3.26 CC’s mum disclosed to the medical team on 16 March 2024 about an incident when dad was looking after CC, picked him up, moved to the bedroom and then his two siblings heard a loud bang coming from the room and dad was shouting.
3.27 CC was readmitted to Hospital B on 20 March 2024 due to an increased head circumference. On initial assessment by the Neurosurgical Registrar his fontanelle was described as full but not as tense as before. He was noted to have been feeding with small vomits that day but otherwise happy and interactive. Head circumference measured 44.5 cm.
3.28 CT head on 20 March 2024 was reported as showing a marginal increase in the bilateral subdural collections. The previously seen acute haemorrhage had resolved.
The ventricles were also noted to be slightly larger likely reflecting reduced pressure from the drained subdural collections.
3.29 Head circumference measured 44.9 cm on 21 March 2024. His fontanelle was described as full and tense. Consultant Neurosurgeon…performed a trans-fontanelle tap on 21 March with 29 ml of fluid aspirated and described as 'frankly red fluid obtained, under pressure. The fluid was neither clear/xanthochromia nor dark/motor oil appearing. It was "Venetian" red'.
3.30 Clinical examination by the Neurosurgery Team on 22 March 2024 found a full fontanelle and concluded that the subdural collections were refilling and therefore decided to insert a surgical drain. This was performed in the operating theatres through a right frontal incision. A drain was inserted into the subdural space and tunnelled out through the skin to drain fluid into a collection bag.
3.31 A cranial ultrasound on 26 March 2024 showed similar sized subdural collections as seen previously on the CT.
3.32 On 30 March 2024 the subdural drain was noted to be blocked with fresh blood. CT showed a reduction in the size of the subdural collections with some fresh blood related to the drain insertion.
3.33 Over the next few days, CC’s head circumference remained stable and he remained clinically well. Intermittent leak from the drain exit site on the head was noted from 04 April 2024. This is a frequent complication of these types of drains.
3.34 CT head on 08 April 2024 was reported as showing a reduced volume of subdural fluid with the drain inserted.
3.35 The drain was removed in theatre under anaesthesia on 08 April 2024.
3.36 CT head on 15 April 2024 showed an increase in the size of the subdural collections. This was discussed with the neurosurgery consultant who considered that further intervention might be required but was content to observe in the first instance.
3.37 Over the next few days, CC remained well with no concerns noted from nursing
staff and with a soft fontanelle.
3.38 He was discharged on 19 April 2024. Head circumference prior to discharge on 18 April was 44.8 cm.
Current living arrangement
11. CA and CB remain in the care of M pursuant to Interim Supervision Orders. CC is in foster care pursuant to an Interim Care Order.
Parental Responsibility
12. M and FA share parental responsibility for CA and CB.
13. M and FC share parental responsibility with the Local Authority in respect of CC.
Positions
Local Authority
14. The Local Authority seek findings as set out below but in summary allege that skull fractures and intracranial injuries were caused by FC on or about 27 February 2024. They do not invite me to make a finding whether that was through an accident whilst under the influence of alcohol or drugs or the deliberate infliction of injury.
Mother
15. The Mother denies causing injuries. She invites the court to find the injuries were inflicted by FC on 27 February 2024.
Father FC
16. At the conclusion of the evidence FC revised his position. He now seeks a finding that CC’s injuries were caused in a single application of force in a single incident of injury, that M did not cause them and nor did CA or CB, and he “accepts that CC must have been injured as a result of an accident when in his sole care on 27 February 2024, but he has no memory, through drink and possibly through drugs, of any such event” and that CC’s injuries are consistent with a fall from the arms of a carer. He accepts that threshold is met.
Children’s Guardian
17. The Guardian considers that after all the evidence the court may conclude CC’s injuries occurred in FC’s care on 27 February 2024.
Evidence Summary
18. I have considered the following documents in particular:
a) M response to threshold [A1] and response to Schedule of allegations [Z32];
b) FC response to threshold [A4] and response to Schedule of allegations [Z53];
c) Schedule of allegations [A68] and Amended Schedule;
d) Paediatric haematology report of Dr Keenan dated 28 May 2024 [E53] and addendum after further testing [Z57];
e) Paediatric neurosurgical report of Mr Jalloh dated 18 June 2024 [E108] and addendum dated 10 October 2024 [Z12];
f) Paediatric neuroradiology report of Dr Oates dated 1 July 2024 [E132] and informal addendum reported in the Local Authority case summary;
g) Paediatric report of Dr Cartlidge dated 14 August 2024 [E171] and addendum dated 9 October 2024 [Z1];
h) Report of Dr Cummings, treating paediatrician [F41];
i) Witness statement of Jo McDonnell, health visitor [C45];
j) Transcript of Police interview of M [O24];
k) Transcript of Police interview of FC [O1] and [O66];
l) Transcript of Police Achieving Best Evidence (ABE) video recorded interview (VRI) of CA [U1] and the video recording [O548];
m) ABE VRI of CB [O526];
n) Police log [O407-O458];
o) Drugs test of FC 16 April 2024 [E1] and 23 September 2024 [E245];
p) 111 call transcripts [Section S] and the recording of the first call on 29 February 2024 [P1];
q) Body worn video (BWV) footage of 8 March 2024 [O515-O519];
r) Phone records (variously in section Z, I will not use the pagination as it relies on M and FC’s initials);
s) Witness statements of M [C66] and [C109]; and
t) Witness statement of FC [C75] and [Z53].
19. I heard oral evidence from Dr Oates, Mr Jalloh, Dr Cartlidge, M and FC.
Law
Threshold
20. I must consider if the Local Authority has proved that the threshold test set out in section 31(2) Children Act 1989 is met. It provides:
(2) A court may only make a care order or supervision order if it is satisfied –
(a) that the child concerned is suffering, or is likely to suffer, significant harm; and
(b) that the harm, or likelihood of harm, is attributable to –
(i) the care given to the child, or likely to be given to him if the order were not made, not being what it would be reasonable to expect a parent to give to him; or
(ii) the child’s being beyond parental control.
21. I remind myself that the relevant date for the purposes of making the assessment is the date on which the Local Authority initiated the procedure ( Re M (Care Order: Threshold Conditions) [1994] 2 FLR 577) but subsequent events and behaviour are capable of providing relevant evidence about the position before the relevant date ( Re L (Care: Threshold Criteria) [2007] 1 FLR 2050).
Fact Finding
22. I remind myself of the fact-finding self-directions that I must give myself adapted from the helpful summary of Munby P in Re X (Children) (No 3) [2015] EWHC 3651:
20. …The principles are conveniently set out in the judgment of Baker J in Re L and M (Children) [2013] EWHC 1569 (Fam), to which I was taken. So far as material for present purposes what Baker J said (and I respectfully agree) was this:
“First, the burden of proof lies at all times with the local authority.
Secondly, the standard of proof is the balance of probabilities.
Third, findings of fact in these cases must be based on evidence, including inferences that can properly be drawn from the evidence and not on suspicion or speculation …
Fourthly, when considering cases of suspected child abuse the court must take into account all the evidence and furthermore consider each piece of evidence in the context of all the other evidence. The court invariably surveys a wide canvas. A judge in these difficult cases must have regard to the relevance of each piece of evidence to other evidence and to exercise an overview of the totality of the evidence in order to come to the conclusion whether the case put forward by the local authority has been made out to the appropriate standard of proof.
Fifthly, … Whilst appropriate attention must be paid to the opinion of … experts, those opinions need to be considered in the context of all the other evidence. It is important to remember that the roles of the court and the expert are distinct and it is the court that is in the position to weigh up the expert evidence against its findings on the other evidence. It is the judge who makes the final decision.
Sixth, … The court must be careful to ensure that each expert keeps within the bounds of their own expertise and defers, where appropriate, to the expertise of others.
Seventh, the evidence of the parents and any other carers is of the utmost importance. It is essential that the court forms a clear assessment of their credibility and reliability.
Eighth, it is common for witnesses in these cases to tell lies in the course of the investigation and the hearing. The court must be careful to bear in mind that a witness may lie for many reasons, such as shame, misplaced loyalty, panic, fear and distress, and the fact that a witness has lied about some matters does not mean that he or she has lied about everything (see R v Lucas [1981] QB 720 ).” [I address this further below]
23. Munby P continued:
21. To this admirable summary I add three further points.
22. First, that the legal concept of proof on a balance of probabilities “must be applied with common sense”, as Lord Brandon of Oakbrook said in The Popi M, Rhesa Shipping Co SA v Edmunds , Rhesa Shipping Co SA v Fenton Insurance Co Ltd [1985] 1 WLR 948, 956.
23. Secondly, that the court can have regard to the inherent probabilities: see Lady Hale in In re B (Children) (Care Proceedings: Standard of Proof) (CAFCASS intervening) [2008] UKHL 35, [2009] 1 AC 11, para 31. But this does not affect the legal standard of proof, as Lord Hoffmann emphasised in the same case (para 15):
“There is only one rule of law, namely that the occurrence of the fact in issue must be proved to have been more probable than not. Common sense, not law, requires that in deciding this question, regard should be had, to whatever extent appropriate, to inherent probabilities. If a child alleges sexual abuse by a parent, it is common sense to start with the assumption that most parents do not abuse their children. But this assumption may be swiftly dispelled by other compelling evidence of the relationship between parent and child or parent and other children. It would be absurd to suggest that the tribunal must in all cases assume that serious conduct is unlikely to have occurred. In many cases, the other evidence will show that it was all too likely.”
24. Thirdly, that the fact, if fact it be, that the respondent … fails to prove on a balance of probabilities an affirmative case that she has chosen to set up by way of defence, does not of itself establish the local authority’s case. As His Honour Judge Clifford Bellamy recently said in Re FM (A Child: fractures: bone density) [2015] EWFC B26, para 122, and I respectfully agree:
“It is the local authority that seeks a finding that FM’s injuries are non-accidental. It is for the local authority to prove its case. It is not for the mother to disprove it. In particular it is not for the mother to disprove it by proving how the injuries were in fact sustained. Neither is it for the court to determine how the injuries were sustained. The court’s task is to determine whether the local authority has proved its case on the balance of probability. Where, as here, there is a degree of medical uncertainty and credible evidence of a possible alternative explanation to that contended for by the local authority, the question for the court is not ‘has that possible alternative explanation been proved’ but rather it should ask itself, ‘in the light of that possible alternative explanation can the court be satisfied that the local authority has proved its case on the simple balance of probability’.”
24. In relation to experts in Re B (Care: Expert) [1996] 1 FLR 667 at 674 Butler-Sloss LJ said:
I agree with the judgment of Ward LJ. Family judges deal with increasingly difficult child cases and are much assisted in their decision-making process by professionals from other disciplines: medical, wider mental health and social work among others. The courts pay particular attention to the valuable contribution from paediatricians and child psychiatrists as well as others, but it is important to remember that the decision is that of the judge and not of the professional expert. Judges are well accustomed to assessing the conflicting evidence of experts. As Ward LJ said, judges are not expected to suspend judicial belief simply because the evidence is given by an expert. An expert is not in any special position and there is no presumption or belief in a doctor however distinguished he or she may be. It is, however, necessary for a judge to give reasons for disagreeing with experts' conclusions or recommendations. That, this judge did. A judge cannot substitute his views for the views of the experts without some evidence to support what it is he concludes.
25. In his President’s Memorandum on Witness Statements dated 10 November 2021 McFarlane P said:
14. Parties should understand that the court’s approach to witness evidence based on human memory will be in accordance with CPR PD 57AC, Appendix para 1.3.
This states that human memory:
a. is not a simple mental record of a witnessed event that is fixed at the time of the experience and fades over time, but
b. is a fluid and malleable state of perception concerning an individual’s past experiences, and therefore
c. is vulnerable to being altered by a range of influences, such that the individual may or may not be conscious of the alteration.
26. I also direct myself to the judgment of Peter Jackson J (as he was) in Lancashire County Council v The Children [2014] EWHC 3 (Fam):
9. To these matters I would only add that in cases where repeated accounts are given of events surrounding injury and death the court must think carefully about the significance or otherwise of any reported discrepancies. They may arise for a number of reasons. One possibility is of course that they are lies designed to hide culpability. Another is that they are lies told for other reasons. Further possibilities include faulty recollection or confusion at times of stress or when the importance of accuracy is not fully appreciated, or there may be inaccuracy or mistake in the record keeping or recollection of the person hearing and relaying the account. The possible effects of delay and questioning upon memory should also be considered, as should the effect on one person of hearing accounts given by others. As memory fades, a desire to iron out wrinkles may not be unnatural - a process which might inelegantly be described as “story creep” - may occur without any inference of bad faith.
27. That should be borne in mind when considering perceived differences between accounts over time and generally when considering a witness’ recall.
28. As to propensity to cause harm to children I refer myself to Ryder J (as he then was) in Lancashire County Council v R [2010] 1 FLR 387:
59. Such evidence may demonstrate that each parent has been or is capable of being physically aggressive or emotionally abusive to the other. The potential for harm to a child in such circumstances is self evident but in order to ensure that it is considered in every case, Parliament has enacted an amendment to the 1989 Act to provide for the same: by s 31(9) as introduced by s 120 Adoption and Children Act 2002 harm explicitly includes impairment suffered from seeing or hearing the ill-treatment of another: in colloquial terms, domestic abuse.
60. However, despite the above, what such incidents do not of themselves demonstrate, is that either parent has the propensity to violence towards small children. A clear distinction is to be drawn between the relevance and admissibility of evidence which describes the harmful circumstances in which a child is being cared for and the same evidence when it is used to suggest that a person has a propensity to commit a particular act. In other words, the evidence will be very relevant to harm or its likelihood in s 31(2) and the court’s assessment of risk in s 1(3)(e) of the 1989 Act but not necessarily to perpetration. It may be forensically unwise for the court to attach much, if any, weight to this evidence if it is directed only to the question of propensity…
29. As regards demeanour I have regard to Peter Jackson LJ in B-M (Children: Findings of Fact) [2021] EWCA Civ 1371:
25. No judge would consider it proper to reach a conclusion about a witness’s credibility based solely on the way that he or she gives evidence, at least in any normal circumstances. The ordinary process of reasoning will draw the judge to consider a number of other matters, such as the consistency of the account with known facts, with previous accounts given by the witness, with other evidence, and with the overall probabilities. However, in a case where the facts are not likely to be primarily found in contemporaneous documents the assessment of credibility can quite properly include the impression made upon the court by the witness, with due allowance being made for the pressures that may arise from the process of giving evidence. Indeed in family cases, where the question is not only ‘what happened in the past?’ but also ‘what may happen in the future?’, a witness’s demeanour may offer important information to the court about what sort of a person the witness truly is, and consequently whether an account of past events or future intentions is likely to be reliable.
26. I therefore respectfully agree with what Macur LJ said in Re M (Children) at [12], with emphasis on the word ‘solely’:
“It is obviously a counsel of perfection but seems to me advisable that any judge appraising witnesses in the emotionally charged atmosphere of a contested family dispute should warn themselves to guard against an assessment solely by virtue of their behaviour in the witness box and to expressly indicate that they have done so.”
…
28…There will be cases where the manner in which evidence is given about such personal matters will properly assume prominence. As Munby LJ said in Re A (A Child) (No. 2) [2011] EWCA Civ 12 said at [104] in a passage described by the Judge as of considerable assistance in the present case:
“Any judge who has had to conduct a fact-finding hearing such as this is likely to have had experience of a witness - as here a woman deposing to serious domestic violence and grave sexual abuse - whose evidence, although shot through with unreliability as to details, with gross exaggeration and even with lies, is nonetheless compelling and convincing as to the central core… Yet through all the lies, as experience teaches, one may nonetheless be left with a powerful conviction that on the essentials the witness is telling the truth, perhaps because of the way in which she gives her evidence, perhaps because of a number of small points which, although trivial in themselves, nonetheless suddenly illuminate the underlying realities.”
29. Still further, demeanour is likely to be of real importance when the court is assessing the recorded interviews or live evidence of children. Here, it is not only entitled but expected to consider the child’s demeanour as part of the process of assessing credibility, and the accumulated experience of listening to children’s accounts sensitises the decision-maker to the many indicators of sound and unsound allegations.
30. In relation to electronic messages I remind myself of the observations in Stocker v Stocker [2019] UKSC 17 in which Lord Kerr cautioned against “elaborate analysis of a tweet; it is likewise unwise to parse a Facebook posting for its theoretically or logically deducible meaning. The imperative is to ascertain how a typical (i.e. an ordinary reasonable) reader would interpret the message. That search should reflect the circumstance that this is a casual medium; it is in the nature of conversation rather than carefully chosen expression; and that it is pre-eminently one in which the reader reads and passes on”.
Lying
31. I remind myself of the Lucas direction from R v Lucas [1981] QB 720, elaborated on by Macur LJ in Re A [2021] EWCA Civ 451:
54. That a witness’s dishonesty may be irrelevant in determining an issue of fact is commonly acknowledged in judgments…in formulaic terms:
“that people lie for all sorts of reasons, including shame, humiliation, misplaced loyalty, panic, fear, distress, confusion and emotional pressure and the fact that somebody lies about one thing does not mean it actually did or did not happen and/or that they have lied about everything”.
But this formulation leaves open the question: how and when is a witness’s lack of credibility to be factored into the equation of determining an issue of fact? In my view, the answer is provided by the terms of the entire ‘Lucas’ direction as given, when necessary, in criminal trials.
55. Chapter 16-3, paragraphs 1 and 2 of the December 2020 Crown Court Compendium, provides a useful legal summary:
“1. A defendant’s lie, whether made before the trial or in the course of evidence or both, may be probative of guilt. A lie is only capable of supporting other evidence against D if the jury are sure that:
(1) it is shown, by other evidence in the case, to be a deliberate untruth; i.e. it did not arise from confusion or mistake;
(2) it relates to a significant issue;
(3) it was not told for a reason advanced by or on behalf of D, or for some other reason arising from the evidence, which does not point to D’s guilt.
2. The direction should be tailored to the circumstances of the case, but the jury must be directed that only if they are sure that these criteria are satisfied can D’s lie be used as some support for the prosecution case, but that the lie itself cannot prove guilt. …”
32. What I have said above in relation to memory applies to a consideration of whether a person is, in fact, lying; that is to say, whether they are dishonestly not telling the truth.
Injuries
33. Peter Jackson LJ summarised the questions to be answered in Re S (A Child: Adequacy of Reasoning) [2019] EWCA Civ 1845 at paragraph 3:
(1) Had the local authority proved that the injuries were inflicted as opposed to being accidental?
(2) If the injuries were inflicted, who had the opportunity to cause them?
(3) Of those people, could one person be identified on the balance of probabilities as having inflicted the injuries (a conventional 'known perpetrator' finding)?
(4) If only two people…could have caused the injuries, but the one responsible could not be identified it necessarily followed that there was a real possibility that each of them may have caused the injuries (an 'uncertain perpetrator' finding).
List of perpetrators
34. The following summary of the law is taken from the Family Court Practice paragraph 2.312[20]:
Uncertain perpetrator cases—If the judge cannot identify a perpetrator or perpetrators, it is still important to identify the possible perpetrators by asking whether the evidence establishes that there is a ‘likelihood or real possibility’ that a given person perpetrated the injuries in question (Re S-B (Children) [2010] 1 FLR 1161, SC; North Yorkshire CC v SA [2003] 2 FLR 849, CA). In such circumstances, it is all the more important to scrutinise the evidence carefully and consider whether anyone, and if so who, should be included as a possible perpetrator (Re S (A Child) [2014] 1 FLR 739, CA). However, it is not helpful for the judge to give an indication of percentages as to the likelihood that one or other of the possible perpetrators was responsible and judges should be cautious about amplifying in this way a judgment in which they have been unable to identify a specific perpetrator (Re S-B (Children) [2010] 1 FLR 1161, SC).
In A (Children) (Pool of Perpetrators) [2022] EWCA Civ 1348 the Court of Appeal reiterated that the evaluation of the facts which will enable a court to identify the perpetrator of an inflicted injury to a child will be determined on the simple balance of probabilities and nothing more. In this context, the Court of Appeal stated that judges should no longer direct themselves not to ‘strain’ to identify the perpetrator as the unvarnished test is clear: following a consideration of all the available evidence and applying the simple balance of probabilities, a judge either can, or cannot, identify a perpetrator. If he or she cannot do so, then, in accordance with Re B he or she should consider whether there is a real possibility that each individual on the list inflicted the injury in question.
In Re B (A Child) [2018] EWCA Civ 2127, and Re B (Children: Uncertain Perpetrator) [2019] EWCA Civ 575, the Court of Appeal gave further consideration to so called ‘uncertain perpetrator’ cases. In Re B (Children: Uncertain Perpetrator), the Court of Appeal urged a change of terminology from ‘pool’ to ‘list’. The following principles can be drawn from the two authorities:
(a) The concept of a ‘pool’ of perpetrators is one that seeks to strike a fair balance between the rights of the individual, including those of the child, and the imperatives of child protection;
(b) A decision by a court to place a person in a ‘pool’ of possible perpetrators does not constitute a finding of fact in the conventional sense in that that person is not proven to be a perpetrator but is rather a possible perpetrator;
(c) Where there are a number of people who might have caused the harm to the child, it is for the local authority to show that in relation to each of them there is a real possibility that they did so;
(d) Within this context, the question is whether it has been demonstrated to the requisite standard that a person is a possible perpetrator. Approaching the matter by considering who could be excluded from a ‘pool’ of possible perpetrators is to risk reversing the burden of proof. The court must consider the strength of the possibility that the person was involved as part of the overall circumstances of the case;
(e) In doing so, in future the court should first consider whether there is a ‘list’ of people who had the opportunity to cause the injury;
(f) The court should then consider whether it can identify the actual perpetrator on the balance of probability and should seek to do so. At this stage, the correct legal approach is to survey the evidence as a whole as it relates to each individual in order to arrive at a conclusion about whether the allegation has been made out in relation to one or other on a balance of probability. Evidentially, this will involve considering the individuals separately and together and comparing the probabilities in respect of each of them. Within this context, the right question is not ‘who is the more likely?’ but rather ‘does the evidence establish that this individual probably caused this injury?’ In a case where there are more than two possible perpetrators, the Court of Appeal highlighted a clear danger in identifying an individual simply because they are the likeliest candidate, as this can lead to an identification on evidence that falls short of a probability;
(g) Only if the court cannot identify the perpetrator to the civil standard of proof should it then go on to ask of each of those on the list whether there was a likelihood or real possibility that they caused the injuries. Only if there is, should that person be considered a possible perpetrator;
35. The commentary in Family Court Practice continues:
It is important to note that the court remains under a duty to consider the welfare of the child under ChA 1989, s 1(3) where that child has suffered injury and thereby significant harm, even where it is not possible to say who the perpetrator of harm is (Re S (A Child)). Note that the Court of Appeal has suggested that, in the context of the requirements of the Children Act 1989, s 31(2), the terms ‘non-accidental’ and ‘accidental’ injury are, in addition to being tautologous and oxymoronic, unhelpful, the threshold criteria not being concerned with intent or blame but rather with an objective standard of care (Re S (Split Hearing) [2014] 1 FLR 1421, CA). Where the court is satisfied that the child has suffered significant harm, the threshold conditions under ChA 1989, s 31(2)(b)(i) will be met in relation to that child even though the court is unable to identify who within the pool of possible perpetrators inflicted the harm: Lancashire County Council v B [2000] 1 FLR 583, HL, in which helpful guidance is given as to how evidence needs to be tested to establish the threshold criteria for the purposes of s 31 where the perpetrator is uncertain. In determining whether a person is properly included in the pool of potential perpetrators, it is essential that the court weighs any lies told by that person against any evidence that points away from them having been responsible for the injuries (H v City and Council of Swansea and Others [2011] EWCA Civ 195). In these ‘uncertain perpetrator’ cases, the correct approach is for the case to proceed at the welfare stage on the basis that each of the possible perpetrators is treated as such (Re O and N: Re B [2003] 1 FLR 1169, HL). The House of Lords held in that case that it would be grotesque if, because neither parent had been proved to be the perpetrator, the court had to proceed at the welfare stage as though the child were not at risk from either parent, even though one or other of them was the perpetrator of significant harm. The judge conducting the welfare hearing should have regard to the facts found at the preliminary hearing when they leave open the possibility that a parent or carer was a perpetrator of proved harm and that conclusion should not be excluded from consideration.
Evidence of Children
36. In Re P (Sexual Abuse: Finding of Fact Hearing) [2019] EWFC 27 (Fam) MacDonald J summarised matters to consider when assessing the memory of children:
577. That said, and considering the authorities set out above, the Report of the Inquiry into child abuse in Cleveland 1987 Cm 412 and Report of the Inquiry into the Removal of Children from Orkney in February 1991 among others and the contents of the current ABE Guidance, I am satisfied that this court can take judicial notice of the following matters:
i) Children, and especially young children, are suggestible.
ii) Memory is prone to error and easily influenced by the environment in which recall is invited.
iii) Memories can be confabulated from imagined experiences, it is possible to induce false memories and children can speak sincerely and emotionally about events that did not in fact occur.
iv) Allegations made by children may emerge in a piecemeal fashion, with children often not reporting events in a linear history, reporting them in a partial way and revisiting topics.
v) The wider circumstances of the child’s life may influence, explain or colour what the child is saying.
vi) Factors affecting when a child says something will include their capacity to understand their world and their role within it, requiring caution when interpreting children’s references to behaviour or parts of the body through the prism of adult learning or reading.
vii) Accounts given by children are susceptible to influence by leading or otherwise suggestive questions, repetition, pressure, threats, negative stereotyping and encouragement, reward or praise.
viii) Accounts given by children are susceptible to influence as the result of bias or preconceived ideas on the part of the interlocutor.
ix) Accounts given by children are susceptible to contamination by the statements of others, which contamination may influence a child’s responses.
x) Children may embellish or overlay a general theme with apparently convincing detail which can appear highly credible and be very difficult to detect, even for those who are experienced in dealing with children.
Police Interviews
37. The following is an extract from Family Court Practice summarising the law at para 2.338[2]:
Video-recorded interviews with children are hearsay evidence but may be admitted as evidence
of truth of the statement in family proceedings. Such interviews should be conducted in accordance with the detailed guidance in Achieving Best Evidence in Criminal Proceedings (ABE) (latest edition 2022) although this guidance is non-statutory. The court can make findings based on ABE evidence so long as it is alive to the hearsay nature of the evidence and the age of the children at the time of interview (Re M (Sexual Abuse: Evidence) [2010] EWCA Civ 1030). In TW v A City Council [2011] 1 FLR 1597, CA, the Court of Appeal found that the inadequacies of the ABE interview were so manifest, even allowing for a broad margin of latitude to anyone conducting such an interview, that no evidential weight could be placed on it. In particular, it was not sufficient for a judge to rely primarily on the fact that a child might be able to stand up to and overcome a thoroughly unsatisfactory interview; rather, a clear analysis of all the evidence was required and the child’s interview had to be assessed in that context. In Re W; Re F (Children) [2015] EWCA Civ 1300, the forensic value of the ABE interviews was found to be minimal such that the trial judge had been wrong to attach any weight to them. Whether the flaws in ABE evidence are so fundamental as to render the interviews wholly unreliable is a matter for the trial judge who must analyse the process thoroughly to evaluate whether any of the allegations made in such inter views can be relied upon (see Re E (A Child) (Evidence) [2017] 1 FLR 1675, CA, Re M-Y (Children) [2019] 1 FLR 79, CA and Re C (A Child) (Fact-Finding) [2022] EWCA Civ 584 where the Court of Appeal dismissed a father’s appeal against findings in care proceedings where criticisms were made of ABE interviews).
Hearsay evidence
38. Hearsay evidence is admissible pursuant to the Children (Admissibility of Hearsay Evidence) Order 1993 but I must assess the weight to be attached to it.
39. In Re W (Minors) (Wardship: Evidence) [1990] 1 FLR 203 Neill LJ at 227 said:
Hearsay evidence is admissible as a matter of law, but…this evidence and use to which it is put has to be handled with the greatest care and in such a way that, unless the interest of the child make it necessary, the rules of natural justice and the rights of the parents are fully and properly observed.
40. Butler-Sloss LJ (as she was) said this at 214:
In considering the extent to which, if at all, a judge would rely on the statements of a child made
to others, the age of the child, the context in which the statement was made, the surrounding circumstances, previous behaviour of the child, opportunities for the child to have knowledge from other sources, any knowledge, as in this case, of a child’s predisposition to tell untruths or to fantasise, are among the relevant considerations.
41. And at 218:
The reliability of the person relating what the child said is of vital importance.
42. The provisions of section 4 of the Civil Evidence Act 1995 apply:
4 Considerations relevant to weighing of hearsay evidence.
(1) In estimating the weight (if any) to be given to hearsay evidence in civil proceedings the court shall have regard to any circumstances from which any inference can reasonably be drawn as to the reliability or otherwise of the evidence.
(2) Regard may be had, in particular, to the following—
(a) whether it would have been reasonable and practicable for the party by whom the evidence was adduced to have produced the maker of the original statement as a witness;
(b) whether the original statement was made contemporaneously with the occurrence or existence of the matters stated;
(c) whether the evidence involves multiple hearsay;
(d) whether any person involved had any motive to conceal or misrepresent matters;
(e) whether the original statement was an edited account, or was made in collaboration with another or for a particular purpose;
(f) whether the circumstances in which the evidence is adduced as hearsay are such as to suggest an attempt to prevent proper evaluation of its weight.
Findings/Threshold
43. The Amended Schedule of Allegations sets out 40 paragraphs of findings that are sought.
44. Paragraphs 1-2 state the law in relation to threshold which I do not understand is in issue. Paragraph 3 sets out the section 31 Children Act 1989 threshold test. The Local Authority then set out the facts they seek to prove.
Agreed facts
45. Some of the allegations are agreed and I summarise them below:
5. CC was born in November 2023 by an emergency Caesarean Section during which no instrumentation was used. At birth his head circumference was noted to be on the 25th centile.
18. CC was born by Caesarean Section during which no obstetric instrumentation was used.
46. In fact all are agreed the notes indicate that Wrigley’s forceps were used during delivery. That is now agreed.
6. On 8 March 2023 [in fact it was 23 January 2024] CC was examined during his 8 week developmental check and his head circumference was noted to have increased to the 50th centile.
7. On presentation and examination at the paediatric assessment unit at A Hospital, 8 March 2024, CC was found to have a bulging anterior fontanelle with prominent scalp veins. His head circumference was noted to have increased to between the 75th and 98th centiles.
8. The following scans were taken in respect of CC (all except the 8/3/24 CT scan taken at Hospital B)–
• 8/3/24 - CT head scan (Hospital A)
• 9/3/24 - MRI brain and spine scan
• 11/3/24 - skeletal survey (Part 1)
• 20/3/24 - CT head scan
• 26/3/24 - cranial ultrasound scan
• 27/3/24 - skeletal survey (Part 2)
• 27/3/24 - CT head scan [in fact on 30 March 2024 per Dr Oates’ oral evidence]
• 8/4/24 - CT head scan
• 15/4/24 - CT head scan
21. There is no radiological evidence to suggest CC has or had a predisposition to fracturing.
22. The skull fractures were not caused by any underlying organic features or any medical condition capable of causing significant bone fragility.
25. The skull fractures were not caused by CC [] because he would have had insufficient mobility to self-sustain fractures.
27. It is not likely that the skull fractures [] were caused by a ‘clashing heads incident’ (as described by FC) because the forces involved in such an incident would be too trivial and would not have generated enough force to cause a skull fracture []. Such an incident could not have caused the skull fractures [] because it is very unlikely that a child of CC’s age [] would have been able to generate sufficient force to cause the severity of the injury.
Disputed or not agreed facts
47. The following findings are in issue; I have grouped them together:
Group 1: Subdural collections
9. CC presented with the following injuries-
(a) Multi-compartmental bilateral subdural collections containing haemorrhage surrounding the brain.
48. This is accepted by FC.
Group 2: Skull fracture
9. CC presented with the following injuries-
(b) two lucencies (linear discontinuities in bone) of the R parietal bone of the skull with no associated scalp swelling.
10. It is most likely that the lucencies are two separate R parietal fractures to the skull because-
(a) both lucencies are unilateral and widen towards an established major suture,
(b) they undergo a healing response over the course of the CT scans, and
(c) other normal variants which are present are unchanged.
Group 3: Skull fracture dating
11. It is likely that the skull fractures were caused in the period between 26 January - 8 March 2024 because the progressive healing response between the CT head scans shows that the skull fractures were most likely to have been not more than approximately 6 weeks old at the date of presentation on 8 March.
12. However, the absence of scalp swelling on either clinical or radiological examination is most consistent with any fractures being more than about 10 days old on 8 March 2024.
13. The skull fractures were therefore most likely to have been caused in the approximate period 26 January - 28 February 2024.
15. It is likely that the skull fractures occurred at the same or a similar time to the subdural collections by the same mechanism, or in the alternative it is likely that the skull fractures [I think this should read sub-dural collections] were caused by a separate shaking-type mechanism, or in the alternative it is possible that the skull fractures were caused after two separate impact events.
16. The skull fractures were likely to have occurred after significant and memorable events to anyone in attendance at the time.
49. Both M and FC now say the skull fractures occurred on or about 27 February 2024 and the Local Authority seek this finding.
Group 4: Subdural collections dating
14. It is most likely that CC’s intra-cranial injuries were caused by an episode or episodes of non-accidental injury on or about 27 February 2024 E108 but it is possible that they were between one and three weeks old at presentation on 8 March 2024 (ie: in the period 16 February - 1 March 2024) E132. The subdural collections were most likely to have been caused on or within a few days before 27 February 2024 and after the time that CC was last completely well, feeding and handling normally.
17. The intra-cranial injury was most likely to have been sustained at the time when CC started to be sleepy and sick on 27 Feb 2024.
50. As noted above, the Local Authority now say the intracranial injury was caused on or about 27 February. M and FC now also invite that finding.
Group 5: Skull fracture mechanism
19. The skull fractures were not caused by birth-related trauma or injury.
51. FC now explicitly accepts this and M does so implicitly.
23. CC has no identified underlying blood clotting disorder that could have caused the skull fractures.
52. Implicitly FC and M now accept this.
26. The parents have not disclosed or described any episode of accidental trauma which could have caused the skull fractures.
29. It is most likely that the skull fractures were caused non-accidentally by a significant impact injury to the head involving blunt impact force with a hard surface during a forceful event that involved greater handling than encountered in normal life.
53. M and FC now invite this finding, save that FC says it must have been a culpable accident.
35. It is most likely that shaking and an impact were aspects of a single causal mechanism, namely a single head injury.
54. FC invites a finding of a single incident.
Group 6: Subdural collections mechanism
20. The large multifocal subdural collections were not caused by birth trauma.
55. FC now explicitly accepts this and M does so implicitly.
24. CC has no identified underlying blood clotting disorder that could have caused the subdural bleeding.
56. Implicitly FC and M now accept this.
32. It is not likely that the subdural collections were caused by an underlying brain abnormality, brain infection or a structural brain abnormality.
57. FC accepts this allegation, as does M implicitly.
27. It is not likely that [] the subdural bleeding were caused by a ‘clashing heads incident’ (as described by FC) because the forces involved in such an incident would be too trivial and would not have generated enough force to cause [] the multi-focal subdural bleeding. Such an incident could not have caused [] the brain injuries because it is very unlikely that a child of CC’s age (3 months 10 days) would have been able to generate sufficient force to cause the severity of the injury.
58. M and FC implicitly accept this.
30. The brain injuries were more likely to have been caused by a rapid/repetitive acceleration/deceleration (for example, shaking), rather than an impact injury, because of the multifocal nature of the injuries or alternatively, although such a significant impact event may have been sufficient to cause the diffuse subdural collections (if there were associated excessive acceleration/deceleration forces), this would be atypical, and a co-existing abusive, shaking-type injury remains a possibility.
31. The substantial impact with an unyielding object with sufficient force to have caused the skull fractures could also have caused some, if not all, subdural bleeding.
59. FC invites this finding.
33. It is not likely that that an accidental trauma could have caused the brain injuries.
34. Trauma is the most likely cause of the subdural collections.
35. It is most likely that shaking and an impact were aspects of a single causal mechanism, namely a single head injury.
60. FC invites this finding.
Group 7: Perpetrators
36. On 27 February 2024 FC had taken drugs and/or alcohol whilst caring for the three children alone.
61. FC now accepts this.
37. The injuries to CC were caused by FC on or about 27 February 2024 whilst in FC’s sole care.
62. FC now accepts this but says it was the result of an accidental but culpable (through alcohol and possible drug use impairment) incident. M invites a finding of deliberate infliction.
Group 8: Observers
28. The level of force needed to cause the skull fractures and/or the subdural bleeding would have been obviously excessive to a normally competent and responsible person.
63. FC accepts this, but M seeks to test the evidence.
38. The skull fractures would have been initially very painful, typically for about ten minutes (unless CC was rendered unconscious by the causal event).
39. FC would have realised that CC had been hurt.
40. As the person not witnessing the event and caring for him, M might have found him to be fractious, but would not have realised the cause unless or until a scalp swelling was found.
64. FC accepted this allegation in its unamended form where it was neutral on the person not witnessing the event and used the words “might not have realised” instead of “would not have realised”.
Credibility
Mother
65. When M gave evidence she did so calmly although became upset at times. I was particularly struck by her self-reflection; she gave evidence on having searched the internet for information on Borderline Personality Disorder which she felt she may suffer from and reflected on the relationship with FC being unhealthy. I also noted that even when pressed if she did not recall something she generally stuck to her guns and said she did not remember. Asked about the incident when CC and FC clashed heads she said “some bits stick out, others don’t” which I found to be a fair assessment of memory generally.
66. I was also struck by her refreshingly honest response to questions about her time in hospital with CC. In the social worker’s initial statement she said:
[C15]
3.1.20 At the re-strategy meetings held on 11th March 2024 and 13th March 2024, the safeguarding nurse reported that nursing staff on [] Ward had noted that M was not always attentive to CC’s needs. M required prompting at times to change his nappy and respond when he was crying.
67. This was not very flattering of M but rather than denying it she accepted on occasion she did need prompting and she volunteered “I was on my phone more than I should have been” and her explanation was she “knew what CC needed but because of trauma response I wasn’t quite up to scratch”.
68. At one point in cross-examination M was asked about whether there had ever been occasions when she had come into the room CC was in to find CB had picked him up. She initially said she could not recall that having happened but when taken to Paternal Grandmother’s statement to police she accepted it had. I adjourned briefly as I was concerned M was answering questions without thinking or in order to speed the end of cross-examination. When she returned she once more said she could not remember but said it may have happened.
Father FC
69. FC’s evidence started badly in that he gave his address as his mother’s home but later had to admit he was not living there but at his girlfriend’s; even that simple information had to be extracted from him in this exchange (my emphasis):
|
Q At beginning of your evidence you gave your address A [Address given], it’s my mum’s address |
|
Q The social worker has spoken with her today and you’ve not been living there for months A I have for many months Q The social worker was astonished by your evidence A I currently live with a new girlfriend, I’ve been staying at mum’s just not fulltime Q Why lie to the court at the beginning A I don’t know why JQ Do you accept you’ve lied A I accept for the last couple of months I’ve been staying with my new girlfriend That’s the address I give for all my mail to go to I have stayed overnight once within last 1.5 to 2 months but predominantly at new girlfriend for last 3 months Maybe I thought it was where letters were sent to |
|
… |
|
JQ Why not give girlfriend’s address A I can’t give a reason |
70. As his evidence continued I came to the gradual realisation I could place no weight at all on what he told me unless it was corroborated by other evidence. His evidence was shot through with lies and evasion:
a) He was asked who a particular person referred to in text messages was and denied knowing anyone by that name except Maternal Grandfather. Later he said he also knew someone’s ex-partner by that name and he had been “mistaken”;
b) He was asked if he was “trying to set up a sexual liaison on more than one occasion after CC was born” and he acknowledged he had done so on 9 March as evidenced by text messages but then had to accept it was in fact on more than one occasion;
c) He agreed M was right to call him a liar in relation to his liaisons with other women;
d) He agreed he allowed M to believe she was “going a bit crazy imagining” he was seeing other women;
e) On the first day of his oral evidence he said he never drank alcohol when he had care of the children. On the second day he said he did not drink when looking after the children, he agreed that was an absolute rule. He had told the police in interview on 18 March 2024 he would not be drunk in charge of looking after CC but agreed he might have 2-3 cans [O80]. His only explanation for the difference was he told the police it was a “possibility” but of course it would not have been a possibility if it was an absolute rule. When taken to an earlier part of the interview in which he had said he was with the kids and “it would be a few, few beers” [O76] he said he did not mean it was when he had sole care of the children. In any event, at the end of his cross-examination he came to accept that his memory was “utterly impaired” on the night of 27 February 2024 and it was “quite possible” he had drunk so much he could not remember the events of that night when all three children were in his care and it was a lie to have said he never drank whilst the children were in his sole care;
f) He said he did not think there had been allegations of domestic abuse in his relationship with his current girlfriend; he was asked if there had been an incident involving damage to her property and said there had been a party and “a window got broken and we were all questioned”. There was no mention of a party in the police record at [Z261] which described him kicking and punching the glass after an argument; when taken to it he accepted that was in fact true, he shouted at her through the door and kicked and punched the glass, he agreed the fact the police were called was nothing to do with a party, he then agreed that shouting, punching and kicking the glass was domestic abuse;
g) He was asked if that was the only time he had been in trouble for an incident with criminal damage and said as far as he could remember it was, but when confronted with a report from October 2022 [O141] it “came back” to him that he had an argument with a previous girlfriend. He evaded answering whether this was controlling behaviour by saying he accepted the messages alleged to have been sent were sent. When pressed he agreed it was and agreed he had changed his view over the 20 seconds of cross-examination that preceded it; when confronted by the report that he was “screaming at her and began to damage her property” he agreed he had broken a mirror and said “now we are talking about it I remember” another incident of criminal damage;
h) In cross-examination he was asked about treatment for drug and alcohol addiction. He said he had “possibly made calls” to set up addiction counselling in the last month yet in his statement of 15 April 2024 [C54], repeated in a revised version of 17 May 2024 he said he was “seeking assistance from Turning Point or similar” [C77]. When I asked him why he had not mentioned that in oral evidence he said he sought help and then stopped but could not give an explanation for not giving that oral evidence;
i) He accepted in cross-examination that he had an alcohol addiction but in his statement he had said “drug and alcohol use…was purely on a recreational basis” [C54/5]. His explanation was he meant that cocaine use was recreational not alcohol use but that is plainly not how the statement is worded and he confirmed its contents at the outset of his oral evidence;
j) He accepted that when first spoken to by the police on 9 March 2024 he lied in saying he did not use drugs [O205];
k) He accepted that when he spoke to the social worker on 14 March 2024 he lied when he said cocaine use was “in his past and it has never been around the children” [F62]. He later agreed it was in fact a possibility he used cocaine in the bathroom at home, he would “put it on a card and snort it”;
l) He accepted that in interview by the police on 18 March 2024 he lied in saying “I’ve tried cocaine a few times” as his use was more regular and ongoing [O77];
m) He accepted that in the same interview he lied in saying he last used drugs “like, three, three months ago” [O78];
n) He accepted in the same interview he lied when he said, in relation to CA and CB’s allegation they had heard a thud and FC swearing when CC was in his care in early February, “that definitely wouldn’t have happened. No, No.” [O79] and “there was no…there was no swearing” [[O80]. He told me “I’m holding my hands up to say I have lied to the police”;
o) He accepted he lied in his hair strand test declaration on 8 April 2024 by saying he used cocaine “occasionally”, when it was more than occasionally [E6];
p) He accepted he lied in his hair strand test declaration on 5 September 2024 saying he used cocaine “a couple of times over four months” when he was still a heavy user [E249] and he under declared his alcohol use at 6-12 cans of beer in a typical week. FC had significant difficulty explaining what the true picture was; first he said “sometimes over 6 in a week”, then “it could be way more than that” then said up to 20 cans a week, then some weeks it could be over 20 cans and eventually said “between 20 and 30”;
q) He was asked in relation to drinking alcohol when it was that his speech would start to slur and he said “after about 6 cans” but when he was taken to his police interview on 18 March 2024 he had said his voice changes after “one or two beers” [O79];
r) He was asked about arranging a drug delivery on 2 March 2024 and he said it was to arrange a delivery to a friend, but could not initially explain why there were no messages from him to the friend then a few moments later said he “may have used my iPad” to message him and when I asked why he had not mentioned that earlier he said he “didn’t think it was necessary”;
s) He was asked where he kept his cocaine and initially said he did not store it anywhere. When it was put to him he was found in possession of drugs in 2022 he said in his pocket; he denied he would have it in the home except for traces in baggies in his pocket. But he could not explain why he would carry empty baggies, and in answer to my question agreed he would use it before returning home. But in almost the next exchange he agreed there were times when his dealer would in fact deliver to the home, then in answer to a later question said there might have been cocaine in the home when M was in hospital and agreed he had lied. He said that he should not have said there would only be empty baggies and said he would keep partial or full baggies in his clothes cupboard or trouser pockets. He could not give an explanation for lying about it in court under oath;
t) He accepted his description of what happened during the 111 call on 29 February 2024, as given to the police on 9 March 2024 [O204], was quite possibly “nonsense”. He accepted his statement of 14 October 2024 in relation to what happened whilst on the call was largely incorrect;
u) He eventually accepted what he told the police about M having rung him on 8 March 2024 saying CC was “coughing up bile” [O205] was “nonsense” and lies; there was no call at all and therefore he had not “insisted” that M try to get a doctor’s appointment;
v) In a series of questions towards the end of cross-examination he made the following admissions:
|
Q You lied to police A Correct Q You lied to M A I did Q You lied to police not just at debrief but in interview A [Nod] Q You have lied in court witness statement A [Nod] Q You’ve told me that you’ve lied in court today A I have |
71. There were other aspects of FC’s evidence that lacked credibility or caused concern about his credibility:
w) In relation to cocaine use he initially said he would use drugs before returning home and that even when he could not resist the craving for alcohol he was able to resist the craving for cocaine that would follow drinking alcohol. I find that very difficult to accept;
x) When asked whether he had been impaired by alcohol or drugs when he prepared his most recent statement he agreed he “was pissed” when it was made; and
y) He repeatedly said he could not remember events at Hospital A on 8 March 2024. He was spoken to with M at 20.33 [L31-L32]. He said “I was drunk” by way of explanation for not remembering, yet the police attended the family home where he was present with the children at 21.37 [O519] and he was able to have lucid conversations and gave no appearance at all of being drunk in the BWV. He could not give an explanation for having gone from so drunk he could not remember to being lucid.
Group 1: Subdural collections
72. Dr Oates recorded extensive subdural fluid overlying the front and temporal lobes bilaterally and in between the cerebral hemispheres.
73. Mr Jalloh identified “large watery bilateral subdural fluid collections” from the MRI of 9 March 2024 [E118/3.54].
74. I accept CC presented with multi-compartmental bilateral subdural collections containing haemorrhage surrounding the brain.
Group 2: Skull fracture
75. In his report Dr Oates identified 2 lucencies, one extending anteriorly from the midpoint of the right lambdoid suture to the central aspect of the right parietal bone and the other extending inferiorly from the anterior aspect of the sagittal suture to the central aspect of the right parietal bone [E137] and concluded:
[E138]
Based on this single CT appearance, the lucencies may reflect normal variant accessory sutures/fissures or alternatively fractures to the skull bones. However, given the evolution in appearance of the lucencies over multiple follow-up CT scans, I believe they are most likely to reflect skull fractures.
76. Dr Oates compared the CT scan of 20 March 2024 with that of 8 March 2024 and recorded:
[E145]
• Of note, the previously described two discrete linear lucencies extending through the right parietal bone are now becoming indistinct.
o In addition, there is evidence of faint, bone-like material traversing the fractures site.
▪ This is despite the sutures remaining widely patent.
o I believe this finding, and the continued evolution over the subsequent CT scans of 30/03/2024, 08/04/2024 and 15/04/2024, leads me to conclude that the lucencies are most likely to reflect fractures.
77. He also considered the skull fractures were “more widely spaced than normal and likely secondary to the large subdural collections creating pressure effects on the skull.” [E139]. Later CT scanning on 30 March 2024 showed less well defined margins to the lucencies “with what appears to be evolving fracture healing” [E150] and on 8 April 2024 “Further progressive healing of the right parietal skull fractures with bridging of the fracture by new bone formation” [E151] with a similar report from the CT scan of 15 April 2024 [E152] and 30 April 2024 [E154]. His conclusion was:
[E157]
Based on the appearance over the course of the 5 CT scans, I believe it is most likely that lucencies are skull fractures. I say this because both lucencies are unilateral (i.e. only one side of the skull) and widen towards an established major suture, but most importantly they undergo a healing response over the course of the CT’s…I cannot say with absolute certainty that they are skull fractures (as opposed to normal variants) but I would not anticipate the latter to “heal” in such a manner even with the potential variable of the fluctuating intracranial pressures due to the subdural collections. (Of note, the other normal variants evident e.g. bilateral occipital foramen and small sagittal membranous fissures are unchanged).
78. Mr Jalloh identified lucency in the right parietal bone on CT scanning on 20 March 2024 [E118/3.56].
79. I conclude CC suffered 2 parietal fractures to the skull.
Group 3: Skull fracture dating
80. In the police notes of a conversation with FC on 9 March 2024 the following was recorded:
[O415]
FC first noticed something was wrong with CC approx. 9 days ago. He had been at work all day and when he returned CC appeared normal...On recommendation from the Dr that when babies teeth they can have Calpol, they gave CC some Calpol quite quickly after this feed. Immediately CC projectile vomited so they rang 111. Whilst on the phone CC became rigid. FC demonstrated
this by holding his arms in the air. FC stated he could not get CC’s arms to go down and this lasted for 10-15seconds.
[O416]
…FC said CC has been sleeping too much…
81. When M gave evidence she said that she could date the time CC began to be unwell was after she went to hospital on 27 February 2024 and he was “sickly” in the early hours of 28 February. She said the incident of FC and CC clashing heads was after that.
82. In the notes in respect of M:
[O417]
Last Tuesday [27 February 2024] CC started vomiting, so I took him to my local GP [] on FRIDAY 1ST MARCH 2024 because CC was vomiting a lot…
…
I took CC to [] MEDICAL CENTRE again on TUESDAY 5TH MARCH 2024 because CC was still throwing up…
83. In her first statement M says that she was admitted to Hospital A on 1 February 2024 with a chest infection and CC was in the care of FC for 5 days until 6 February 2024 [C70/23-24]. CC was then in the joint care of M and FC until M was re-admitted on 27 February to 28 February 2024 [C70/25-27]. She then describes CC as “a lot more sleepy” and “being sick” on the morning after her discharge, i.e. on 28 February 2024 [C70/28]. During the period 5-8 March 2024 “he was being sick and was very grisly but more than anything I found that he was very sleeping and not his usual happy self” [C71/33-35].
84. Dr Oates’ opinion having regard to 5 CT scans over 5 weeks starting on 8 March 2024 was:
[E163]
Ultimately, given the rapid evolution between CT scans, I believe the skull fractures were unlikely to be longstanding and I would estimate not more than approximately 6 weeks old at presentation (and possibly much more recent).
85. He elaborated in cross-examination saying that the evolution of the fracture healing response on CT scanning “was rapid” and he could not account for no healing response for more than 6 weeks prior to 8 March 2024; he considered “it is more likely the fracture was sustained closer to the 8 March end of the window” than earlier in the 6 week period, “logically it is more recent to the time of presentation”, but did acknowledge there is no rigorous evidence base. It was, he said, a “sensible estimation”.
86. He was more reticent about using scalp swelling to assist in dating, saying there was “no rigorous evidence base” [E164]; although in oral evidence, when asked if the absence of scalp swelling on CT scanning on 8 March 2024 militated against a skull fracture in the last 2 weeks, he said that in the majority of skull fractures scalp swelling occurs within a few hours and resolves within 2 weeks (i.e. implicitly accepting it does so militate) but “it’s difficult to be certain”.
87. My summary of Dr Oates’ evidence is that the window for the skull fracture is 26 January to 8 March 2024; logic suggests closer to the 8 March end of the spectrum but the absence of scalp swelling possibly suggests it was before 23 February 2024.
88. Mr Jalloh’s opinion was:
[E126/4.44]
Invariably, skull fractures caused by trauma are associated with scalp swelling which is not always obvious clinically but would be seen on CT and is typically visible for at least 2 weeks.
[E127/4.46]
The absence of scalp swelling implies the skull fracture would be at least 2 weeks old by the time of the CT scan on 08 March 2024 i.e., caused by an episode of trauma on or before 23 February.
89. He was asked about scalp swelling in cross-examination and said in the vast majority of cases “skull fracture from recent trauma would be associated with scalp swelling but even on imaging we do not always see scalp swelling”. He later confirmed the absence of scalp swelling “would not necessarily preclude an episode of trauma”.
90. It follows from this that his opinion is the trauma was likely on or before 23 February but that was not absolute.
91. Dr Cartlidge’s view was that “The rate of onset and extent of a scalp swelling is variable” [E187] and “A traumatic scalp swelling usually disappears within about 10-14 days” and he therefore concludes the absence of the same on 8 March 2024 is “most consistent with any fractures being more than about 10 days old”. That would date them on or before 27 February 2024 but in cross-examination he said “absence could be it never formed” so implicitly the trauma could have been after 27 February.
92. In relation to clinical signs Dr Cartlidge considered that “there would be distress from the fracture but I agree that could be relatively brief at 10-15 minutes and then maybe an hour or so later could return to normal”. He agreed in cross-examination that there was “no solid anchor on which to fix the timing of the causative event” and that he had not “seen anything that points with confidence…not seen anything that indicates when the skull fracture was sustained”. He then clarified he would “lessen the amount of confidence” in his overall assessment that the causal event was 1.5 to 3 weeks prior to 8-9 March 2024 (i.e. the last bullet point of his report at [E201/4.5]).
93. When asked to look specifically at 27 February 2024 as a possible date for infliction of injury there was this exchange in cross-examination:
|
Q We then move to 27 February 2024 and this is the beginning of the period we have to look at with CC being presented for medical attention, on 27 February 2024 M became unwell again and went back to hospital for second time and was there from afternoon of 27th to early hours on 28th, whilst she was at hospital FC is caring for the baby and whilst in hospital M received a number of messages from him including on 27 February 2024 at 18.59 “He still hasn’t stopped screaming” and 28 February 2024 at 00.34 “He keeps shitting and screaming” M got home on 28 February and found CC to be unusually sleepy and was more regularly sick, that’s not constant sickness because intermittently he’s able to take bottles but sufficient to worry M enough to go back to hospital and back to the GP Can we piece together that sequence of events Screaming and not settling is consistent with head injury just caused? A Yes |
94. And then:
|
Q Intermittent vomiting and poor feeding through the period…1 March 2024 took a bottle and 4 March able to tolerate feed but M reporting reduced intake and finally 8 March where we know severe symptoms, do we see a picture then of the symptoms of the subdural collection developing over time, overtaking any degree of encephalopathy, does that make sense? A Yes, as one gets more information about how unwell CC was, if impression of gradually getting worse then that’s most consistent with symptoms being part of the chronic lesion getting worse, with the acute injury I’d expect a step change but it may only last for a brief period, 15mins or an hour but after that because no injury to brain could be a return to virtual normal before symptoms of chronic subdural, ie sickness, sleepiness develop, a biphasic history I’m looking for If this is gradually deteriorating between 28 February and 8 March most likely chronic lesion, if you can identify something that happened and then a gradual worsening you’re identifying an acute injury and then gradual worsening Q We see FC reporting very significant distress and some symptoms of diarrhoea and then settled on 28th and deterioration thereafter, we’ve potentially got both phases A Potentially, yes |
95. Later he confirmed the scenario of distress on 27 February “links in to a biphasic scenario”.
96. I conclude the likely date of fracturing on the medical evidence was between 26 January 2024 and on or shortly after 27 February 2024. I discount the possibility of the end of the window being as early at 23 February 2024 having regard to the uncertainty about scalp swelling.
Group 4: Subdural collections dating
97. Dr Oates’ opinion was that the absence of membranes on the MRI of 9 March 2024 suggest trauma was less than 2-3 weeks prior although he did note “that long standing subdural collections do not always form membranes” [E164]. In cross-examination he confirmed because membranes do not always develop it is “difficult to say the injury was not more than 3 weeks prior to the scan”.
98. He said the size of the collections would only occur after a number of days or weeks (if it was over a shorter timescale CC would have been profoundly unwell) [E164]. He concluded “the subdural collections were greater than 1 week old at presentation and possibly up to approximately 3 weeks old” [E164]. He clarified in oral evidence the assessment of 1 week was because the collection was of low attenuation on CT scanning (dark) which suggests it was not acute. In summary his evidence was the window for the intracranial injury is 16 February to 1 March 2024.
99. Mr Jalloh reported:
[E126]
4.40 CC’s clinical presentation with vomiting, macrocephaly (enlarged head circumference with separation of the skull sutures) and tense fontanelle is consistent with the relatively large subdural fluid collections, which continued to increase in volume during the early part of his inpatient stay. The enlarged head circumference and separation of skull sutures occurs when the skull compartment is gradually expanded to accommodate the fluid. The gradual accumulation of fluid is likely to occur over the course of days (or even weeks) rather than hours. A more rapid accumulation of fluid would squash the brain rather than expand the skull, leading to a rapid collapse.
4.41 In summary, CC’s vomiting was primarily due to raised intracranial pressure caused by progressively enlarging subdural collections and possibly encephalopathy caused by an episode of trauma. His vomiting was first reported to healthcare on 29 February 2024. On 01 March he was noted by the GP and paediatric registrar to have a normal fontanelle consistent with subdural collections that had not yet reached a critical size. On balance, the subdural collections were likely caused on or within a few days before the 29 February, and after the Court finds that CC was completely well, feeding and handling normally.
100.However, he acknowledged the possibility of an earlier trauma which might be consistent with his dating of a skull fracture:
[E127]
4.46…In my opinion, it is possible that the subdural collections were caused by an episode of trauma on or within a few days of 23 February with vomiting only becoming apparent when progressively enlarging subdural collections had reached a size to become symptomatic (on 29 February).
101.In cross-examination Mr Jalloh was asked about the relevance of FC’s evidence that CC was bottle fed but “grizzly” on 29 February 2024 and 2 hours later vomited and then went “rigid” [Z54]. He was not able to say that that either did or did not mark the onset of symptoms from a subdural collection. The vomiting was “relatively non specific”; going rigid may have been commensurate with having vomited and being grizzly may either have been from teething or the start of symptoms from a subdural collection. Later he confirmed “it is difficult to be overly precise”. In short he could not date the infliction of injury as specifically before or after 29 February 2024.
102.In relation to the formation of membranes Mr Jalloh said:
[E125]
The absence of any visible subdural membranes on the MRI plus the re-accumulation of subdural fluid after initial drainage due to on-going CSF leak, suggests the subdural collections are consistent with a recent episode of trauma rather than long-standing chronic subdural collections.
103.As with Dr Oates, he was cautious about membranes; they probably always occur but it might depend on where the collection was and they may be too small to see on a scan but their absence “does carry some weight”.
104.Dr Cartlidge agreed with Dr Oates’ analysis; sometimes membranes do not in fact develop. Therefore this method of dating has limitations but he considered the likely causative event was 1-3 weeks before 8-9 March 2024 [E194] i.e. between 16 February 2024 and 1 March 2024. He deferred to Dr Oates in so far as the radiological signs are concerned [E200]. From a clinical perspective he said “I think it probable that it occurred shortly before CC developed the sleepiness and sickness on 28 February 2024” [E201].
105.When he gave oral evidence there was extensive cross-examination on the clinical signs of injury. He felt that “there would have been a change in demeanour but it may not have been profound as there was no injury to the substance of the brain…symptoms may have been at the mild end…the demeanour may have only lasted an hour and then got worse when pressure inside the head increased”. The reference to an hour is a reference to his later evidence about the clinical signs of skull fracture (see above in relation to Group 3 findings). He said that after injury the child could “return to normal and the subdural bleeding can be relatively silent and only become symptomatic as it increases in volume in the head causing sleepiness and sickness” and agreed a logical sequence was “subdural bleeding becomes chronic collection and expands in size and the sutures in the head accommodate that expansion but only up to a point and at a point, an unspecified point the raised pressure can no longer be accommodated and CC becomes symptomatic”.
106.He was taken to the report of CC going rigid [Z54] and agreed there was not sufficient information to link that to a causal event, and later he agreed with Mr Jalloh that rigidity could just be a baby in distress or pain. He agreed that “timing of the originating insult…is plainly clouded by the identification of only non-specific symptoms” but he said observation was important, and later:
…it’s the persistence of symptoms, I assumed the symptoms persisted as low level lethargic, not quite right manner and you want to find out why and the only thing we found out was a subdural collection developing
[Sleepiness] is much more likely symptoms of chronic subdural [than something innocuous]
107.Noting there was reported sleepiness on 5 February 2024, he said that could have been caused by a developing chronic subdural collection which was worsened by a later re-bleed at the end of February but “the further back you go without symptoms the more improbable it becomes in my mind” and specifically an event on 4 February 2024 was a possibility still. Of the 5 February symptoms themselves, he said they were “non-specific…the only real thing is sleepiness but that’s common with a baby with anything”.
108.He was asked about the early part of the window given in his report, given the limited reliance that can be placed on the formation of membranes in the collection and he said it fits with the normotensive anterior fontanelle noted by the GP on 1 March 2024. But on that point he could not disregard the possibility that the GP observation was incorrect (given the GP was probably assessing the possibility of a depressed rather than tense fontanelle indicative of dehydration given the reports of vomiting) and even if the anterior fontanelle was in fact normotensive on 1 March it is still possible there was “a little bleeding after 1 March and that tipped the balance”. 2 weeks prior to 1 March was not the maximum time for chronic subdural collections to be reflected in a tense anterior fontanelle. He said “I don’t want the court to think I’m very confident with that timescale it’s just that it’s the most likely for me”.
109.Ultimately what it came to was that, as in relation to the skull fracture, he was less confident in his written evidence that the traumatic event was within 1.5 to 3 weeks of 8-9 March 2024.
110.I conclude the likely date for intra-cranial injury on the medical evidence is between 16 February 2024 and 1 March 2024.
Group 5: Skull fracture mechanism
111.Dr Oates concluded that “a simple skull fracture can occur from as low as 50 cm although this is certainly not the norm” and “the fractures would only occur after significant and memorable events to anyone in attendance” [E159]. In cross-examination he considered that a fall from a carer’s arms “would be compatible although it would be unusual”.
112.In relation to FC’s account of a clash of heads he said:
[E165]
I find it very unlikely that a 3-month-old infant will be able to generate sufficient force to cause the severity of injury as seen.
113.He considered that “The use of forceps at birth would not influence [his] radiological interpretation as described” in his report (from an email dated 9 October 2024 not in the bundle). In his oral evidence he said radiologically he could not determine if the cause of fractures was 1 or 2 events.
114.Mr Jalloh reported:
[E122]
4.12 The CT showed a lucency (gap) in the parietal bone which is either a skull fracture or an accessory suture (a variant of normal that infants are born with and not caused by trauma). It can be difficult to differentiate between these two particularly in the absence of any scalp swelling, which was not reported on CC’s scans.
115.He considered “there is still the possibility of an unrecognised skull fracture occurring at the time of birth” [E123/4.21] and in his addendum report “the use of forceps during CC’s delivery does not alter the conclusions set out in my report” [Z12] which was that “an unrecognised linear skull fracture from birth is possible but unlikely” [E124/4.23].
116.He considered “bumping heads” would involve forces “too trivial to cause a skull fracture” [E124/4.25].
117.In relation to possible cause he said:
[E124]
4.29 If the Court finds that CC has a skull fracture, then an episode of non-accidental injury involving blunt impact force with a hard surface is a possible cause.
…
4.31…An episode or episodes of non-accidental injury is the most likely cause.
[E125]
4.33…Normal handling and minor domestic accidents would not be expected to cause any injury at all.
118.Mr Jalloh accepted a fall from a carer’s arms could cause a skull fracture.
119.Dr Cartlidge has ruled out medical conditions capable of causing bone fragility [E188-E190]. He considered the likely mechanism was “the head impacting with an unyielding object” [E190]. He rules out birth related trauma (caesarean section not likely and Dr Oates’ evidence of dating incompatible) and self-sustained trauma (infant not having sufficient mobility) [E191].
120.In relation to birth trauma he considered the reference in the obstetric notes to “high head” [L585] on delivery suggests not low in the birth canal and “if anything [the head] is floating around” and the overall likelihood of Wrigley’s forceps causing a fracture is small.
121.He analysed FC’s account of the clash of heads in this way:
[E192]
• The timing of the event is consistent with the medical ageing of the probable skull fractures (and the intracranial injuries).
• The description of the event lacks sufficient detail to assess whether a force equivalent to a free-fall of at least 50 cm [see discussion at [E190/4.3.5] for this measurement’s genesis] onto an unyielding object could have been generated. Yet, I think such a force would not be generated by CC’s head wobbling around because he lacked developmental maturity to have good head control.
• The description of the event lacks sufficient detail to assess whether CC was as distressed by the impact as I would expect.
• The movement of the head of such a young infant is primarily wobbling back and forth. Any impact would usually be against the forehead or a temple. Yet, the probable skull fractures to CC were at the back-right of the head.
In my opinion, this event did not cause any skull fractures.
122.He concluded the most likely mechanism was a non-accidental cause.
123.My conclusion is that birth injury is very unlikely, the clash of heads incident is essentially ruled out and a fall from a carer’s arms and inflicted injury are possible causes.
Group 6: Subdural collections mechanism
124.Dr Keenan has identified no blood clotting disorder that could account for the subdural collections [Z95].
125.Dr Oates considered a number of differential diagnoses and concluded the most likely cause of subdural collections was trauma [E160]. He considered that whilst bilateral subdural collections “theoretically may have been caused by a very significant impact injury” “when head trauma is secondary to an impact injury”, it tends to be localised adjacent to the site of impact [E162].
126.Shaking can result in collections of blood from tears of bridging veins [E162] and CSF from disrupted arachnoid membranes. He concluded:
[E163]
Ultimately reviewing the entirety of the findings, I believe it is most likely that CC has sustained a significant impact injury to the head to cause the skull fractures. This impact event may have also been sufficient to cause the diffuse subdural collections (if there were associated excessive acceleration/deceleration forces). However, this would be atypical, and the possibility of a coexisting abusive, shaking-type injury remains a possibility.
127.In oral evidence he confirmed he was “confident there’s been at least one impact” but bilateral subdural collections would be atypical. The collections were also “slightly unusual” in that they “continued to get larger even with tapping and the drain being put in, this atypical appearance makes it more difficult to say if they were part of the initial impact injury”, and it is possible they could be caused by a single impact but “it would be unusual secondary to a single impact…it’s possible at the time of the initial impact they were very small and continued to get larger”. He then said that it was “more likely there was an associated shaking mechanism” because “it’s unusual to get disruption to the dura with an impact injury”. He was cross-examined on the absence of other indicators of shaking (spinal bleeding, metaphyseal lesions of the long bones, retinal haemorrhages), but went on to say:
Any traumatic event is a spectrum, the absence of other shaking symptoms may reflect there is a spectrum and the anchor point is there’s definitely been the impact injury and if hit the floor causing 2 fractures is that sufficient to move the brain backwards and forwards? I can’t exclude that possibility.
128.As I understood his evidence he also acknowledged relative movement (brain in skull) as part of a swinging motion.
129.As above, he said of FC’s explanation of a clash of heads:
[E165]
I find it very unlikely that a 3-month-old infant will be able to generate sufficient force to cause the severity of injury as seen.
130.He was cross-examined on the possibility of birth trauma as a cause. He acknowledged the research on the incidence and resolution of birth related subdural bleeds is “not complete” but in clinical practice he reviews a large number of MRI and CT scans in the 2-4 month age group and it would be “vanishingly rare” for there to be chronic subdural haematoma (i.e. from birth) at 3 months. He did not rule it out “but it’s unlikely”. In reaching that conclusion he considered the “preponderance of dark fluid with small bright” attenuation consistent with chronic collections of blood or mixed blood and CSF and discreet rebleeding, but took account of the absence of membranes and pointed to other markers reported: rapid increase in head circumference and fontanelle fullness.
131.He was also asked about the possibility of Benign Enlargement of the Subarachnoid Spaces (BESS) which some researchers have associated “with subdural haemorrhage after minor trauma secondary to disruption of the tensioned blood vessels traversing through the enlarged subarachnoid space” [E161]. His evidence in cross-examination was that there was no evidence to support this as a cause, but he could not exclude it. In particular, he noted that the subarachnoid spaces are fluid filled, with their own mass effect “so it is difficult to see they’d be compressed [by subdural collections] and mask BESS.”
132.He was asked about multi-focal collections from low level falls and agreed “we put low level falls causing skull fracture and subdural collections in the unusual box”.
133.Mr Jalloh considered subdural haemorrhage was caused by mechanical trauma [E121/4.5]. He said “rapid/repetitive acceleration-deceleration…produces an injury pattern reflecting energy distribution across the whole head” as opposed to impact type injuries “that tend to produce only a focal subdural bleed, just on one side of the head, rather than multifocal as in this case” and “rarely, an impact type injury will be of sufficient force/energy to cause significant inertial acceleration-deceleration of the brain and a multifocal distribution of subdural fluid” [E121/4.7]. He confirmed in oral evidence it “would be rare, it’s not likely” that a single impact injury would have caused multifocal collections.
134.He referred to studies suggesting that birth-related subdural haemorrhages “resolve within a few weeks” and there was “no clinical evidence of chronic subdural collections prior to CC developing vomiting, such as macrocephaly at the 8-week baby check, which would be expected if chronic subdural collections were established at the time of birth.” [E123/4.20]. In his oral evidence he agreed it is possible that the subdural collections were initiated at birth and persisted and became chronic, but there is no evidence for it. He was taken to the growth chart at [E120]:
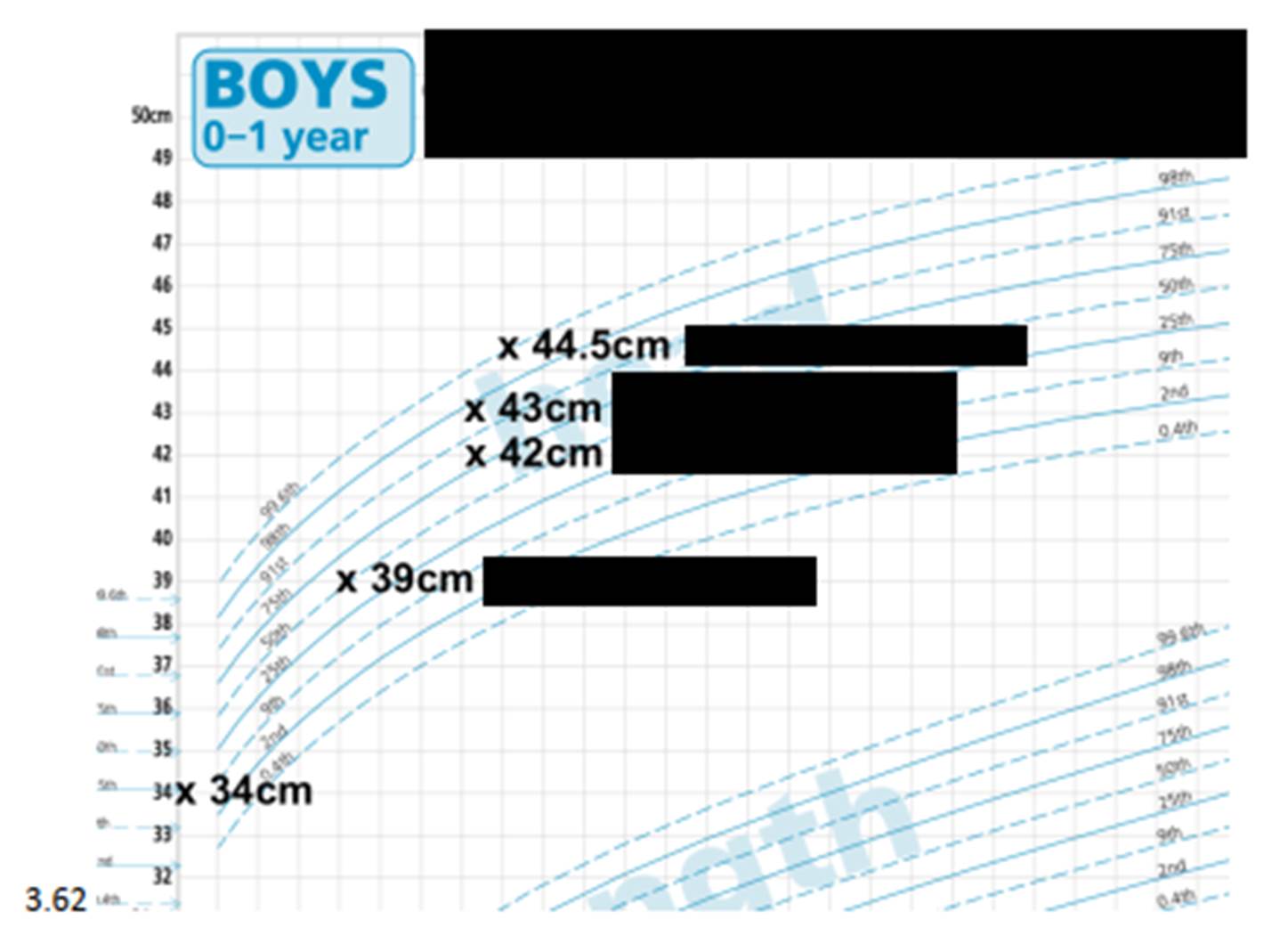
135.It was put to him that at 8 weeks head circumference had increased from the 25th centile at birth to the 50th centile and this “tells us chronic collections were on their way to developing”. He disagreed; he thought the rate of increase was more important and the increase post 8 week check was at a much greater rate, it was possible there was a slow increase from birth to 8 weeks and a more rapid increase thereafter as a result of the collections, but thought “it is more likely that is not the case”.
136.As with skull fracture, he considered ““bumping heads” would involve forces “too trivial to cause…subdural collections” [E124/4.25].
137.Mr Jalloh said that multi-focal collections would rarely be seen in household falls; “it would be rare, it’s not likely” and further, when the Hughes paper (Biomechanical characteristics of head injury from falls in children younger than 48 months, J Hughes et al. Archives of Disease in Children. 2016; 101: 310-315) [E217], was put to him he said:
My clinical experience and there are other publications indicate to me that infant falls from household falls from furniture or carer are common, sometimes produce a head injury and normally a skull fracture which is sometimes associated with a small amount of acute blood and this paper doesn’t do anything to change my understanding of that type of injury but that is different from large subdural chronic subdural that we see in this case, we don’t see focal injuries becoming multifocal chronic subdural.
138.He was also asked about the possibility of a fall from a carers arm producing sufficient acceleration and deceleration to cause subdural bleeding and a tear to the arachnoid membrane resulting in chronic subdural collections. He said that “kids rolling off changing tables or being dropped have skull fractures and small subdural bleeds, they do not come back with large subdural collections” and arachnoid tears causing large subdural collections are not observed. He later confirmed that a fall from a carer’s arms could cause “bilateral bleeds” (my understanding of that evidence is he was not retracting his earlier evidence that it would not be expected to cause large subdural collections of CSF from a tear to the arachnoid membrane).
139.In relation to possible cause he said:
[E124]
4.28 An episode of non-accidental injury involving rapid/repetitive acceleration-deceleration (i.e., shaking-type injury) is a possible cause of the subdural collections. Other evidence of a shaking-type injury such as retinal haemorrhages or rib fractures were not found but this does not reduce the likelihood of this mechanism.
…
4.31…An episode or episodes of non-accidental injury is the most likely cause.
[E125]
4.33…Normal handling and minor domestic accidents would not be expected to cause any injury at all.
[E128/4.51]
The level of force would be significant, greater than that encountered through every day or even accidentally rough handling, typically associated with a loss of control by the caregiver.
140.Dr Cartlidge considered a number of alternative causes of the injury and ruled them out (malformation, bacterial infections, coagulation disorder, Glutaric aciduria (widening of the subdural space), Ehlers Danlos syndrome, enlargement of the subarachnoid space and perinatal or birth injury) [E195-E199].
141.He was cross-examined on the issue of birth trauma and thought it “highly unlikely” the subdural collections originate from birth; Wrigley’s forceps were used but “they’re usually just a lift out, cradling the head, it’s not a traumatic situation and subdural bleeding is very uncommon after caesarean so the starting point is it is uncommon and I ask how can it remain so silent and then appear at [around 100] days of age and that seems very unlikely”. So he cannot date the injury to birth, notwithstanding the lesser confidence in his 3 week window.
142.As above, he considered FC’s explanation unlikely because it would be unlikely to generate sufficient force for multi-location subdural bleeding [E199]. By contrast he considered “Shaking the child and/or hitting the child’s head on a firm object leads to marked acceleration-deceleration forces that rupture these engorged veins, resulting in subdural bleeding.” [E200]. He considered the relevance of the absence of retinal haemorrhages reporting them to be “absent in about 20% of infants with an inflicted head injury” and less common in impact only events [E200]. He was not able to identify the force required, save to say “in my opinion the force needed would have been obviously excessive to a normally competent and responsible person.” [E201].
143.Dr Cartlidge also assessed the likelihood of the skull fractures and intra-cranial injury being sustained in the same incident:
[E201]
• I think that an impact sufficient to cause the probable skull fractures could have also caused at least some of the subdural bleeding. Yet, there was subdural bleeding at multiple sites, some of which were distant to the fractures. These are features more commonly associated with a shaking mechanism than with impact alone.
• Shaking and an impact could have been aspects of a single causal mechanism, for example if CC was shaken and his head hit an unyielding object during the same action.
144.My conclusion is that birth trauma is possible but unlikely. I particularly rely on Dr Oates’ evidence that it would be vanishingly rare to see chronic subdural haematoma at 3 months which originated from birth and Mr Jalloh’s consistent analysis of the head circumference data. A fall from a carer’s arms is a possible cause but unlikely to cause the multi-focal subdural collections (Dr Oates and Mr Jalloh) or large subdural collections (Mr Jalloh) which are seen in CC. A single impact injury (as from a fall) would be unlikely to cause them and would be atypical (Dr Oates and Mr Jalloh). The absence of other injuries does not reduce the likelihood of a shaking mechanism (Dr Cartlidge). That leaves 2 alternatives: a shaking event and an impact event or a single impact event but with greater force than would be expected from a carer’s arms (Dr Oates’ evidence it would require “a very significant impact injury” and Mr Jalloh’s evidence that it would need to be “of sufficient force/energy to cause significant inertial acceleration-deceleration of the brain”).
Group 7: Perpetrators
General Observations M
145.When cross-examined M accepted that from early February she had breathing difficulties; she was “pretty exhausted” but she denied CA was right when he told the police she would get angry and irritated. The full context of that comment is important; it came in the first pre-interview assessment of CA on 9 March 2024 (my emphasis):
[O421]
In regards to his mum he said that she is a fun and caring person who is really easy to talk to and they can talk for hours easily about anything. The best thing about his mum is her cooking and her roast dinners are the best especially her potatoes. What he likes the least is that she gets angry and irritate recently trying to manage the three children and the baby being sick, but he said nothing of concern other then she will shout at them. [sic]
146.However, she did agree that she tends to bottle things up when she has stress and problems (she had said as much in a text message to FC on 6 January 2024 [Z254]). She agreed “I just end up letting all my feelings out in one go” and agreed she was low in mood from CC’s birth “until FC had gone from the picture” which was after CC’s admission to hospital. She agreed that left her feeling isolated and caused her stress but did not agree it made her feel less able to cope.
147.A line of questioning was pursued based on a note in the police summary of text messages:
[O551]
Conversations with Paternal Grandmother discussing lack of support from FC, Feeling low, lonely and isolated due to not working, stating her job kept her distracted from 'nasty thoughts' and suggestions of how to work through these feelings.
148.She said she could not remember what the “nasty thoughts were”, but when pressed said “nasty thoughts of being alone, nothing sinister…not nice to be alone when you should have support around”; they were not thoughts of harming herself or others. I asked her why she appeared so sure when initially she said she could not remember what the nasty thoughts were; she did not initially answer the question but did say they were not “really bad, just everyday life, cut off, I’d lost a friendship due to relationship with FC and I had these horrible thoughts I’ve got nobody now and stuck in this relationship without my best friend and no support to help me”. When I asked her directly if it was a case of not remembering or finding it difficult to articulate what the thoughts were, she agreed it was the latter and when challenged on that said “I haven’t done this [giving evidence] before” and felt like questions were being fired at her. I make no criticism of counsel for FC who was properly cross-examining, but do acknowledge that may have felt challenging.
149.FC accepted M was “patient and loving with CC”; he told the police she was “perfect with the baby” and “amazing” [O205].
150.The GP attendance note for 8 March 2024 records M as “concerned”, “worried” and “genuinely worried” and querying the previous diagnoses of allergy or viral illness. Attendance at the GP with that presentation does not fit someone who had inflicted the injury that was the possible cause of CC’s illness.
General Observations FC
151.I remind myself I am entitled to take account of lies told by FC. I have set these out above. I ask myself if they are deliberate untruths or arise from mistake or confusion. FC’s admissions to the effect they are lies is sufficient to be satisfied they are lies not mistakes.
152.I ask if they relate to a significant issue. Where FC lives does not, although it was somewhat curious. His lack of recollection of someone who it turned out was the ex-partner of a person FC tried to arrange to have intercourse with the day after CC was admitted to hospital might have been from embarrassment about his behaviour. His lies about alcohol and drug use did not appear to have an innocent explanation. He has tested positive for cocaine use and chronic excessive alcohol use; he had admitted the same at least to some degree. It cannot be from embarrassment that he lied about his consumption of alcohol in the home. The lies point towards an attempt to conceal the truth about what happened at home when he was in sole charge of the children. His evidence about domestic abuse and criminal damage may have been a genuine lack of recollection, although this is really quite difficult to accept given the proximity of these incidents in 2022 and 2024, and it seems more likely an attempt to conceal his violent behaviour and perhaps that he gets angry.
153.When M gave evidence she spoke of CC not settling “that well with FC, if he was crying and FC tried to settle him there wasn’t a lot of patience there, it was very short lived”. She had told the police that “I think he also gets a bit jealous that CC has a better bond with me than he does with FC” [O50]. When cross-examined she agreed with the Local Authority that he was someone much louder than her who finds it difficult to accept he has done something wrong and who in some cases tries to blame other people. She said “he always put himself first…and didn’t understand you have to put the child first”. She agreed FC treated her house a bit like a hotel and when she went to hospital both at the beginning and end of February she was uneasy because “FC was not as experienced in raising children…he didn’t have the knowledge that I had”; but later she agreed that was not surprising given she was CC’s main carer.
154.However, when cross-examined, she agreed she picked up no signs that FC may hurt CC, she did not think he was a risk to CC and she accepted she told the police he was a good dad on 10 March 2024.
155.M referenced an incident when he had told her he was going to a friend’s flat after a funeral “but that wasn’t the case, he’d gone back out drinking” and said “he had lied, he was a liar”.
156.She said she felt unhappy in the relationship because of a lack of support from FC and “he has been” violent. She agreed it was a fair summary to say “he was quite overpowering, difficult to say no to him, used the house like a hotel, went his own way and did what he liked”.
157.When FC gave evidence he agreed that the day after CC was admitted to Hospital A on 8 March (and then transferred to Hospital B with the noted serious injuries) he had been “setting up some sort of liaison”, a sexual liaison, with a woman whose name he could not now recall. The attempt was by exchange of WhatsApp messages which are in the bundle. When asked to give an explanation for the apparent lack of concern for CC or M, he said he “must have had a drink that evening and I really can’t explain that” and in answer to my question he agreed it was “pretty much” a 24 hour drinking session. He later described it as a binge.
158.As noted above in relation to credibility, FC has a history of causing criminal damage. In cross-examination he admitted to sending a photo of himself to a former girlfriend holding a kitchen knife to his neck saying “he would not be here much longer” ([O142]). Whilst it was not his intention to threaten anyone he was drunk, he admitted the possibility of having “a pattern of abusive behaviour to partners” and said “when I drink I don’t know what I’m doing and become a lot more angrier” and agreed he would do things he would not ordinarily do. He said when he drinks “sometimes I can’t remember, sometimes happy, sometimes makes me angry”. He accepted that when he drinks he has a craving for cocaine - “when I’ve had quite a few beers”.
159.FC tested positive for cannabinoids possibly from environmental exposure in the approximate period November to December 2023. He tested positive for cocaine and its metabolites from November 2023 to March 2024. He admitted occasional use of cocaine pre-testing. As noted above in fact his consumption was much higher and his alcohol consumption could be up to 30 cans of lager per week, in cross-examination he said:
Drink would fuel me up and cocaine level up
Drink would make me feel angry
Cocaine levelled me out
160.He said he was under stress after CC’s birth, trying to find work (until 19 February 2024) but still had financial problems thereafter, he could not support his drug habit, he felt guilty for not doing enough to help and support M and “couldn’t find a way to step up”. He accepted he did not have the same bond with CC as M, he lacked patience when CC was crying, he found it difficult to settle CC at times, he was worried CC had a preference for M, he could not find it within himself to commit the time and effort to spend time with CC, care for him, feed him, change his nappies and that was “awful” and it caused him to feel really down, more upset and sometimes caused his alcohol and cocaine abuse to get worse.
161.On 18 March 2024 M told the police that on 8 March when FC was at hospital she “overheard FC saying to [Maternal Grandfather] that “she’s trying to say that I shook him”” [O449], the importance being that the possibility of a shaking injury had not been raised by medical staff or M. Whilst FC said that M was not lying about that, he could not remember because he was too drunk. I have already noted above this seems rather unlikely given the BWV taken not long after. An alternative explanation is that FC is fabricating his lack of recollection as a convenient way of avoiding an admission.
162.In cross-examination FC accepted (in relation to the incident that CA and CB reported) that he lied because he did not want the court to know he had behaved in a reckless fashion to protect himself and his own interests and to avoid looking like someone who behaves dangerously around children.
General Observations CA and CB
163.In cross-examination FC accepted he had never seen CA or CB “do anything worrying to CC”. He was so unconcerned about CC in their care that on one occasion, when M was in hospital on one of the two occasions, he left CC with CA and CB whilst he went to a local shop for food.
164.He now does not seek to blame CA and CB saying “they are blameless and should be exonerated”. There is no evidence at all of an incident whilst CC was either alone with CA, CB or both of them together.
Specific Incidents
1-6 February 2024
165.In the pre-interview assessment of CA on 9 March 2024 he is reported to have said (my emphasis):
[O422]
He was also asked if he could think of anything recently which made have made CC and his head poorly and the only thing he could think of was a few days ago he picked him up and CC’s head flopped back a bit CC kept smiling and gurgling like he always does. He could not think of anything else.
166.In the pre-interview assessment of CB on 9 March 2024 she is reported to have said:
[O421]
When asked directly about how CC might have hurt his head, she said she didn't know and that maybe he was born with it.
167.In her amended statement M said:
[C115/40]
Whilst I was at Hospital A I spoke to my children and asked them to have a think if anything might have happened to CC when I was in hospital. My son CA said to me that when I was in hospital FC was drunk at home and picked CC up from his swing chair and he had gone into the bedroom with CC and CA and CB both heard a loud bang and they heard FC saying, “Oh fuck”.
168.When cross-examined she gave further detail. The initial allegation was made by CA in the course of a phone call on 16 March 2024, CB was present but “just agreed with what CA was saying”. As far as she could remember, it was only discussed once more, on 17 March 2024 in the course of a car journey home to collect some supplies for hospital. When asked if CA and CB had made up the allegation to help her, she said “I don’t see how that’s possible as I called CA and he was put on the spot and asked outright if anything happened”. I infer she meant he would not have had time to make it up.
169.In the records from Hospital A there is the following entry written in retrospect on 16 March 2024 but apparently from 16.00 that day:
16.00 - while doing observations on CC. Mum wanted to speak privately away from CC and support worker to talk about recent events. Mum said her two children (older children) informed her of what biological dad has done when Baby CC was 9/10 weeks. Dad and 2 kids initially in living room together, dad went into bedroom. 2 kids heard loud bang and f**k after from dad. During this time mum was in hospital 5 day admission. Mum thinks head injury resulted from this incident…
170.The police log records a conversation with M on 16 March 2024 (my emphasis):
[O447]
Mum arranged to go home from Hospital A in order to collect some new clean clothes and then return to hospital, where CC is an inpatient. Around this time, CA (her eldest son) decided to update Mum and tell her some further information that he had not previously disclosed to her…
CA made the following disclosure to Mum. He stated that whilst Mum was previously in hospital with Pneumonia, FC (Mum’s boyfriend) had been drinking. He picked up CC and took CC into Mum’s Bedroom. CA and CB then heard a very loud bang, after they heard FC say “Oh fuck”. CA described the bang as sounding like a wall bang according to Mum. CB also heard the bang.
CB was present when CA was making this new disclosure to Mum. Both CA and CB apologised to Mum for not telling her the truth earlier and they both said that they thought FC was the cause of the injuries to CC. Mum told the children that in future that they needed to be truthful. CA told Mum that he had not made his disclosure to her as he did not want to get anyone into trouble.
CA confirmed that the incident took place during the 5 days when Mum was in hospital with pneumonia.
171.I note that this appears to date the described incident to the period of 5 days to 6 February 2024 when M says she was in Hospital A with breathing difficulties (M’s witness statement [C70/24]), rather than the 2 day period of 27-28 February 2024 when she was admitted (M’s witness statement [C70/26]).
172.There is an entry in the police log for 17 March 2024:
[O436]
Phonecall Received
Call Summary: STAFF MEMBER AT HOSP HAS BEEN TOLD THE FOLLOWING INFORMATION BY M. M ASKED THE CHILDREN HOW CC WAS HURT. CHILDREN HAVE TOLD HER THAT WHEN M WENT OUT THE CHILDREN WERE LEFT WITH FC. HE WAS DRUNK AND ON DRUGS. FC PICKED UP CC FROM THE ROCKING CHAIR, TOOK HIM INTO THE BEDROOM. THE CHILDREN HEARD A THUMP AND FC SHOUTING 'OH FUCK'
173.On 18 March 2024 the police log records a conversation with M:
[O442]
M disclosed that on Saturday 16th March 2024, whilst in the car driving on the way back from being picked up at hospital, her children CA and CB (but mainly CA) told her about an incident with FC and CC where they heard a loud noise and FC say 'OH FUCK'
174.In the pre-interview assessment of CA on 18 March 2024 he is reported to have said:
[O229] and [O440-O441]
CA stated that he heard a bang from FC and Mum's bedroom
He heard FC say "Ah. fuck".
He and his sibling CB were in The Front Room of their H/A.
The incident was at night time and he thinks over a weekend.
FC (Mum's boyfriend) was holding CC and then FC walked into Mum's bedroom with CC after picking CC out of her chair in The Living Room.
CA confirmed that FC was really drunk. He was slurring his words and his voice changes when he is drunk. He was stumbling slightly.
Mum mentioned that she didn't want to be with FC anymore.
The incident took place during the time that Mum…was in hospital with Pneumonia and Covid.
CA was unable to recall whether CC was crying or not as a result of the incident.
175.In pre-interview assessment of CB on 18 March 2024 she is reported to have said:
[O229] and [O441]
FC was drunk and he picked CC up and took him into Mum's bedroom.
Although CB did not see the incident, she commented that she thought that FC banged CC’s head owing to her hearing a loud bang. FC then said the "F" word.
CB described hearing a thud, which FC at some point told her was a head butt, but CB did not believe him.
CB could not be certain as to whether CB heard CC crying after the thud.
CB thought that she and her Brother thought the bang sound was near the wall or door in Mum's room.
At the time of the bang, she and CA were in the Front Room chilling.
She said "Be saw nothing" (referring to the actual cause of the bang).
The incident took place maybe 10 oclock ish at night on a Friday or Saturday.
176.There is a summary of a VRI with CB within the police log for 18 March 2024:
[O446]
CB said that she was on her phone on the sofa and CA was sitting on the floor playing GTA 5 on the playstation in the front room with CC who was in his little chair. It was about 10pm, which she knew as she had looked at her phone and it was sometime after 10pm. Mum’s boyfriend FC came to pick up CC but he was drunk. He picked up CC and walked out the room into mum and his room. Mum was in hospital at this time with pneumonia and covid, there was no one else in the house. She heard a loud bang, like a thump bang, and FC said ‘AH’ and then ‘said the F word’. When she heard the noise she said to CA ‘DID YOU HEAR THAT’ and CA said ‘YEAH I DID’, and that was all they said before FC came back into the room with CC approx. a minute after the bang. FC then put CC back in his crib in the front room.
When asked what happened when they came back into the front room she didn’t remember. She didn’t notice anything different about CC or see any injuries. CB said ‘WE CAN’T REMEMBER IF CC WAS CRYING AND ALL THAT’, and that she ‘THINK[S] CC MAY HAVE SMACKED HIS HEAD ON THE DOOR OR DROPPED DOWN AND FELL, BUT I DON’T KNOW’. When asked how long CC was back in the crib in the front room for or what else happened that night she said she didn’t know. When asked what FC did after putting CC back in his crib she said he just sat back down on his phone watching and playing a game, and they carried on for the night. He didn’t say anything about CC and she didn’t see him make any phone calls. FC seemed stressed and tired when he came back in the front room, she didn’t know why. They went to bed at around 11.
She didn’t know why FC picked up CC. She said FC normally lives with them. She demonstrated how FC picked up CC and when asked how tight he was holding CC she said ‘I THINK LOOSELY’. When asked how she knows FC took CC into the hallway and then mum’s bedroom she said ‘WE JUST KNOW THAT’S WHAT HAPPENED, WE’RE SMART, WE’RE DETECTIVES. WE DIDN’T SEE BUT WE KNOW WHAT MUM’S DOOR SOUNDS LIKE. I SAW FC’s FOOT GO INTO MUM’S ROOM’. She
said she was still in the living room but saw FC’s foot go into the bedroom. When asked how the front room door leading into the hallway was open or closed, CB said the door was open but he moved it a bit. She didn’t know why.
She said CC started puking after the bang, ‘MORE THAN USUAL AND BIGGER’, on the same night. She said FC cleaned the sick and ‘THAT’S ALL I KNOW’ and did not elaborate on this further.
When asked what she meant by FC being drunk she said ‘HE WAS DRINKING BEER’. She thought he was drinking a fosters beer, but then said she saw him drinking a grey or green can in the front room that wasn’t the fosters. She knew it was a beer as ‘I KNOW THAT HE DRINKS BEER ALL THE TIME’.
…
[O447]
…
CB mentioned an incident taking place before this that she wasn’t present for where CC flung his head backwards and so FC accidentally bumped heads with CC. She said ‘I DO BELIEVE THAT HAPPENED BUT I DON’T BELIEVE THAT’S WHAT GAVE CC A FRACTURED SKULL AND BRAIN BLEED’.
177.In cross-examination M agreed that appeared to be information she had got from an adult.
178.The police record continues:
[O447]
Following completion of both children's VRIs, when I was speaking with SW Vicky Tobutt who had been present in the waiting room throughout, Vicky said that after CB came out of her VRI
she said to Vicky in the waiting room "GRANDDAD TOLD ME WHAT HAPPENED AND THAT FC HURT CC". Vicky said she asked CB to expand on what she meant and CB said she didn't want to talk about it so they didn't speak about it further.
179.In cross-examination M said she asked CA about this and he said “it’s because that’s what we told grandad and he said make sure you tell the police”.
180.In his VRI CA variously said:
[U6]
21 CA: Er, so it was late at night, like, ten to 11, er, me and CB were in the front room
22 and FC, mum’s boyfriend, was drunk.
23 DC SL: Mm-hmm?
24 CA: Erm, he’s picked up CC out of his chair and then walked into their bedroom
25 which is then we heard, like, a loud bang, er, FC swear, and then he, erm, came
26 back, like, a few minutes later, came back with CC and put him back in the chair.
[U8]
9 CA: But when we heard the bang, FC said, “Oh, fuck,” [inaudible 00:08:32] when,
10 this is, like, when the bang happened, he said that.
181.He was asked about saying FC was drunk:
[U10]
7 CA: Er, well, he was, like, slurring slightly, like, his voice sounded a lot different than
8 what he sounds like when he’s sober—
9 DC SL: Mm-hmm?
10 CA: —and he stumbled slightly.
11 DC SL: Stumbled slightly?
12 CA: Yes.
13 DC SL: Okay, and what do you mean by “stumbling”?
14 CA: So when he was walking, he, like, kind of, you know, was, like, slightly swaying
15 a little bit.
182.In cross-examination FC agreed that CA and CB would “quite possibly” know what they were talking about in relation to his behaviour when he had been drinking. Certainly, what they report about slurring is consistent with FC’s report to police in interview that his voice changes after “one or two beers” [O79]. It is also consistent with his admission in interview that “it would be a few, few beers” he had in the period 1-6 February 2024.
183.Further on:
[U11]
12 DC SL: Why did he pick up CC?
13 CA: Erm, I think CC had just been sick a little bit so he was going to, like, go and
14 clean him in the bedroom and then that’s when he walked into Mum’s room.
15 DC SL: So he’d been sick a little bit?
16 CA: Yeah, I’m... I’m... I don’t exactly know.
…
28 CA: I think he either needed, like, his diaper changed or he was sick a little bit.
[U16]
13 DC SL: —and how... in terms of, roughly in terms of time, after he’s gone into the bedroom
14 with CC, FC, how soon was the bang?
15 CA: Like, a few seconds later.
16 DC SL: Mm, and what do you mean by “a bang”? I mean, a bang could mean lots of things
17 to different people, couldn’t it?
18 CA: It was, like, a wood... so I think it was, like, on the wooden floor [inaudible
19 00:19:27] wooden flooring in their room. It was, like, a wood... it was, like, a—
20 DC SL: Wooden flooring?
21 CA: Yeah, it was, like, a bang—
22 DC SL: Okay.
23 CA: —on that or something—
24 DC SL: Right.
25 CA: —if not the wall.
26 DC SL: Okay.
27 CA: [Inaudible 00:19:36] I think it was definitely the door though.
28 DC SL: Mm-hmm, but did you—
29 CA: Sorry, not the door, er, floor.
1 DC SL: Why do you think it was definitely the floor?
2 CA: It was, like, a wooden-type sounding bang and it was quite loud so—
3 DC SL: Okay, thank you, that’s helpful. You said that the bedroom’s got wooden floors?
4 CA: Yes.
5 DC SL: Okay, and after the bang, how many bangs were there?
6 CA: One.
7 DC SL: One bang?
8 CA: Yeah.
184.He described FC’s voice as “pretty loud” when he swore [U17], louder than normal [U18] and then:
[U18]
7 CA: Erm, he then... we... CB actually asked him what the... because
8 asked her to, erm, ask him what the bang was and he said that he
9 Mum because she wasn’t picking up but that’s all he told us.
[U19]
3 CA: —and then he said, “Oh, er, I was just trying to get hold of your mum and she
4 wasn’t answering the phone so I hit the wall.”
185.He later clarified he heard CB ask the question but did not hear FC’s response, he was told that by CB [U19-U20] and confirmed:
[U22]
11 CA: Erm, she said, “Oh, FC just said that he couldn’t get, he couldn’t get hold of
12 mum, she wasn’t picking up the phone so he just hit the wall.”
186.He said that FC was gone “maybe five to ten minutes” [U23], he did not notice anything unusual about CC when FC brought him back to the living room [U24-U25] and that this incident happened when M was in hospital with pneumonia and Covid for “between four and five days” [U26]. He thought it would have been on a Friday or Saturday as CA and CB’s bedtime is 9.30pm Sunday to Thursday and later on Friday and Saturday and this incident was between 10 and 11pm [U25-U26]. That would date the incident to 2 or 3 February 2024
187.He was asked why this information was not shared until 16 March 2024:
[U33]
24 DC SL: …All right, and what kind of prompted or, well… first
25 of all, about this, all this thud noise and what’s happened to CC on that night—
26 CA: Mm-hmm [nods].
27 DC SL: —who did you first tell about all that?
28 CA: Er, I’ve told my granddad first and my—
[U34]
10 DC SL: Mm, when did you tell [Maternal Grandfather]?
11 CA: Er, it was a night where I was at his house—
12 DC SL: Yes?
13 CA: —I don’t know exactly when but I was at his house and I told him about it.
14 DC SL: Yes, thank you for sharing that, and what did [Maternal Grandfather] say?
15 CA: Er, he said, he just agreed with me and said, “That’s probably what happened.”
16 DC SL: Right, [inaudible 00:45:30]—
17 CA: Like, that’s probably why CC’s in hospital because he thinks that FC, er,
18 maybe fell or dropped him.
19 DC SL: Mm-hmm, and why would [Maternal Grandfather] think that?
20 CA: Er, it’s because the doctors said that the injury on CC’s head was due to head
21 trauma—
22 DC SL: Right.
23 CA: —so that must be… so they said that was caused by a drop or something like that.
[U37]
9 DC SL: Mm-hmm, okay. So why didn’t you tell your mum straight away after the
10 incident?
11 CA: Er, I didn’t want to think that she thought... I didn’t want her to think that I was
12 lying and—
13 DC SL: Mm-hmm, why would she think that then, that you were lying?
14 CA: Because, er, we didn’t see it so of course she might just think that we’re trying to
15 lie and that maybe we did something like dropped him—
16 DC SL: Mm-hmm.
17 CA: —which we didn’t.
188.M was asked about CA’s reported concern that M may think he was lying, and she said she would not have blamed CA and CB; she agreed “his explanation for not telling anyone earlier does not add up”.
189.FC was re-interviewed on 18 March 2024. He said it was not “too bad” looking after the children when M was in hospital at the beginning of February [O72/15], he would drink 2-3 beers at home [O76/6] and when CA and CB’s allegation was put to him there was this exchange:
[O79]
12 DC KW: You have picked CC up—
13 FC: Mm-hmm.
14 DC KW: —and taken him into the bedroom—
15 FC: Okay.
16 DC KW: —and then they’ve heard a loud thud—
17 FC: Okay.
18 DC KW: —followed by hearing you shout, “Oh, fuck.”
19 FC: No, that definitely wouldn’t have happened. No, no.
[O80]
5 DC MC: Can you think of anything that may have happened that may have led to them
6 thinking like this or anything—
7 FC: I dunno, may-maybe something fell off the bed, like the controller, or something,
8 I don’t know, but, erm, there was no... there was no swearing and then me going
9 back into the front room, so other than that, I can’t think of anything, I’m afraid.
[O81]
2 DC KW: —but when they say a loud thud, can you think of anything that—
3 FC: I can’t, I’m afraid. No.
4 DC KW: —could have been?
5 FC: No. Like I said, unfortunately, I can’t.
6 DC KW: Okay. With saying, “Oh, fuck,” is that something that you would say? Like, do
7 you swear?
8 FC: No, no. No, that’s, that’s quite thrown me, actually.
190.In FC’s revised first statement he said:
[C76/2]
The only incident I am aware of is recounted in paragraph 1.11 whereupon CC jolted upwards unexpectedly, and we clashed heads. This was the only explanation I could put forward which might have caused his injuries, as the clash hurt my head.
[C76/3]
At paragraph 1.12, the information provided by CA and CB to their mother suggesting that CC’s injuries were caused by me is incorrect. They were both in my care as was CC for a period of five days when Mother was in Hospital with pneumonia in February of this year. I was not drinking heavily or intoxicated, CC was asleep in his baby rocker and he had done a poo, so I took him to his room and changed his nappy. I do not recall there being a very loud bang, it may have been that his bottle fell off the bed or one of his toys. I swore at the time because he had done a rather large poo, otherwise I don’t usually swear around the house. Nothing happened on that occasion to CC to cause his injuries.
191.I note that this is not consistent with FC’s second police interview on 18 March 2024 in which he denied a recollection of the account that CA gave generally at [O79-O80] in relation to the cause of a thud he could think of nothing [O81/3]; and in relation to swearing denied doing so to the extent that the allegation had “thrown” him [O81/6-8] although he did later say that he might have said “Oh, oh god” if CC had a “pooey nappy” [O87/7-9].
192.In cross-examination FC accepted CA did not seem to be motivated to tell lies about him and was not lying when he said “he had, like, a few beers, if not like a few dozen” [U11]. He said there may have been cocaine in the house although denied using any.
193.There are some important points to remember about CA and CB’s allegation:
a) CB was reported by M to have a bad temper and to have been jealous of CC;
b) There have been occasions when M has returned to a room because CC was crying and CB has been holding CC;
c) It was not reported at the time;
d) It was not reported when CC was admitted to hospital;
e) CA’s explanation for the delay (that M may have thought he was lying) “does not add up”;
f) In the second pre-interview assessment CB said FC told her the thud “was a head butt” [O441] but this was not CA’s account or an account given earlier by CB, and it differs from CA’s account of what CB told him what FC had said (that it was him hitting the wall [U19]);
g) After her VRI CB told the social worker “Grandad told me what happened and that FC hurt CC”; and
h) CB appears to have parroted what she was told by an adult in relation to the head clash incident [O447].
194.On the other hand:
a) The information appears not to have been prompted;
b) FC did not suggest CA was lying in his recollection;
c) M’s oral evidence was that there was no discussion in front of CA and CB about the cause of CC’s injuries prior to 16 March 2024;
d) M’s oral evidence was that she put CA “on the spot” in the call when the allegation was first made so there was no time to make something up;
e) FC does now accept there was an occasion when he took CC to his room, changed his nappy and swore [C76/3];
f) FC does now accept drinking at home and that slurring his words would be consistent with the quantity of alcohol he remembers drinking;
g) When cross-examined FC was unable to give an explanation for having lied to the police that there had not been such an occasion.
27-29 February 2024
195.As noted above, when M gave evidence, she said that she could date the time CC began to be unwell as after she went to hospital on 27 February 2024 and he was “sickly” in the early hours of 28 February. She said he was otherwise “a very easy baby, very content, very happy” In her statement she said:
[C113]
26. On 27th February 2024 I went to the GP was I was not feeling well. I had collected CB from school. FC and CC were also with me. I was seen by the GP and the GP said I had to go to the hospital. My dad took me to the hospital and FC was at home with all three children. He kept calling me and I could hear CC crying in the background, FC said CC had been crying and that he had been sick and had three diarrhoea nappies. I told FC to comfort CC and reassure him. I was in A&E at that time and there was a long wait.
27. I was discharged from Hospital A on 28th February 2024 at 4am. The hospital prescribed me with an inhaler, steroids and more antibiotics.
28. When I returned home CC was sleeping and when I saw him in the morning he was being sick. I also felt he was a lot more sleepy.
196.In her oral evidence she said that immediately prior to her leaving for hospital CC had been “a bit unsettled, he was given Calpol for teething and had been sick from having it”. She was challenged on this in cross-examination:
|
Q CC before you went into hospital CC was unsettled and sick A Yes Q Following day you returned home A Yes Q CC continued to be sick and seemed a bit more sleepy A Yes Q That seemed to be a continuation of how he seemed the previous day A I don’t recall CC being sleepy before I left for hospital though Q He might have been A No, it was unsettled and sick but not sleepy |
197.It follows that, although there was some similarity between pre and post-attendance by M at hospital, there was also a difference, and when asked about it in re-examination she said her impression was that on 27 February CC was teething “because his cheeks were red and he was dribbling and munching on his hands.”
198.In the phone downloads there is evidence of a message from FC to M at 18.59 on 27 February, “Still hasn’t stopped screaming x” and then calls (or perhaps missed calls) from FC to M at 23.28, 23.42, 23.55, 23.56 and 23.58 followed by a text from FC at 23.59, “Can you answer pls x” and “Or call x”. At 00.22 on 28 February M replied saying, “I’ll contact you soon Struggling with my breathing. x” and he replied at 00.33 “Ok but he keeps shitting n really screaming call me when you csn x”. When cross-examined he said he could not remember why he was calling; he thought it could be to check on M, although that is not consistent with the messages or the fact that he tried to call M even after she messaged saying she was struggling with her breathing, a call that was under 2 minutes later, and the message 10 minutes later saying “he keeps shitting”; it was not “how are you”.
199.In cross-examination he accepted it was quite possible he had been drinking and in written closing submissions accepted “he has no memory, through drink and possibly through drugs”. He agreed that when M left for hospital he was not worried about CC’s presentation and then there was a “screaming baby for hours, a material difference to how CC normally presents”.
200.It was put to him that he had shaken CC and hit his head and he said “I wouldn’t do that”, but he agreed drink and drugs make him do things he would not ordinarily do and behave without normal levels of control.
201.FC called 111 on 29 February 2024 (transcribed at [S1]); he told the operator “erm, the mother’s panicking. He, he’s been quite ill for the last couple of days. Er, we took him to the doctor’s and, erm, they believe it to just be, er, gastroenteritis.” M denies CC had been taken to the doctor immediately preceding this and there is no record of it (save for much earlier on 5 February 2024). FC also said, “He’s now just laying in his cot so obviously we’re, er, closely monitoring him” which M also denied in her evidence in chief saying CC was with her, in her arms and FC had gone outside to make the call.
202.In his first statement FC said:
[C77/11]
On 27th February - 28th February 2024 whilst Mother was in Hospital, I contacted her because I was concerned about CC as he had been crying for some time. Nothing happened, he settled and was fine the following day.
203.In his statement dated 14 October he said variously:
[Z54-Z55]
2. On 27 February 2024 I was concerned about CC as he was not keeping his milk down…
…
4. On 29th February 2024 when I came home from work, I gave CC his bottle feed after his bath. After that M sat next to him with me in the bedroom. He seemed absolutely fine apart from being grizzly which was due to him teething…put him in his cot in the bedroom. M was still in the room at the time and he went to sleep for a couple of hours. She later took him out of the cot and he started to be sick so she gave some more Calpol. He kept putting his hand in his mouth which we thought was because he was teething. I was in the kitchen or with the other two children in the front room at the time when I heard M say that CC had gone rigid after he’d been sick…
6. I had heard her call out in panic to me and I had already seen CC vaguely rigid when I came running into the room, then coming out of rigidness, so I decided to call 111 and I told them what we had both seen…
204.He agreed this was at variance with what he told police on 9 March 2024 [O204], and in the course of cross-examination agreed it was not correct to say CC slept for 2 hours, that he was in the kitchen, that M said CC had gone rigid, that he rushed through to the bedroom, and that M said she did not want to make the call to 111. He agreed he was trying to take the credit for wanting to call 111, when it was M who wanted to.
205.He agreed there were differences in what he told the police on 9 March 2024 and what was reported to the 111 operator on 29 February 2024. He told the police:
[O204]
Whilst on the phone CC became rigid. FC demonstrated this by holding his arms in the air. FC stated he could not get CC’s arms to go down and this lasted for 10-15 seconds. He was unable to do the checks they were asking him to do because his joints were so rigid. They tried lying him down and this did not change his pose. FC described feeling incredibly scared. He described this on the phone to 111 and they were advised to take CC to hospital.
206.None of that is captured in the 111 audio recording (in which I note FC seems incredibly relaxed). FC admitted in cross-examination that “quite possibly, yes” the “whole description is a pack of nonsense”.
207.In M’s discussion with the police on the same day there is the following recording:
[O417]
[CB] has become very jealous of CC as he is now the youngest in the family and she states CC get all the attention and he [sic] doesn’t like that cause she feels like she doesn’t get any. CB has also got a very bad temper and doesn’t seem to be a fan of CC…
208.In cross-examination M accepted that “she has returned to the room on a couple of times when CB held CC, due to hearing CC crying” (the Paternal Grandmother’s report to police [O489]). She agreed that CB “can be explosive at times” and that was primarily why she had sought an autism referral for her. In her VRI M said:
[O45]
28 DC AL: Is it that you’re suspecting something has happened between CB and CC?
29 JT: It’s possib-possible. She... I don’t want the blame on my daughter, but possibly
30 she might have tried picking him up and bumped his head but she may be too
31 scared to say anything because she’s probably scared that she’s gonna get in
32 trouble, which she wouldn’t, she wouldn’t be in trouble, but it is possible—
209.FC was interviewed on 11 March 2024. He mentioned CC kept being sick quite a lot [O5] “within the last week” [O11], an incident where he and CC clashed heads [O8] and he was asked about the time M was in hospital in early February 2024 and said his mother had come around a few times to help at home [O20], and there were no problems or issues whilst M was in hospital [O21].
210.It was put to FC in cross-examination that whilst in hospital on 8 March 2024 on a couple of occasions FC made it look like he was the one pushing for medical attention for CC when that was not true. He agreed. He admitted he had lied about being the one who wanted to call 111 on 29 February 2024, but he could give not an explanation for it. He admitted he lied in his witness statement in saying that M was in a room alone with CC before the incident of rigidity on 29 February 2024, but could give no explanation for it. it was put to him it was to make the judge think M had done something to CC which he denied.
Analysis
211.No-one invites a finding that the injuries were caused by CA or CB and aside from occasionally being alone with CC there is no evidence to suggest he sustained injuries in their care.
212.No-one invites a finding that the injuries were caused by M. CC was unwell whilst generally, at least, in her care but there is evidence of her seeking appropriate medical attention and of a loving relationship with CC. I am satisfied on the balance of probabilities that FC must have caused the injuries on around 27 February 2024.
213.My reasons for this finding are FC’s admissions, the change in CC’s symptoms between 27 and 28 February 2024, the consistency of that timing with the expert medical evidence and the evidence of a biphasic presentation (an acute response of crying and a chronic response of gradual unwellness). I have considered whether FC may have been responsible for injuring CC at the time he is reported by CA and CB to have sworn in the period 1-6 February 2024, but there is no evidence of a biphasic presentation, and the dating of the subdural collections by the medical experts does not fit.
214.FC invites me to find that the cause of injury on 27 February 2024 was due to a culpable accident (i.e. whilst under the influence of alcohol and possibly drugs) and that it was a single incident. Whilst the Local Authority do not seek a finding as between culpable accident and infliction of injury, M does and I am entitled to consider the matter. If infliction is a conclusion that can be reached on the balance of probability, I am entitled to make that finding and CC is entitled to know that.
215.Mr Goodwin KC for FC reminds me that a propensity to inflict injuries does not necessarily map on to a propensity to inflict them on children. I do not derive much assistance from the admissions of 2 previous incidents of criminal damage or the allegations of domestic abuse against a former partner. Allegations of domestic abuse by FC against M were not pursued.
216.Mr Goodwin KC reminded me that the collection of injuries could have arisen from a single impact which would be consistent with an accidental drop but that is equally consistent with a deliberate impact. I consider this is a neutral piece of evidence.
217.Counsel also submitted that the medical evidence did not demonstrate metaphyseal fractures, retinal haemorrhage etc suggestive of a separate shaking incident militating against an inflicted injury, but Dr Cartlidge’s evidence was that it did not reduce the likelihood of this mechanism. It also does not rule out a single inflicted injury causing both skull fractures and intra-cranial injury.
218.FC said he would not have hurt CC.
219.Against these points I must weigh the following evidence:
a) FC’s extensive dishonesty set out above and which in significant respects is not explicable, save for him covering for his own misdemeanour: his lies about how much he drank in the home and with the children present;
b) His evidence that he becomes dysregulated, including angry, when in drink such that he would do things he would not ordinarily do and behave without normal levels of control;
c) His acceptance that he lacked patience when CC was crying;
d) His evidence that he was upset by the relatively poorer bond he had with CC than M had;
e) His evidence that the upset about that bond sometimes caused his alcohol abuse to get worse;
f) The reported comment about M trying to blame him for shaking CC when the same had not by then been raised by the hospital, coupled with FC’s evidence that he could not remember because he was too drunk, when in fact just over an hour later the BWV appeared to show him sober and lucid;
g) His admission that, in relation to the incident in early February reported by CA and CB, he had lied to protect himself and his own interests;
h) His willingness to lie at hospital and in his witness statement to make it appear he was the one pushing for medical attention and that there was a time when M was in the room alone with CC before he went rigid on 29 February 2024; and
i) As counsel for the Mother put it, the invitation to find a culpable accident “does not sit well with…the preponderance of the expert evidence”.
220.This last consideration requires a little more analysis:
221.Dr Oates considered a skull fracture could occur from as low as 50 cm but that was not the norm, and skull fracture would be compatible but unusual in a fall from a carer’s arms. Mr Jalloh considered such a fall could cause a skull fracture. Dr Oates considered multi-focal collections from low level falls were “in the unusual box”. Mr Jalloh said it was rare and not likely, “kids falling off changing tables or being dropped have skull fractures and small subdural bleeds”, not large subdural collections from arachnoid tears.
222.I am driven to the conclusion that, on the balance of probabilities, an accidental fall whilst in FC’s care is much less likely than an inflicted injury, one which FC has sought to cover by reliance on a lack of memory of the event.
223.I conclude that CC suffered 2 skull fractures to the right parietal bone and an intracranial injury later manifesting in chronic subdural collections whilst in the care of FC on 27 February 2024. There was either a single impact with greater force than would be occasioned by an accidental fall from a carer’s arms or 2 separate incidents of shaking and impact. On the evidence I cannot say one is more likely than the other. If it were a single impact, that was a deliberate act and it required greater force than an accidental drop from a carer’s arms. If it were a combination of shaking and an impact, the impact may have been accidental (such as by dropping CC) but the shaking could not have been; it was deliberate.
224.Ms Howe KC for M highlighted the impact of this on CC in her closing submissions:
CC has lost vital months of maternal care during the most critical period for the development of his attachments. He may have incurred permanent emotional harm as a consequence. This is all because FC was too cowardly to own his behaviours and accept responsibility for what he did to CC, preferring instead to point a finger at M and keeping silent for months to protect himself. What FC has done is unforgiveable…
225.I agree. FC has inflicted significant harm on CC: through physical injury and emotionally through persisting in denying responsibility for his actions which has led to the separation of CC from M. And all this when his ultimate position was that he admitted causing the physical injuries through culpable accident, albeit I have gone further to find he inflicted them. FC has engaged in a deliberate and cynical attempt to conceal the true facts and has, at almost every turn, sought to evade and minimise his responsibility.
Group 8: Observers
226.Mr Jalloh’s evidence was:
[E126]
An impact that causes a skull fracture is painful and associated with an immediate change in behaviour such as crying, irritability, or appearing stunned.
227.Dr Cartlidge’s evidence was:
[E187]
The skull fractures would have been initially very painful, typically for about 10 minutes (unless CC was rendered unconscious by the causal event)
[E193]
Skull fractures would have been painful. In my opinion, any person witnessing the causal event(s) would have realised that CC had been hurt.
228.I conclude that the skull fractures would initially have been very painful for around 10 minutes and an observer of the causative event would have known CC had been hurt. I conclude FC was aware CC had been hurt; that was why he was repeatedly messaging M. I conclude that M could not have been aware of the seriousness of the injury thereafter but would have been, and was, aware CC was unwell.
Threshold
229.In light of the findings there can be no doubt that the section 31(2) threshold is crossed.
